Narcolepsy, an enigmatic sleep disorder, is often accompanied by a myriad of perplexing symptoms that can disrupt both the personal and professional lives of those affected. From excessive daytime sleepiness to vivid hallucinations and sudden loss of muscle control, narcolepsy poses numerous challenges to those who experience it. Despite its prevalence, narcolepsy remains relatively mysterious, but with a better understanding of its symptoms, causes, and available treatments, individuals living with this condition can find relief and regain control over their daily routines. In this comprehensive guide, we unravel the intricacies of narcolepsy, exploring its symptoms, potential causes, diagnosis methods, treatment options, and coping strategies. Additionally, we delve into the latest advancements in research to shed light on this puzzling disorder and offer hope for a brighter future for those affected by narcolepsy.
What is Narcolepsy?

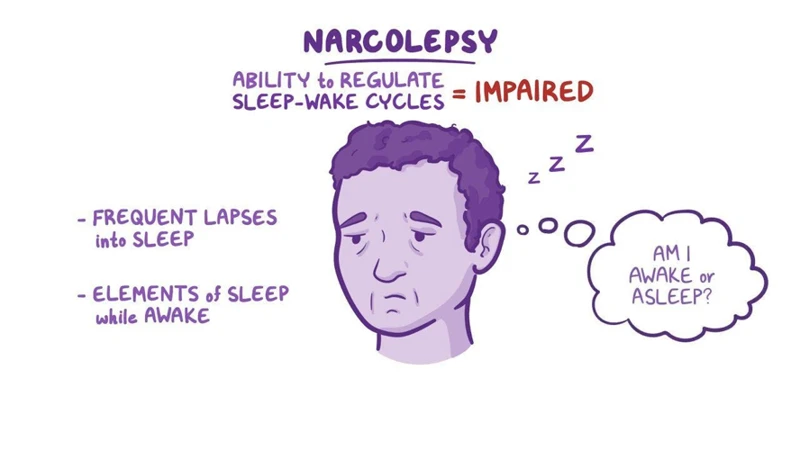
Narcolepsy is a neurological disorder characterized by the brain’s inability to regulate sleep-wake cycles properly. This leads to significant disruptions in sleep patterns and a range of challenging symptoms. One of the hallmark features of narcolepsy is excessive daytime sleepiness (EDS), where individuals experience an overwhelming and persistent urge to sleep throughout the day, regardless of how much sleep they have had at night. This intense sleepiness can make it difficult to concentrate, stay alert, and perform daily activities. Another distinct symptom of narcolepsy (narcolepsy) is cataplexy, a sudden loss of muscle control triggered by strong emotions such as laughter, surprise, or anger. During a cataplexy episode, individuals may experience mild muscle weakness or a complete collapse, which can be quite distressing. Sleep paralysis (sleep paralysis) is another perplexing symptom of narcolepsy, during which people are temporarily unable to move or speak while transitioning between sleep and wakefulness. This can be a terrifying experience as individuals may also hallucinate vividly during these episodes. Speaking of hallucinations, narcolepsy can cause hallucinations (hallucinations) that occur just before falling asleep or upon waking up. These hallucinations can be visual, auditory, or even tactile, adding to the already disorienting nature of the disorder. Lastly, individuals with narcolepsy often experience fragmented sleep, meaning that their nighttime sleep is frequently disrupted by frequent awakenings and brief periods of wakefulness. This can lead to a feeling of unrested sleep and daytime fatigue. By understanding the symptoms associated with narcolepsy, individuals can seek appropriate medical intervention and management strategies to effectively cope with this complex disorder.
Symptoms of Narcolepsy
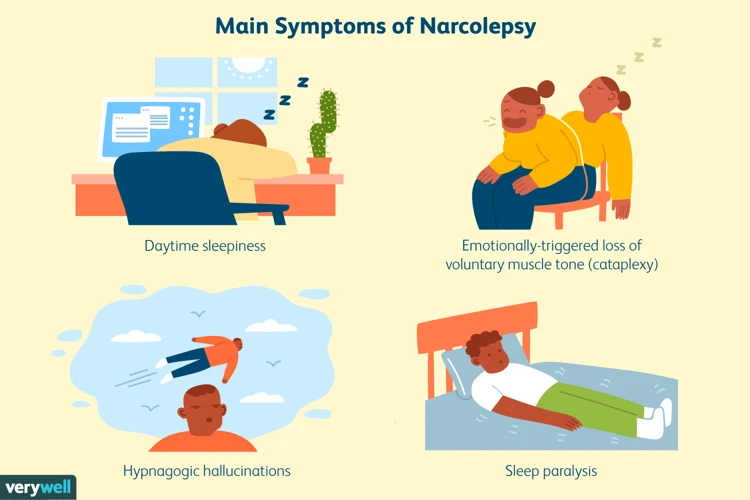
Narcolepsy manifests through various symptoms that can significantly impact an individual’s daily life. One prominent symptom is excessive daytime sleepiness (EDS), causing an overwhelming and persistent urge to sleep during the day, regardless of prior sleep duration. This constant sleepiness can lead to difficulty concentrating, staying attentive, and undertaking daily activities. Cataplexy, another classic symptom (cataplexy), involves sudden loss of muscle control triggered by emotional states such as laughter, surprise, or anger. Individuals experience a range of manifestations during cataplexy episodes, from mild muscle weakness to complete collapse. Additionally, narcolepsy can entail sleep paralysis (sleep paralysis), during which individuals temporarily cannot move or speak while transitioning between sleep and wakefulness. This can be accompanied by vivid hallucinations, further intensifying the distressing nature of the disorder. Individuals may experience hallucinations (hallucinations) just before falling asleep or upon waking up. These hallucinations can be visual, auditory, or tactile, further adding to the disorienting nature of narcolepsy. Lastly, fragmented sleep is a common symptom, characterized by disrupted nighttime sleep due to frequent awakenings and brief periods of wakefulness. It can result in feelings of unrested sleep and daytime fatigue. Recognizing and understanding these symptoms is crucial for individuals to seek appropriate medical evaluation (medical evaluation) and develop effective coping strategies to manage narcolepsy successfully.
Excessive Daytime Sleepiness
Excessive daytime sleepiness (EDS) is one of the primary symptoms experienced by individuals with narcolepsy. It is characterized by an overwhelming and constant urge to sleep during the daytime, regardless of the amount of sleep obtained the night before. This persistent sleepiness can have a significant impact on daily activities and overall quality of life. Those with EDS may struggle to stay awake and alert, leading to decreased productivity at work or school, difficulty concentrating, and a higher risk of accidents or errors. EDS can manifest as extreme fatigue, drowsiness, and the irresistible urge to nap throughout the day. Individuals may find themselves nodding off in inappropriate situations or locations, such as during a meeting, while driving, or even during conversations. The severity of EDS can vary among individuals with narcolepsy, and it often persists despite getting an adequate amount of nighttime sleep. It is crucial for individuals experiencing EDS to consult a healthcare professional for a proper diagnosis and appropriate management strategies. Treatment options may include medications to promote wakefulness, lifestyle modifications, and developing strategies to manage fatigue effectively. By addressing excessive daytime sleepiness, individuals with narcolepsy can regain control over their daily routines and improve their overall well-being.
Cataplexy
Cataplexy is a unique symptom of narcolepsy (cataplexy) that involves a sudden loss of muscle control and tone. It is often triggered by intense emotions, such as laughter, surprise, or anger. Individuals with narcolepsy may experience varying degrees of cataplexy, ranging from mild muscle weakness to a complete collapse. The duration of a cataplexy episode can also vary, lasting anywhere from a few seconds to several minutes. During an episode, individuals remain fully conscious but are unable to move or speak. It is important to note that cataplexy is not directly linked to the amount of fatigue or sleepiness a person is experiencing, which means it can occur even when the individual is well-rested. The experience of cataplexy can cause significant distress and interfere with daily activities, leading to potential challenges in both personal and professional life. Understanding and recognizing cataplexy is crucial for individuals with narcolepsy to seek appropriate support and management strategies, which may include medications, lifestyle adjustments, and therapy.
Sleep Paralysis
Sleep paralysis (sleep paralysis) is a fascinating yet unsettling phenomenon that can occur in individuals with narcolepsy. It is characterized by a temporary inability to move or speak while transitioning between sleep and wakefulness. Typically, sleep paralysis occurs either when falling asleep or when waking up, leaving individuals in a state of temporary immobilization. During episodes of sleep paralysis, individuals may also experience hallucinations, intensifying the already perplexing nature of this phenomenon. These hallucinations can take various forms, such as seeing shadowy figures, feeling a presence in the room, or hearing strange noises. The combination of being unable to move and experiencing vivid hallucinations can be terrifying for those who encounter sleep paralysis. The exact cause of sleep paralysis is not fully understood, but it is believed to be linked to disruptions in the rapid eye movement (REM) sleep phase. During REM sleep, dreaming occurs, and the body is naturally immobile to prevent acting out dreams. However, in sleep paralysis, this immobilization persists beyond the usual REM sleep period, creating a temporary state of muscle paralysis. While sleep paralysis can be a distressing experience, there are coping strategies and techniques that can help manage and reduce the frequency of episodes. These may include practicing good sleep hygiene, managing stress levels, and maintaining a regular sleep schedule. Additionally, seeking professional help from a healthcare provider familiar with sleep disorders (sleep paralysis causes, symptoms, coping strategies) can provide valuable insight and guidance for managing sleep paralysis effectively.
Hallucinations
Hallucinations are a puzzling symptom experienced by individuals with narcolepsy. These hallucinations (hallucinations) can occur during a state of wakefulness, known as hypnagogic hallucinations, or upon awakening, known as hypnopompic hallucinations. These vivid sensory experiences can manifest in various forms, including visual, auditory, and tactile sensations. Visual hallucinations may involve seeing people, animals, or objects that are not actually present. These images can be incredibly lifelike and indistinguishable from reality, causing confusion and distress. Auditory hallucinations, on the other hand, involve hearing sounds, voices, or music that others cannot perceive, further adding to the disorienting nature of the hallucinations. Some individuals may also experience tactile hallucinations, which involve sensations of being touched, such as feeling a hand on the shoulder or insects crawling on the skin. It is important to note that these hallucinations are not indicative of mental illness, but rather a result of disruptions in the sleep-wake cycle. They can be triggered by moments of fatigue or during the transitions between sleep stages. Hallucinations can contribute to the overall sense of confusion and uncertainty that individuals with narcolepsy experience. Managing hallucinations often involves implementing strategies to improve sleep hygiene and addressing any underlying sleep disorders. If hallucinations occur during episodes of sleep paralysis, understanding the link between the two phenomena can provide valuable insights for managing and coping with both experiences.
Fragmented Sleep
Fragmented sleep is a common symptom experienced by individuals with narcolepsy (narcolepsy). It refers to the disturbance of normal sleep patterns, characterized by frequent awakenings and interruptions throughout the night. This fragmented sleep can be attributed to various factors associated with narcolepsy, such as sudden muscle weakness during cataplexy episodes or the rapid onset of REM sleep. REM sleep, also known as rapid eye movement sleep, is the stage of sleep where dreaming occurs and is typically associated with muscle paralysis to prevent acting out dreams. However, in narcolepsy, the transition into REM sleep can be abrupt and occur throughout the sleep cycle, leading to disrupted sleep patterns. These interruptions not only result in a feeling of unrested sleep but also contribute to excessive daytime sleepiness (EDS), a hallmark symptom of narcolepsy. The lack of consolidated, quality sleep during the night can make it challenging for individuals with narcolepsy to stay awake and alert during the day, impacting their overall functioning and quality of life. Addressing fragmented sleep is an essential aspect of managing narcolepsy, and individuals should work closely with healthcare professionals to develop strategies aimed at improving sleep continuity and reducing daytime sleepiness. These strategies may include maintaining a consistent sleep schedule, creating a conducive sleep environment, and practicing relaxation techniques to promote better sleep. By prioritizing strategies to address fragmented sleep, individuals with narcolepsy can strive for improved overall sleep quality and better manage their daytime symptoms.
Causes of Narcolepsy

The causes of narcolepsy (narcolepsy causes) are not yet fully understood, but researchers have made significant progress in unraveling its origins. One of the primary factors believed to contribute to narcolepsy is a deficiency in a neuropeptide known as hypocretin or orexin. Hypocretin plays a crucial role in regulating sleep-wake cycles and promoting wakefulness. In individuals with narcolepsy, there is a significant reduction in hypocretin production or a loss of hypocretin-producing neurons in the brain. This deficiency is thought to be primarily due to an autoimmune response, where the body’s immune system mistakenly attacks and destroys these particular cells. The exact trigger for this autoimmune response remains unclear, but genetic factors (genetic factors) are believed to play a role. Certain genes, such as the HLA-DQB1*06:02 allele, have been associated with an increased susceptibility to narcolepsy. Additionally, external factors such as viral infections (viral infections) or hormonal changes during puberty (hormonal changes during puberty) may contribute to the development of narcolepsy in genetically predisposed individuals. Narcolepsy is believed to be a complex interplay between genetic susceptibility, autoimmune responses, and environmental factors. Understanding the underlying causes of narcolepsy is crucial for improving treatment options and developing preventive measures to mitigate the impact of this sleep disorder.
Diagnosis

Diagnosing narcolepsy can be a complex process that requires a comprehensive evaluation of an individual’s symptoms, medical history, and sleep patterns. Since narcolepsy shares some similarities with other sleep disorders, it is crucial to differentiate it from conditions such as sleep apnea, insomnia, and restless legs syndrome. To begin the diagnostic process, a healthcare professional will typically conduct a thorough physical examination and review the patient’s medical history. (Diagnosis) They may inquire about the frequency and severity of symptoms like excessive daytime sleepiness, cataplexy, sleep paralysis, hallucinations, and fragmented sleep. The specialist may also ask the individual to keep a sleep diary or wear a portable monitoring device to track sleep patterns and any abnormal behaviors during sleep. In order to confirm the diagnosis of narcolepsy, two key tests are commonly used. The first is a Multiple Sleep Latency Test (MSLT), which measures how quickly an individual falls asleep during daytime naps and assesses their tendency to enter rapid eye movement (REM) sleep. The second test, called a Polysomnogram (PSG), monitors brain activity, eye movements, heart rate, and muscle activity during an individual’s overnight sleep. These diagnostic tools help identify specific sleep abnormalities associated with narcolepsy. While the process may take time, an accurate diagnosis is essential for implementing appropriate treatment strategies and improving overall quality of life for individuals with narcolepsy./relationship-sleep-disorders-chronic-fatigue/
Treatment Options
When it comes to treating narcolepsy, there are various options available to help individuals manage their symptoms and improve their overall quality of life. Treatment approaches may involve a combination of lifestyle changes, medications, therapy, and even alternative treatments. Lifestyle changes (lifestyle changes) can play a significant role in managing narcolepsy. Establishing a consistent sleep schedule and practicing good sleep hygiene can help regulate sleep patterns and reduce the impact of excessive daytime sleepiness. Additionally, avoiding stimulants like caffeine and alcohol close to bedtime can promote better sleep quality. Medications (medications) prescribed by healthcare professionals, such as stimulants and antidepressants, can help alleviate symptoms, promote wakefulness, and manage cataplexy. Therapy (therapy), such as cognitive-behavioral therapy, can assist individuals in developing coping strategies and addressing any emotional or psychological challenges associated with narcolepsy. Alternative treatments (alternative treatments) such as acupuncture, yoga, or herbal supplements may also be explored in conjunction with traditional medical approaches. It is important for individuals with narcolepsy to work closely with their healthcare team to develop a personalized treatment plan that addresses their specific symptoms and needs. By combining various treatment options, individuals with narcolepsy can find effective ways to manage their symptoms and improve their overall well-being.
Lifestyle Changes
Making certain lifestyle adjustments can significantly improve the management of narcolepsy symptoms. Here are some key lifestyle changes that individuals with narcolepsy can consider:
1. Establish a Regular Sleep Schedule: Maintaining a consistent sleep schedule is crucial for managing narcolepsy. Going to bed and waking up at the same time each day can help regulate sleep patterns and improve overall sleep quality.
2. Nap Strategically: Taking short, scheduled naps throughout the day can help combat excessive daytime sleepiness. It is advisable to limit naps to 15-20 minutes and schedule them strategically to prevent them from interfering with nighttime sleep.
3. Create a Sleep-Friendly Environment: Designing a conducive sleep environment can promote better sleep. Ensure that the bedroom is dark, quiet, and at a comfortable temperature. Consider using eye masks, earplugs, or white noise machines to aid in relaxation.
4. Regular Exercise: Engaging in regular physical activity can enhance overall sleep quality and promote wakefulness during the day. Aim for at least 30 minutes of moderate-intensity exercise, such as brisk walking or swimming, most days of the week.
5. Avoid Stimulants: Stimulants like caffeine and nicotine can worsen sleep disturbances in individuals with narcolepsy. Limiting or avoiding consumption of these substances, especially close to bedtime, can improve sleep quality.
6. Manage Stress: Stress can exacerbate narcolepsy symptoms. Implementing stress management techniques, such as deep breathing exercises, meditation, or engaging in hobbies, can help reduce stress levels and promote better sleep.
7. Nutritious Diet: A balanced diet can contribute to overall well-being and potentially improve narcolepsy symptoms. Avoid heavy meals close to bedtime and opt for a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
It’s important to note that while lifestyle changes can have a positive impact on narcolepsy management, they may not completely alleviate the symptoms. A comprehensive treatment plan, including medications and therapy, may be necessary to effectively manage narcolepsy. Discussing lifestyle changes and their potential benefits with a healthcare professional is recommended. With the right combination of strategies, individuals with narcolepsy can lead fulfilling lives and better cope with the challenges posed by this sleep disorder.
Medications
Medications play a crucial role in the treatment of narcolepsy (narcolepsy), helping to manage its symptoms and improve the overall quality of life for individuals with the disorder. One commonly prescribed type of medication is stimulants. These medications work by stimulating the central nervous system, promoting wakefulness and reducing excessive daytime sleepiness (EDS). Stimulants, such as modafinil and armodafinil, are often the first line of treatment for narcolepsy due to their effectiveness in combating EDS. However, it’s important to note that stimulants can have potential side effects, including increased heart rate, elevated blood pressure, and insomnia. Regular monitoring by a healthcare professional is crucial when taking these medications. Another class of medications prescribed for narcolepsy is antidepressants. Antidepressants, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors (SNRIs), are primarily used to manage cataplexy (cataplexy), a common symptom of narcolepsy. These medications help regulate the neurotransmitters in the brain, reducing the frequency and severity of cataplectic episodes. Additionally, sodium oxybate, which is a central nervous system depressant, can be prescribed for both cataplexy and fragmented sleep in narcolepsy. It promotes deeper, more restorative sleep and can significantly improve the symptoms associated with narcolepsy. It’s important to discuss with a healthcare provider to determine the appropriate medication and dosage that will best suit an individual’s specific needs and lifestyle.
If you’re interested in learning more about coping strategies for sleep paralysis, please check out our comprehensive guide on sleep paralysis.
Therapy
Therapy can play a crucial role in the comprehensive treatment approach for individuals with narcolepsy. Cognitive Behavioral Therapy (CBT) is one commonly utilized therapy modality that can be beneficial for managing the emotional and psychological impact of living with narcolepsy. CBT focuses on identifying and modifying negative thought patterns, beliefs, and behaviors that may contribute to stress, anxiety, and depression. Through therapy sessions, individuals can learn techniques to manage stress, improve sleep hygiene, and develop coping strategies (coping strategies) to navigate the challenges associated with narcolepsy. In addition to CBT, there are other therapy options that can be beneficial in addressing specific symptoms of narcolepsy. For example, sleep paralysis (sleep paralysis) can be particularly distressing, and therapists can help individuals understand and manage the fear and anxiety associated with these episodes. They may also provide relaxation techniques and imagery exercises to promote a sense of calm during sleep paralysis episodes. Therapy can also be a valuable resource for individuals who experience cataplexy (cataplexy). Therapists can help individuals identify triggers and develop strategies to minimize the frequency and severity of cataplexy attacks. By addressing the emotional and psychological aspects of narcolepsy alongside other treatment modalities, therapy can greatly enhance the overall well-being and quality of life for individuals living with narcolepsy.
Alternative Treatments
Alternative treatments can complement traditional approaches in managing narcolepsy symptoms. While there is no cure for narcolepsy, certain alternative therapies may offer additional support and relief. Acupuncture is a traditional Chinese therapy that involves inserting thin needles into specific points of the body to stimulate energy flow. Some individuals with narcolepsy have reported improvements in sleep quality and overall well-being after undergoing acupuncture sessions. Herbal supplements, such as valerian root or chamomile, are popular among individuals seeking natural remedies for sleep disturbances. However, it’s important to consult with a healthcare professional before incorporating any herbal supplements into your routine, as they may interact with other medications. Another alternative treatment option is yoga and meditation. These practices can promote relaxation, reduce stress, and improve sleep quality. By incorporating deep breathing exercises, gentle stretches, and mindful meditation into a daily routine, individuals with narcolepsy may experience a more restful sleep and enhanced overall well-being. It’s important to note that alternative treatments should not replace conventional medical interventions or prescribed medications. They should be used as adjunctive therapies to enhance symptom management and overall quality of life. Always consult with a healthcare professional before starting any alternative treatment to ensure safety and effectiveness. For individuals with narcolepsy, exploring various treatment modalities, such as alternative therapies, can provide additional support in managing symptoms while working towards a healthier sleep-wake pattern.
Coping with Narcolepsy

Coping with narcolepsy (narcolepsy) can be a challenging journey, but with the right strategies and support, individuals can regain control over their lives. Establishing a consistent sleep schedule is crucial for managing narcolepsy symptoms. Creating a bedtime routine and ensuring a comfortable sleep environment can promote better sleep quality. It is also important to prioritize rest throughout the day, allowing for short power naps to combat excessive daytime sleepiness (EDS). Additionally, adopting healthy lifestyle habits such as regular exercise, balanced nutrition, and stress management techniques like meditation or yoga can help improve overall well-being. Seeking support from healthcare professionals, support groups, or counseling can provide valuable guidance and emotional support during the coping process. Exploring different techniques such as cognitive-behavioral therapy can aid in managing the emotional challenges associated with narcolepsy. Another helpful coping strategy is educating family, friends, and coworkers about narcolepsy to build a supportive environment and understanding network. Finally, focusing on self-care and practicing self-compassion is important. Accepting the limitations imposed by narcolepsy while also celebrating personal victories can help individuals navigate their daily lives with resilience and optimism. In the face of the unique challenges posed by narcolepsy, individuals can take steps to adapt and thrive, improving their quality of life and overall well-being.
Living with Narcolepsy
Living with narcolepsy can present various challenges, but with proper management strategies and support, individuals can lead fulfilling lives. Here are some essential aspects to consider when navigating life with narcolepsy:
1. Establish Consistent Sleep Routine: Maintaining a regular sleep schedule is crucial for managing narcolepsy. Going to bed and waking up at consistent times can help regulate the body’s sleep-wake cycle and improve overall sleep quality.
2. Create a Sleep-Conducive Environment: Design a relaxing sleep environment that promotes restful sleep. Ensure the bedroom is quiet, dark, and at a comfortable temperature. Consider using earplugs, eye masks, or white noise machines to minimize disruptions during sleep.
3. Practice Good Sleep Hygiene: Adopting healthy sleep habits can improve the quality of sleep. Avoid stimulants like caffeine and nicotine close to bedtime, establish a relaxing pre-sleep routine, and limit daytime napping to prevent excessive sleepiness.
4. Communicate with Loved Ones: Educate family members, friends, and colleagues about narcolepsy to enhance understanding and empathy. Inform them about your symptoms, how they may impact your daily life, and the importance of support during challenging periods.
5. Seek Support: Joining support groups or connecting with others who have narcolepsy can provide valuable emotional support and a sense of community. Sharing experiences and tips for managing symptoms can be empowering and helpful in coping with the condition.
6. Explore Relaxation Techniques: Engaging in relaxation techniques such as meditation, deep breathing exercises, or yoga can help reduce stress levels and improve overall sleep quality.
7. Prioritize Safety: Understand potential risks associated with narcolepsy, such as sudden loss of muscle tone during cataplexy episodes or sleep attacks. Take necessary precautions to ensure personal safety, such as avoiding potentially hazardous activities when experiencing excessive sleepiness.
8. Maintain a Healthy Lifestyle: Adopting a well-balanced diet, regular exercise routine, and managing stress levels can contribute to overall well-being and minimize symptoms of narcolepsy.
Remember, each individual’s experience with narcolepsy is unique. It is essential to work closely with healthcare professionals to develop an individualized management plan that addresses specific symptoms and improves quality of life. With the right strategies and support, individuals with narcolepsy can thrive and live fulfilling lives.
Research and Advancements
Research and advancements in the field of narcolepsy continue to shed light on this complex disorder and offer hope for improved management and treatment options. Scientists and medical professionals are actively working to unravel the underlying mechanisms of narcolepsy in order to develop targeted therapies. One area of focus is the study of the brain chemicals involved in sleep-wake regulation, such as hypocretin. Researchers are investigating the role of hypocretin in narcolepsy and exploring potential ways to replenish or modulate it to alleviate symptoms. Additionally, genetic studies have revealed specific genes that may be associated with an increased risk of developing narcolepsy. Understanding the genetic factors at play could lead to tailored treatment approaches in the future. Alongside these biological investigations, advancements in technology have also provided new tools for diagnosing and managing narcolepsy. Sleep studies, including polysomnography and multiple sleep latency tests, have become more sophisticated, allowing for more accurate and comprehensive assessments of sleep patterns and disorders. Treatment options for narcolepsy are also evolving. Novel medications targeting specific symptoms, such as cataplexy and EDS, are being developed to provide tailored relief. Research is exploring the possible benefits of non-pharmacological approaches, such as cognitive behavioral therapy and lifestyle modifications, in managing narcolepsy symptoms and improving overall well-being. As our understanding of narcolepsy deepens and research progresses, the hope is that individuals with narcolepsy will have access to more effective treatments and improved quality of life. To stay updated on the latest advancements in narcolepsy research, it is recommended to consult reputable sources and engage with healthcare professionals specialized in sleep disorders.
Conclusion
In conclusion, narcolepsy is a complex sleep disorder that presents a variety of perplexing symptoms. From excessive daytime sleepiness (EDS) to cataplexy, sleep paralysis, hallucinations, and fragmented sleep, individuals with narcolepsy face unique challenges in their daily lives. While the exact cause of narcolepsy is still not fully understood, ongoing research is shedding light on potential genetic and neurological factors that may contribute to its development. Diagnosis of narcolepsy involves a thorough evaluation of symptoms, sleep studies, and other diagnostic tests. Treatment options for narcolepsy include a combination of lifestyle changes, medications, therapy, and alternative treatments. With the right management strategies and support, individuals with narcolepsy can learn to cope effectively and lead fulfilling lives. It is important for those with narcolepsy to seek professional help and connect with support networks to navigate the ups and downs of living with this chronic condition. By staying informed about the latest research and advancements, individuals with narcolepsy can be hopeful for future breakthroughs in understanding and managing this enigmatic disorder. To learn more about related sleep disorders and prevention strategies, you can read our article on sleepwalking causes, risks, and prevention strategies.
Frequently Asked Questions
1. What are the main risk factors for developing narcolepsy?
While the exact cause of narcolepsy remains unknown, certain factors can increase the risk of developing this sleep disorder. Genetic predisposition plays a significant role, as narcolepsy tends to run in families. Additionally, certain infections, such as H1N1 flu or streptococcus infections, have been linked to an increased risk of developing narcolepsy. Other factors, such as hormonal changes, autoimmune disorders, and brain injuries, may also contribute to the development of narcolepsy.
2. Can narcolepsy be diagnosed in children?
Yes, narcolepsy can occur in children, although it is relatively rare. Pediatric narcolepsy often presents with similar symptoms as in adults, including excessive daytime sleepiness, cataplexy, and disrupted nighttime sleep. However, the diagnosis and management of narcolepsy in children may require specialized pediatric sleep medicine expertise.
3. Is narcolepsy a progressive disorder?
Narcolepsy is not considered a progressive disorder in the traditional sense. The symptoms of narcolepsy, such as excessive daytime sleepiness and cataplexy, typically persist throughout a person’s life. However, with appropriate treatment and management strategies, individuals with narcolepsy can effectively control their symptoms and lead fulfilling lives.
4. Are there any natural remedies or lifestyle changes that can alleviate narcolepsy symptoms?
While there are no known natural remedies to cure narcolepsy, certain lifestyle changes can help manage the symptoms. Establishing a regular sleep schedule, maintaining good sleep hygiene, practicing stress management techniques, and avoiding triggers such as alcohol and caffeine can all contribute to better symptom control in individuals with narcolepsy.
5. Can medications for narcolepsy cause addiction?
Medications used to treat narcolepsy, such as stimulants or sodium oxybate, are generally safe when taken as prescribed. While these medications may carry a risk of dependency or tolerance with prolonged use, proper monitoring and adherence to the prescribed dosage can help minimize these risks. It is important to consult with a healthcare professional for guidance on appropriate medication use.
6. Are there any support groups available for individuals with narcolepsy?
Yes, there are several support groups and organizations dedicated to providing resources, education, and support to individuals living with narcolepsy. These groups offer a sense of community, a platform to share experiences, and valuable information on coping strategies for managing narcolepsy. Examples of such organizations include the Narcolepsy Network and Wake Up Narcolepsy.
7. Can narcolepsy impact a person’s ability to drive?
Yes, narcolepsy can pose challenges for individuals when it comes to driving safely. Excessive daytime sleepiness and sudden loss of muscle control (cataplexy) can significantly impair a person’s ability to operate a vehicle. It’s important for individuals with narcolepsy to discuss driving restrictions and safety precautions with their healthcare provider to minimize any potential risks.
8. Are there any alternative therapies that can be used alongside conventional treatments for narcolepsy?
While there is limited scientific evidence supporting the efficacy of alternative therapies in managing narcolepsy, some individuals may find complementary practices such as yoga, acupuncture, or relaxation techniques helpful for symptom management. It is important to discuss these options with a healthcare professional and use them as adjuncts to conventional medical treatments.
9. Can narcolepsy lead to other health complications?
Narcolepsy itself does not cause severe health complications, but it can significantly impact an individual’s quality of life. The excessive daytime sleepiness and sudden loss of muscle control can increase the risk of accidents and injuries. Additionally, the chronic sleep disruption associated with narcolepsy may contribute to a higher risk of mental health issues such as depression or anxiety.
10. Is there ongoing research to better understand narcolepsy and develop new treatments?
Yes, there is ongoing research aimed at unraveling the complexities of narcolepsy. Researchers are exploring potential genetic markers, studying the underlying mechanisms of the disorder, and investigating new treatment options. Advances in understanding narcolepsy offer hope for improved diagnosis methods, targeted therapies, and enhanced management strategies in the future.