Have you ever woken up from sleep and found yourself completely unable to move or speak? It can be an incredibly unsettling experience, leaving you feeling trapped in your own body. This phenomenon is known as sleep paralysis, and it affects a surprising number of people. In this article, we will delve into the intricacies of sleep paralysis, exploring its causes, symptoms, and possible treatments. Whether you have personally experienced sleep paralysis or are simply curious about this enigmatic condition, join us as we unravel the mysteries behind this peculiar and often terrifying sleep disorder.
What is Sleep Paralysis?
Sleep paralysis is a fascinating yet perplexing phenomenon that occurs during the transition between wakefulness and sleep. During this state, individuals find themselves temporarily unable to move or speak, despite being fully conscious of their surroundings. It is as if the body is experiencing a temporary loss of muscle control, rendering the person immobile. This inability to move can last for a few seconds to several minutes, causing considerable distress and anxiety. In addition to the physical immobilization, sleep paralysis often brings along vivid hallucinations, including eerie figures or a feeling of an overwhelming presence in the room. Many people report a sense of pressure on their chest, making it difficult to breathe. Understandably, these experiences can lead to a profound feeling of terror and panic for those who go through them.
Sleep paralysis typically occurs during two distinct stages: upon falling asleep (hypnagogic or predormital sleep paralysis) and upon waking up (hypnopompic or postdormital sleep paralysis). During these transitional moments, the brain seamlessly switches between sleep states, and sleep paralysis can occur if this process becomes disrupted. While the exact mechanisms behind sleep paralysis are not fully understood, one theory suggests that it may be linked to the body’s natural sleep-wake cycle and the inhibition of voluntary muscle movement during rapid eye movement (REM) sleep. REM sleep is characterized by dreaming and a temporary paralysis of the muscles to prevent individuals from acting out their dreams. In sleep paralysis, this paralysis persists even after waking up or before falling asleep, causing the unsettling sensation of being trapped in one’s own body.
Although sleep paralysis itself is considered harmless, it can significantly impact an individual’s quality of sleep and overall well-being. Episodes of sleep paralysis may be isolated, but they can also occur frequently in some individuals, even multiple times within a single night. The fear of experiencing sleep paralysis can create anxiety around sleep, leading to disrupted sleep patterns and increased daytime fatigue. It is important to note that sleep paralysis is not considered a sleep disorder in itself but rather a symptom associated with various underlying factors. Understanding the causes and symptoms of sleep paralysis is crucial in order to address the root issue and find appropriate solutions for better sleep and reduced episodes of paralysis. So, let’s unravel the mysteries of sleep paralysis and explore the factors that contribute to its occurrence.
Causes of Sleep Paralysis

Sleep paralysis can be attributed to a variety of factors, ranging from sleep disorders to irregular sleep patterns and high levels of stress and anxiety. One of the primary causes of sleep paralysis is sleep disorders, such as narcolepsy and sleep apnea. These conditions disrupt the normal sleep cycle and can increase the likelihood of experiencing episodes of sleep paralysis. Additionally, individuals with inconsistent sleep patterns, such as those who frequently change their sleep schedule or suffer from jet lag, may be more prone to experiencing sleep paralysis. The body’s internal clock plays a significant role in regulating sleep, and disruptions to this rhythm can disrupt the transition between sleep stages and potentially trigger episodes. Stress and anxiety are also closely linked to sleep paralysis. High levels of stress can lead to sleep disturbances and alterations in sleep architecture, which can manifest as sleep paralysis. Finally, sleeping on your back has been associated with a higher incidence of sleep paralysis, as this position can increase the probability of experiencing episodes. By understanding the potential causes of sleep paralysis, individuals can take steps to address these underlying factors and potentially reduce the occurrence of these unsettling experiences.
Sleep Disorders
Sleep disorders can play a significant role in the occurrence of sleep paralysis. Various sleep disorders disrupt the normal sleep cycle, leading to imbalances in the different stages of sleep and potentially triggering episodes of sleep paralysis. One such disorder is narcolepsy, a neurological condition characterized by excessive daytime sleepiness and sudden, uncontrollable bouts of sleep. Narcolepsy is often accompanied by other symptoms like cataplexy, which is the sudden loss of muscle tone triggered by emotions. These abrupt muscle weaknesses experienced in narcolepsy resemble the temporary paralysis seen in sleep paralysis. Another sleep disorder associated with sleep paralysis is insomnia. Chronic insomnia, marked by difficulty falling asleep or staying asleep, disrupts the natural sleep-wake cycle, making individuals more susceptible to sleep paralysis episodes during disrupted transitions between wakefulness and sleep. Additionally, sleep apnea, a disorder characterized by interrupted breathing during sleep, can also contribute to sleep paralysis. The interruptions in breathing during sleep apnea cause frequent arousals, disturbing the normal sleep cycle and potentially leading to episodes of sleep paralysis. A study published in the Journal of Sleep Research found a correlation between sleep apnea and sleep paralysis, suggesting that the disturbed respiratory patterns associated with sleep apnea could hinder the smooth transition between sleep states, increasing the likelihood of sleep paralysis occurrences. Understanding and addressing underlying sleep disorders is essential in managing sleep paralysis and achieving a healthier sleep pattern. If you’re interested in learning more about different sleep disorders, you can read our article on the top 10 sleep disorders that affect individuals worldwide.
Irregular Sleep Patterns
Irregular sleep patterns can contribute to the occurrence of sleep paralysis. When our sleep schedule is inconsistent or disrupted, it can disrupt the natural sleep-wake cycle and increase the likelihood of experiencing sleep paralysis. This can happen when we have irregular sleep patterns due to shift work, jet lag, or frequent changes in sleep schedule.
One possible explanation for this is that irregular sleep patterns can disrupt the body’s internal clock, known as the circadian rhythm. The circadian rhythm regulates the timing of various physiological processes, including sleep and wakefulness. When the circadian rhythm is disrupted, it can lead to fragmented sleep and an imbalance in the sleep stages, including REM sleep where sleep paralysis is most likely to occur.
Additionally, irregular sleep patterns can affect the duration and quality of our sleep. When we do not get enough sleep or have poor sleep quality, it can increase the chances of experiencing sleep paralysis. Sleep deprivation, whether it is due to insufficient sleep time or poor sleep quality, can disrupt the normal sleep cycle, making it more likely for sleep paralysis to occur.
To mitigate the impact of irregular sleep patterns on sleep paralysis, it is important to establish a consistent sleep schedule. Going to bed and waking up at the same time every day, even on weekends, can help regulate the circadian rhythm and promote healthier sleep patterns. Creating a bedtime routine that includes relaxation techniques, such as reading a book or taking a warm bath, can also signal the body to prepare for sleep.
It is crucial to create a sleep-friendly environment that promotes restful sleep. This includes keeping the bedroom dark, cool, and quiet, and avoiding stimulating activities or screens before bed. Regular exercise during the day can also improve sleep quality and help regulate the sleep-wake cycle.
By addressing and correcting irregular sleep patterns, individuals may reduce the frequency of sleep paralysis episodes and improve overall sleep quality. However, if sleep paralysis persists despite addressing these factors, it may be necessary to consult with a healthcare professional to explore other underlying causes or related sleep disorders. Understanding the importance of regular sleep patterns can greatly contribute to managing sleep paralysis and promoting healthier sleep.
Stress and Anxiety
Stress and anxiety are significant factors that can contribute to the occurrence of sleep paralysis. When we experience high levels of stress or anxiety, our bodies can become hyperaroused, making it difficult to relax and fall into a deep, restful sleep. This can disrupt the normal sleep cycle and increase the likelihood of experiencing sleep paralysis episodes. Additionally, stress and anxiety can trigger an overactivation of the sympathetic nervous system, which is responsible for our “fight-or-flight” response. This heightened state of arousal can make it harder for the body to transition smoothly between sleep stages and increase the chances of experiencing sleep paralysis.
It is important to note that sleep paralysis itself can also be a source of anxiety and stress. The fear of experiencing another episode can create a cycle of worry and anticipation, further exacerbating the problem. This anxiety can perpetuate a vicious cycle, leading to more frequent episodes of sleep paralysis.
To address the role of stress and anxiety in sleep paralysis, it is crucial to develop effective stress management techniques. Engaging in activities such as mindfulness meditation, deep breathing exercises, or yoga can help calm the mind and promote relaxation before bedtime. Creating a nighttime routine that promotes a peaceful environment and reduces stressors can also be beneficial. This can include activities such as reading a book, taking a warm bath, or listening to soothing music. Additionally, seeking support from a therapist or counselor can provide valuable guidance and strategies for managing stress and anxiety.
It is worth mentioning that if stress and anxiety persist and significantly impact your daily life, it is essential to seek professional help. Mental health professionals can provide appropriate interventions, such as cognitive-behavioral therapy or medication if necessary. Taking steps to address and manage stress and anxiety can not only improve overall well-being but also reduce the frequency and severity of sleep paralysis episodes. Remember, understanding and addressing the underlying factors contributing to sleep paralysis is crucial for finding relief and achieving restful sleep.
Sleep Deprivation
Sleep deprivation plays a significant role in the occurrence of sleep paralysis. When we consistently fail to get adequate sleep, our body and mind become more susceptible to disruptions in the sleep-wake cycle. Sleep deprivation can occur due to various factors, such as work schedules, lifestyle choices, or underlying sleep disorders. When our sleep is consistently disrupted or shortened, it can prevent our brain from going through the necessary stages of sleep properly, including the important REM sleep where dreams occur. This disruption in the sleep cycle can lead to an imbalance in neurotransmitters and hormones that regulate sleep, potentially triggering episodes of sleep paralysis.
Sleep deprivation can contribute to increased stress levels and overall fatigue, making the body more susceptible to experiencing sleep paralysis. Chronic lack of sleep can weaken the body’s natural defenses and disrupt its ability to achieve restorative sleep. It is important to note that the relationship between sleep deprivation and sleep paralysis is bidirectional – sleep deprivation can increase the likelihood of sleep paralysis, while experiencing sleep paralysis can further disrupt an individual’s sleep, leading to ongoing sleep deprivation.
Treatment for sleep deprivation involves prioritizing sleep hygiene and practicing healthy sleep habits. Establishing a consistent sleep schedule, creating a comfortable sleep environment, and practicing relaxation techniques can all contribute to improving sleep quality. In cases where sleep deprivation is a symptom of an underlying sleep disorder, addressing and treating that disorder is crucial in alleviating sleep deprivation and reducing the likelihood of sleep paralysis episodes. If recurring nightmares are associated with sleep deprivation and sleep paralysis, it may be helpful to seek professional guidance to explore the connection between them and develop effective treatment strategies. Understanding the link between sleep deprivation and sleep paralysis can empower individuals to take control of their sleep health and seek appropriate solutions to promote better sleep and overall well-being.
Sleeping on Your Back
Sleeping on your back is a common sleeping position for many individuals, but it can also increase the likelihood of experiencing sleep paralysis. When you sleep on your back, your airways can become partially blocked, leading to disruptions in breathing patterns. This can trigger episodes of sleep paralysis, as the body tries to prevent you from acting out your dreams while also dealing with restricted airflow. Additionally, sleeping on your back can exacerbate issues related to sleep disorders such as obstructive sleep apnea, where breathing pauses frequently during sleep.
In some cases, individuals who sleep on their back may also experience a higher frequency of sleep paralysis episodes due to the way this position affects the brain’s transition between sleep stages. Sleeping on your back can potentially lead to an increase in REM sleep, the stage of sleep most closely associated with vivid dreaming. This prolonged time in REM sleep increases the chances of experiencing sleep paralysis, as this state is characterized by temporary muscle paralysis to prevent you from physically acting out your dreams.
To reduce the risk of sleep paralysis while sleeping on your back, it may be beneficial to try alternative sleeping positions. Sleeping on your side or stomach can alleviate the pressure on your airways and potentially reduce the occurrence of obstructed breathing. Experimenting with different pillow placements or using specially designed pillows that encourage side-sleeping can also be helpful. Additionally, maintaining a consistent sleep schedule and practicing relaxation techniques before bed can promote more restful sleep and potentially reduce the likelihood of sleep paralysis episodes.
It is important to understand that while sleeping on your back can be a contributing factor to sleep paralysis, it may not be the sole cause. Sleep paralysis is a complex phenomenon influenced by various factors like sleep disorders, irregular sleep patterns, stress, and anxiety. By addressing these underlying issues, including altering sleeping positions, individuals may decrease the frequency of sleep paralysis episodes and improve their overall sleep quality. So, if you often experience sleep paralysis and tend to sleep on your back, it might be worth exploring different sleep positions to see if there is any positive impact.
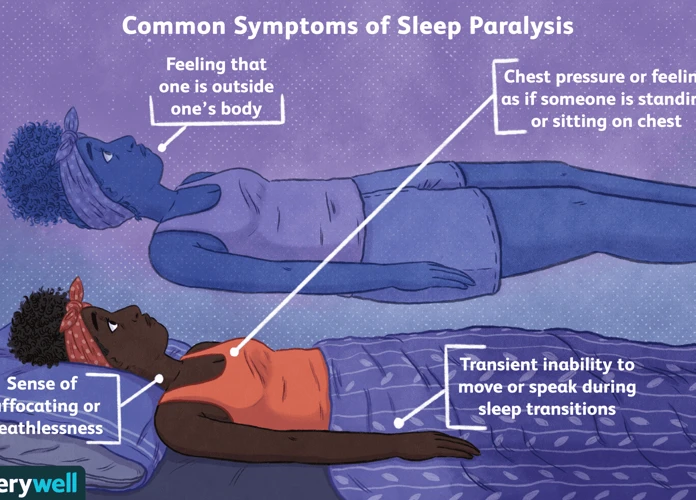
Symptoms of Sleep Paralysis
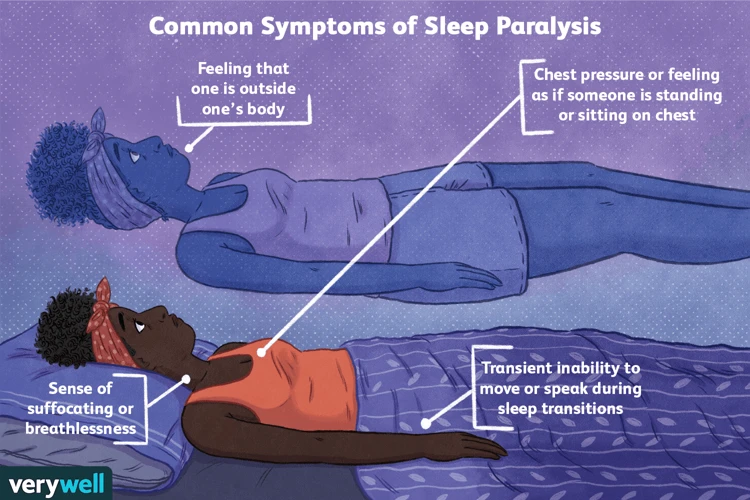
During episodes of sleep paralysis, individuals experience a range of unsettling symptoms that can be both physical and psychological in nature. The most prominent symptom of sleep paralysis is immobility, where one finds themselves unable to move their limbs or speak despite being fully conscious. This sense of paralysis can be accompanied by vivid hallucinations, which often involve seeing shadowy figures, feeling a presence in the room, or perceiving eerie sensations. Some may also experience a feeling of pressure on their chest, making it difficult to breathe. Additionally, individuals going through sleep paralysis may feel a profound sense of terror and panic, as the experience can be incredibly distressing. While these symptoms can vary in intensity and duration, they contribute to the overall perplexity and fear associated with sleep paralysis. Understanding the symptoms is essential in recognizing and differentiating sleep paralysis from other sleep-related issues, such as recurring nightmares or sleep disorders (source).
Immobility
Immobility is one of the key symptoms of sleep paralysis. During an episode of sleep paralysis, individuals find themselves completely unable to move their body, despite their conscious awareness of their surroundings. It is as if a heavy weight is pressing down on them, rendering their muscles unresponsive. This feeling of physical paralysis can be incredibly distressing and alarming, as it goes against our natural instinct to move and react.
The immobility experienced during sleep paralysis is closely linked to the inhibition of voluntary muscle movement that occurs during REM sleep. During REM sleep, the brain sends signals to temporarily paralyze the muscles, preventing us from physically acting out our dreams and potentially causing harm to ourselves or others. This paralysis is known as REM atonia. Normally, when we transition from REM sleep to wakefulness, the paralysis gradually dissipates, allowing us to regain control of our muscles. However, in the case of sleep paralysis, this paralysis persists even though the individual has already awakened or is in the process of waking up.
The immobility experienced during sleep paralysis can vary in duration, with episodes lasting from a few seconds to several minutes. The inability to move can lead to a sense of frustration, panic, and even terror. People often describe feeling trapped or imprisoned in their own bodies, desperately attempting to move or scream but being unable to do so. It is important to remember that even though the sensation of immobility during sleep paralysis may be distressing, it is not a physically harmful condition.
Addressing the immobility aspect of sleep paralysis involves understanding the underlying causes and finding ways to manage and reduce the occurrence of episodes. Some techniques that may help include improving sleep hygiene, establishing a regular sleep schedule, reducing stress levels, and creating a calm and comfortable sleep environment. In some cases, for individuals who experience frequent and disruptive episodes of sleep paralysis, consulting with a medical professional may be beneficial to explore potential treatment options, such as medications that target underlying sleep disorders or nightmares.
By understanding the immobility aspect of sleep paralysis and its connection to REM atonia, individuals can gain insights into their experiences and take steps to alleviate the distress associated with this symptom. It is an intriguing phenomenon that continues to be studied and explored, providing valuable insights into the complexities of the human sleep-wake cycle and the mysteries of our subconscious minds.
Hallucinations
Hallucinations are a common feature of sleep paralysis and often contribute to the intense fear and unease experienced during an episode. These hallucinations can take various forms, ranging from auditory sensations to vivid visual images. As the mind transitions between sleep and wakefulness, it can generate sensory perceptions that feel incredibly real. Individuals may see shadowy figures or monstrous creatures lurking in the room, even though there is no actual presence. These hallucinatory experiences can be incredibly vivid, with details that are indistinguishable from reality. The brain, still partially in a dream state, can create scenarios that are highly unsettling and terrifying.
The hallucinations experienced during sleep paralysis are known as hypnagogic hallucinations when they occur during the onset of sleep, and hypnopompic hallucinations when they happen upon waking up. These hallucinations may be influenced by an individual’s cultural background, personal fears, and existing beliefs. For example, someone with a strong belief in the supernatural may perceive the presence of ghosts or demons, while others may envision more mundane, yet still distressing, scenarios.
It is worth noting that these hallucinations are generally harmless and are a result of the brain trying to make sense of the unusual state between consciousness and sleep. They can appear so vivid and convincing that it becomes challenging to distinguish them from reality, which adds to the overall confusion and fear experienced during sleep paralysis. Understanding that these hallucinations are a natural part of the phenomenon can help individuals cope with the distress caused by them.
In some cases, the hallucinations experienced during sleep paralysis can be indistinguishable from nightmares. This similarity has led to the exploration of medication, such as selective serotonin reuptake inhibitors (SSRIs), as a possible treatment option. SSRIs, commonly used to treat depression and anxiety, have been found to reduce the frequency and intensity of nightmares, including those associated with sleep disorders. However, more research is needed to determine the effectiveness of medication specifically for managing hallucinations during sleep paralysis.
The hallucinations that occur during sleep paralysis can be extremely vivid and terrifying. These visual and auditory perceptions are a result of the brain’s attempt to make sense of the blurred boundaries between sleep and wakefulness. While medication may hold promise in treating hallucinations related to sleep disorders and nightmares, further investigation is required to establish its efficacy in managing sleep paralysis hallucinations.
Feeling of Pressure
During sleep paralysis, a common and unsettling symptom that individuals often experience is a feeling of pressure on their chest. This sensation can range from mild discomfort to a sense of immense heaviness, making it difficult to breathe properly. It’s important to note that this feeling of pressure is purely subjective and not caused by any external force.
The exact cause of this sensation is not fully understood, but several theories have been proposed. One possibility is that the feeling of pressure on the chest during sleep paralysis may be related to the body’s natural relaxation response during sleep. As the muscles in the body become more relaxed, including those involved in breathing, individuals may perceive this relaxation as a heaviness or pressure on their chest.
Another theory suggests that the feeling of pressure may be linked to the activation of the body’s stress response during sleep paralysis. When the brain transitions between wakefulness and sleep, there can be a surge in stress hormones, such as cortisol. This hormonal surge may contribute to a heightened perception of physical sensations, including the feeling of pressure on the chest.
It is worth noting that the feeling of pressure on the chest during sleep paralysis can also be accompanied by a sense of difficulty breathing. Individuals may feel as though their breath is shallow or restricted, adding to the overall distress of the experience. However, it is important to understand that while the sensation can feel alarming, it is generally not harmful and does not pose any immediate danger to one’s health.
Managing and alleviating the feeling of pressure during sleep paralysis can be challenging, but several strategies may help. First and foremost, it is essential to stay calm and remind yourself that the experience is temporary and will pass. Deep breathing exercises can help promote relaxation and ease the feeling of restricted breathing. Practicing stress reduction techniques, such as meditation or progressive muscle relaxation, may also help minimize the intensity of the pressure sensation.
In certain cases where the feeling of pressure during sleep paralysis becomes particularly distressing or interferes with a person’s sleep quality, medical interventions may be considered. Consulting with a healthcare professional, such as a sleep specialist or therapist, can provide guidance on potential treatment options tailored to individual needs. They may explore techniques such as cognitive-behavioral therapy or, in rare cases, discuss the role of medication in managing sleep paralysis and associated symptoms.
As we delve further into the factors that contribute to sleep paralysis, understanding the sensation of pressure on the chest is crucial for individuals who seek to overcome the distressing experiences associated with this phenomenon. By unraveling the mysteries behind sleep paralysis and implementing appropriate strategies, individuals can take steps towards a better night’s sleep and reduced occurrence of sleep paralysis episodes.
Difficulty Breathing
Difficulty breathing is a distressing symptom that often accompanies episodes of sleep paralysis. Many individuals report feeling a sensation of tightness in their chest, as if a heavy weight is pressing down on them. This feeling of pressure can make it challenging to take deep breaths, leading to a sense of suffocation or shortness of breath. While the physical sensation of difficulty breathing during sleep paralysis can be intense and frightening, it’s important to note that it is generally a subjective experience and not a result of actual respiratory problems. Despite the feeling of being unable to breathe, the body is still receiving sufficient oxygen, and the respiratory system continues to function normally.
During sleep paralysis, the brain is in a state between wakefulness and REM sleep, where muscle tone is reduced, including the muscles involved in breathing. This reduction in muscle activity can give the illusion of breathlessness, further exacerbating the distress experienced during an episode. It is crucial to remember that although it can be challenging, maintaining calmness and reminding oneself that it is a temporary state can help alleviate some of the anxiety related to difficulty breathing.
For individuals who find that difficulty breathing during sleep paralysis significantly impacts their emotional well-being or sleep quality, seeking medical advice is recommended. It is important to rule out any underlying respiratory disorders or conditions that may contribute to the sensations experienced during sleep paralysis. In some cases, healthcare providers may recommend certain medications or techniques to manage the symptoms and improve overall sleep quality. However, it is essential to consult with a healthcare professional before considering any medications or interventions.
To explore more about the role of medication in treating nightmares and sleep disorders, feel free to check out our related article that provides insights and information on how medication can be utilized as part of a comprehensive treatment plan.
Terror and Panic
Experiencing terror and panic is a common and distressing aspect of sleep paralysis. When individuals find themselves temporarily paralyzed and aware of their surroundings, it can be an incredibly frightening and disorienting experience. The inability to move coupled with the vivid hallucinations that often accompany sleep paralysis can instill a sense of intense fear and terror. The hallucinations may involve seeing shadowy figures, demonic entities, or a sense of a malevolent presence in the room. These hallucinations can feel incredibly real, leading to a heightened state of panic and a desperate urge to break free from the paralysis.
The terror and panic experienced during sleep paralysis may also be exacerbated by the feeling of pressure on the chest, which creates a sensation of restricted breathing. This physical sensation, combined with the inability to move, can intensify the fear and make individuals feel as if they are suffocating or being crushed. It is important to note that while these sensations and hallucinations may seem terrifying, they are not harmful or indicative of any underlying physical harm.
The emotional toll of sleep paralysis can be significant, leaving individuals anxious and fearful about going to bed and falling asleep. The anticipation of experiencing another episode of sleep paralysis can lead to heightened anxiety, which in turn can disrupt sleep further and contribute to a vicious cycle of sleep deprivation and more frequent occurrences of sleep paralysis. Managing these feelings of terror and panic is essential for those who experience sleep paralysis. Various relaxation techniques and coping strategies, such as deep breathing exercises, visualization, and mindfulness, can help individuals calm their minds and reduce anxiety.
In some cases, understanding the nature of sleep paralysis and its non-harmful nature can be reassuring to individuals, reducing the fear and panic associated with the experience. Seeking support from professionals, like sleep specialists or therapists, can also provide valuable guidance and help individuals develop effective coping mechanisms to alleviate the distress caused by sleep paralysis. Additionally, creating a sleep-friendly environment that promotes relaxation and calmness can contribute to better sleep quality and a reduced frequency of sleep paralysis episodes, ultimately minimizing the terror and panic associated with this phenomenon.
Treatment for Sleep Paralysis
Treating sleep paralysis involves addressing the underlying factors that contribute to its occurrence. One of the first steps in managing sleep paralysis is establishing a regular sleep schedule and routine. This includes sticking to consistent bedtimes and wake-up times, as well as creating a relaxing pre-sleep routine to signal to the body that it is time to unwind and prepare for rest. Managing stress and anxiety is also crucial, as these factors can exacerbate sleep paralysis episodes. Techniques such as deep breathing exercises, meditation, and mindfulness practices can help reduce stress levels. Additionally, avoiding stimulants like caffeine and alcohol before bedtime can improve sleep quality and reduce the likelihood of experiencing sleep paralysis. Creating a sleep-friendly environment is another important step, ensuring that the sleeping area is comfortable, cool, and free from distractions. For those who experience frequent sleep paralysis episodes that significantly impact their daily life, medical interventions may be necessary. These interventions may include prescribing medications that regulate sleep patterns or addressing any underlying sleep disorders that contribute to sleep paralysis. A multifaceted approach that combines lifestyle adjustments, stress management techniques, and, if needed, medical support can help individuals effectively manage and reduce the occurrence of sleep paralysis episodes.
Sleep Schedule and Routine
Creating and maintaining a consistent sleep schedule and routine is vital in managing sleep paralysis. A regular sleep schedule helps regulate the body’s internal clock, promoting healthy sleep patterns and reducing the likelihood of sleep disruptions, including episodes of paralysis. Aim to establish a consistent bedtime and wake-up time, even on weekends, to ensure a stable sleep routine.
In addition to a set schedule, incorporating sleep-promoting habits into your nightly routine can further enhance the quality and quantity of your sleep. Establish a relaxing pre-sleep ritual that signals to your body and mind that it’s time to unwind and prepare for sleep. This may include activities such as taking a warm bath, practicing relaxation techniques like deep breathing or meditation, or engaging in light reading. Avoid stimulating activities close to bedtime, such as using electronic devices or consuming caffeine, as they can interfere with the onset of sleep.
Creating a sleep-friendly environment can also contribute to a more restful sleep and potentially reduce the occurrence of sleep paralysis. Ensure your bedroom is cool, dark, and quiet, promoting a calm and comfortable atmosphere. Consider using earplugs, eye masks, or white noise machines if external disturbances are a concern.
It is important to establish a consistent wake-up routine that allows you to start your day feeling refreshed. Open your curtains or expose yourself to natural light upon waking to help regulate your body’s internal clock and promote alertness.
By prioritizing a consistent sleep schedule and establishing a relaxing sleep routine, you can promote better sleep hygiene and potentially reduce the occurrences of sleep paralysis. Remember, it is always beneficial to consult with a healthcare professional if you experience persistent sleep paralysis or other sleep-related concerns.
Stress Management Techniques
When it comes to managing sleep paralysis, addressing the underlying stress and anxiety in one’s life can be incredibly beneficial. Stress is known to disrupt sleep patterns and increase the likelihood of experiencing sleep paralysis episodes. Incorporating stress management techniques into daily routines can help alleviate the frequency and intensity of these episodes.
One effective stress management technique is practicing relaxation exercises, such as deep breathing, meditation, or progressive muscle relaxation. Deep breathing exercises involve taking slow, deep breaths to activate the body’s relaxation response. Meditation allows individuals to quiet the mind, reduce racing thoughts, and promote a sense of calm. Progressive muscle relaxation involves tensing and then releasing different muscle groups to release tension and promote relaxation throughout the body.
Engaging in regular physical exercise is another excellent stress management tool. Exercise not only helps reduce stress and anxiety levels but also improves overall sleep quality. Engaging in activities like yoga, jogging, or swimming can not only help manage stress but also promote better sleep hygiene.
Incorporating stress-reducing activities into one’s daily routine is crucial. These activities may include hobbies, such as painting, playing a musical instrument, or engaging in crafts. Engaging in activities that bring joy and relaxation can help divert attention from stressors and promote a sense of well-being.
Establishing healthy sleep habits and routines is another important aspect of stress management for individuals experiencing sleep paralysis. Creating a soothing bedtime routine that includes activities like reading, taking a warm bath, or listening to calming music can help signal the body that it’s time to unwind and prepare for sleep. It is also crucial to maintain a consistent sleep schedule, going to bed and waking up at the same time every day, even on weekends or days off.
In addition to these techniques, seeking support from a therapist or counselor can be extremely beneficial for managing stress and anxiety related to sleep paralysis. Cognitive-behavioral therapy (CBT) has shown to be particularly effective in helping individuals cope with stress and anxiety disorders. A therapist can help identify triggers, develop coping strategies, and provide a safe space to discuss and process emotions related to sleep paralysis.
Remember, managing stress is a continuous process, and what works for one person may not work for another. Experimenting with different techniques and finding what works best for individual needs is key. By actively managing stress, individuals may find a reduction in sleep paralysis episodes and an improvement in overall well-being.
Avoiding Stimulants and Alcohol
Avoiding stimulants and alcohol is an important aspect of managing sleep paralysis. Stimulants such as caffeine and nicotine can have a significant impact on sleep quality and disrupt the normal sleep cycle. These substances can make it harder for individuals to fall asleep and increase the likelihood of experiencing sleep disturbances like sleep paralysis. It is advisable to limit or avoid consuming caffeine-containing beverages like coffee, tea, and energy drinks, especially in the afternoon and evening.
Alcohol, while initially sedating, can also lead to disrupted sleep patterns. It may cause individuals to wake up frequently during the night and experience poor sleep quality overall. These disruptions can potentially trigger episodes of sleep paralysis or exacerbate existing symptoms. It is best to avoid alcohol close to bedtime to promote better sleep and reduce the risk of experiencing sleep paralysis.
Instead of relying on stimulants and alcohol, individuals can explore healthier alternatives that promote relaxation and improve sleep quality. This includes practicing good sleep hygiene, such as establishing a consistent sleep schedule, creating a peaceful sleep environment, and engaging in nighttime rituals that promote relaxation, such as reading a book or taking a warm bath. Additionally, incorporating relaxation techniques like deep breathing exercises or mindfulness meditation can help to further reduce stress and promote better sleep.
By consciously avoiding stimulants and alcohol and adopting healthier sleep habits, individuals can create an environment that supports restful sleep and potentially reduce the occurrences of sleep paralysis. It is important to note that lifestyle changes alone may not completely eliminate sleep paralysis episodes, especially if there are underlying medical conditions contributing to its occurrence. In such cases, it is advisable to seek medical advice to explore further treatment options.
Creating a Sleep-Friendly Environment
Creating a sleep-friendly environment can significantly improve your chances of getting a good night’s rest and reduce the likelihood of experiencing sleep paralysis. Here are some tips to help you achieve an optimal sleep environment:
1. Control the temperature: Make sure your bedroom is at a comfortable temperature, typically between 60 to 67 degrees Fahrenheit (15 to 19 degrees Celsius). A cooler room promotes better sleep, as it mimics the natural drop in body temperature that occurs during sleep.
2. Eliminate noise: Noise can disrupt your sleep and make it harder to fall asleep or stay asleep. Use earplugs, a white noise machine, or a fan to mask unwanted sounds and create a quieter sleep environment.
3. Keep it dark: Ensure your bedroom is as dark as possible. Use blackout curtains or an eye mask to block out any external light sources that can interfere with your sleep. Even small sources of light, such as electronic devices or alarm clocks, can disrupt your sleep patterns.
4. Invest in a comfortable mattress and pillows: A good mattress and pillows are essential for proper spinal alignment and support. Choose a mattress that suits your preferred sleeping position and provides the right level of firmness or softness. Pillows should support your head and neck to avoid strain and discomfort.
5. Minimize electronic devices: The blue light emitted by electronic devices, such as smartphones, tablets, and laptops, can interfere with your sleep by suppressing the production of melatonin, a hormone that regulates sleep. Avoid using electronic devices at least an hour before bedtime, or use blue light filters or night mode settings to reduce the impact of blue light.
6. Keep your bedroom clutter-free: A messy and cluttered environment can create mental stress and make it difficult to relax. Keep your bedroom clean and organized to promote a sense of calm and tranquility.
7. Establish a bedtime routine: A consistent bedtime routine signals to your body that it’s time to wind down and prepare for sleep. Engage in relaxing activities such as reading a book, taking a warm bath, or practicing deep breathing exercises. Avoid stimulating activities or screens close to bedtime.
By implementing these strategies, you can create a sleep-friendly environment that promotes better sleep quality and reduces the likelihood of experiencing sleep paralysis. Remember, it’s important to address the underlying causes of sleep paralysis, but optimizing your sleep environment can contribute to overall better sleep hygiene and well-being.
Medical Interventions
Medical interventions can be beneficial for individuals experiencing frequent and debilitating episodes of sleep paralysis. If sleep paralysis is significantly impacting one’s daily life and sleep quality, it may be necessary to consult a healthcare professional for further assessment and guidance. There are several potential medical interventions that can be considered.
One possible option is medication. In some cases, doctors may prescribe certain medications to help regulate sleep patterns and reduce the occurrence of sleep paralysis. These medications can include antidepressants, as they can help regulate sleep cycles and reduce the frequency of REM sleep disruptions. However, it is important to note that medication should be approached cautiously and under the guidance of a healthcare professional, as each individual’s situation is unique.
Another medical intervention that can be considered is therapy. Cognitive-behavioral therapy (CBT) can be effective in helping individuals manage the anxiety and fear associated with sleep paralysis. CBT focuses on identifying and challenging negative thought patterns and behaviors, providing practical coping strategies, and promoting relaxation techniques. By addressing the psychological aspects of sleep paralysis, therapy can aid in reducing the frequency and intensity of episodes.
In some cases, medical interventions may also involve treating any underlying sleep disorders that contribute to sleep paralysis. For example, if sleep apnea or narcolepsy is present, these conditions should be appropriately managed through the use of continuous positive airway pressure (CPAP) machines or medications, respectively. By addressing the underlying sleep disorder, the occurrence of sleep paralysis may be minimized.
It is important to emphasize that medical interventions should be approached on an individual basis. Each person’s experience with sleep paralysis is unique, and the appropriate course of action will depend on various factors. Seeking professional guidance and discussing the available options is crucial to determine the most suitable approach.
While medical interventions can be helpful, it is essential to remember that they are not the only solution. Adopting healthy sleep habits, managing stress levels, and creating a sleep-friendly environment are also crucial components in reducing the frequency and severity of sleep paralysis episodes. Combining medical interventions with self-care strategies can provide a more comprehensive approach to managing sleep paralysis and improving overall sleep quality.
Conclusion
In conclusion, sleep paralysis is a fascinating and often unsettling phenomenon that affects many individuals during their sleep-wake transitions. It is characterized by temporary muscle paralysis and a sense of being unable to move or speak, accompanied by hallucinations and a feeling of pressure. While sleep paralysis itself is not considered a sleep disorder, it can be indicative of underlying issues such as sleep disorders, irregular sleep patterns, stress, and sleep deprivation. Managing sleep paralysis involves establishing a consistent sleep schedule, practicing stress management techniques, avoiding stimulants and alcohol before bed, and creating a sleep-friendly environment. In some cases, medical interventions may be necessary to address the underlying causes of sleep paralysis. By understanding the causes, symptoms, and potential treatments, individuals can take steps towards improving their sleep quality and reducing the frequency of sleep paralysis episodes. So, if you or someone you know experiences sleep paralysis, remember that there are ways to cope and alleviate its impact on your well-being.
Frequently Asked Questions
1. What are the main causes of sleep paralysis?
Sleep paralysis can be caused by a variety of factors, including sleep disorders, irregular sleep patterns, stress and anxiety, sleep deprivation, and sleeping on your back.
2. How common is sleep paralysis?
Sleep paralysis is more common than you might think, affecting approximately 8% of the general population. However, some individuals may experience it more frequently than others.
3. Can sleep paralysis be prevented?
While it may not be possible to completely prevent sleep paralysis, there are steps you can take to reduce the likelihood of experiencing it, such as maintaining a regular sleep schedule, managing stress levels, and creating a sleep-friendly environment.
4. Is sleep paralysis dangerous?
Sleep paralysis itself is not dangerous, but the feelings of terror and panic that may accompany it can be distressing. It’s important to remember that sleep paralysis is a temporary condition and poses no long-term health risks.
5. Can medication help with sleep paralysis?
There are no specific medications designed to treat sleep paralysis directly. However, if the underlying cause of sleep paralysis is a sleep disorder, such as narcolepsy, medication prescribed for that disorder may help alleviate symptoms.
6. Can sleep paralysis occur during daytime naps?
Yes, sleep paralysis can occur both during nighttime sleep and daytime naps. The transition between wakefulness and sleep is a common trigger for sleep paralysis, regardless of the time of day.
7. Can sleep paralysis be hereditary?
While there is no definitive evidence suggesting a direct genetic link to sleep paralysis, there may be a genetic predisposition to certain sleep disorders or conditions that can contribute to its occurrence.
8. Is there a relationship between sleep paralysis and lucid dreaming?
There is a potential connection between sleep paralysis and lucid dreaming. Some individuals may enter a state of sleep paralysis immediately after becoming aware within a dream, resulting in the perception of being awake but unable to move.
9. Can changing sleep positions prevent sleep paralysis?
Changing sleep positions, particularly avoiding sleeping on your back, may help reduce the likelihood of experiencing sleep paralysis. Sleeping on your side or stomach can help minimize the occurrence of episodes.
10. Does everyone who experiences sleep paralysis have hallucinations?
No, not everyone who experiences sleep paralysis will have hallucinations. Hallucinations can be present in some individuals, but others may only experience the temporary inability to move or speak without any accompanying visual or auditory disturbances.