Restless Leg Syndrome: Unlocking the Secrets Behind the Unsettling Sensations
Do you find yourself constantly plagued by an irresistible urge to move your legs, especially when you’re trying to relax or get some much-needed rest? You may be suffering from Restless Leg Syndrome (RLS), a neurological disorder that affects millions of people worldwide. This perplexing condition can have a significant impact on your quality of life, leaving you drained and frustrated. In this article, we will delve deeper into the causes, symptoms, and treatment options for RLS. Join us as we unravel the mysteries of this unsettling sensation and discover ways to find relief.
What is Restless Leg Syndrome?

Restless Leg Syndrome, also known as Willis-Ekbom Disease, is a neurological disorder characterized by an irresistible urge to move the legs accompanied by uncomfortable sensations. These sensations are often described as creeping, crawling, tingling, or burning, and can range from mild to unbearable. The symptoms typically worsen during periods of rest or inactivity, particularly in the evenings and at night, leading to sleep disturbances and insomnia. While RLS commonly affects the legs, it can also manifest in other parts of the body, such as the arms or torso. It is estimated that around 10% of the population suffers from this condition, with women being more commonly affected than men. Although RLS can develop at any age, it is more prevalent in middle-aged and older individuals. Despite its widespread occurrence, RLS remains a relatively unknown and often misdiagnosed condition, leading to many misconceptions and myths surrounding its cause and treatment
Definition
The definition of Restless Leg Syndrome (RLS) refers to a neurological disorder characterized by an irresistible urge to move the legs, usually accompanied by uncomfortable sensations. These sensations can be described as tingling, creeping, pulling, or burning, and they typically occur in the evening or at night when the individual is at rest or trying to sleep. The discomfort experienced with RLS can range from mild to severe, and it can have a significant impact on the individual’s quality of life, leading to sleep disturbances and daytime fatigue. RLS is often categorized as a sleep disorder since it commonly disrupts sleep patterns. It is important to note that RLS can also affect other parts of the body, such as the arms or torso, although the legs are the most commonly involved. To learn more about how RLS affects children, you can read our article on restless leg syndrome in children.
Prevalence
Prevalence:
Restless Leg Syndrome (RLS) is a relatively common condition that affects a significant portion of the population. It is estimated that around 10% of adults worldwide suffer from RLS, making it a widespread neurological disorder. The prevalence of RLS varies among different age groups and demographics. Studies have shown that the prevalence of RLS tends to increase with age, with the highest rates observed in individuals over the age of 60. Gender also plays a role, as women are generally more prone to developing RLS than men. Certain medical conditions and lifestyle factors can influence the likelihood of developing RLS. For example, individuals with conditions such as iron deficiency, kidney disease, diabetes, and Parkinson’s disease are more likely to experience RLS symptoms. It’s important to note that RLS can also occur in children, although it is less common compared to adults. If you’d like to learn more about RLS in children, you can explore our article on Restless Leg Syndrome in Children.
Causes of Restless Leg Syndrome

The exact cause of Restless Leg Syndrome (RLS) is still not fully understood. However, researchers have identified several factors that may contribute to the development of this condition. One potential cause is genetics. There is evidence to suggest that RLS can run in families, with certain genetic variations increasing the risk of developing the disorder. Another significant factor is iron deficiency. Research has shown that low levels of iron in the brain may disrupt the normal functioning of dopamine, a neurotransmitter involved in controlling movement. Medications and substances such as antidepressants, antihistamines, and certain anti-nausea drugs have also been linked to the onset or worsening of RLS symptoms. Additionally, underlying conditions such as kidney failure, diabetes, and peripheral neuropathy can trigger or exacerbate RLS. It is important to note that anxiety and stress can worsen RLS symptoms, but they are not considered direct causes of the condition. Understanding the possible causes of RLS is crucial for effective management and treatment.
Genetics
Genetics:
Research suggests that genetics may play a role in the development of Restless Leg Syndrome. Studies have shown that individuals with a family history of RLS are more likely to experience the condition themselves. In fact, approximately half of those diagnosed with RLS have a first-degree relative who also suffers from the disorder. Scientists have identified specific gene variants that are associated with an increased susceptibility to RLS, such as the BTBD9 gene and the MEIS1 gene. These genetic factors are thought to contribute to abnormalities in the dopamine system, a neurotransmitter involved in movement and muscle control. While the exact mechanisms linking genetics and RLS are still being investigated, the hereditary nature of the condition highlights the importance of recognizing familial patterns and considering genetic predisposition when evaluating patients. Understanding the genetic component of RLS can help guide further research and contribute to the development of more targeted treatments in the future.
Iron Deficiency
Iron deficiency is considered to be one of the leading causes of Restless Leg Syndrome (RLS). Iron plays a critical role in the production of dopamine, a neurotransmitter involved in controlling movement and sensory perception. When iron levels in the body are deficient, there is a disruption in dopamine regulation, leading to the development of RLS symptoms. Studies have shown that individuals with RLS often have lower levels of iron in their brain and peripheral tissues compared to those without the condition. Research has found a correlation between low iron stores and the severity of RLS symptoms. In some cases, correcting the iron deficiency through supplementation or dietary changes can alleviate the symptoms of RLS. However, it’s important to note that not all RLS cases are linked to iron deficiency, and treatment approaches may vary depending on the underlying cause of the condition. To learn more about the connection between RLS and anxiety, check out our article on “/exploration-rls-anxiety/“. Additionally, it’s crucial to debunk common myths surrounding RLS and its treatment options. Check out our article on “/restless-leg-syndrome-myths/” to separate fact from fiction.
Medications and Substances
Medications and Substances:
There are several medications and substances that have been found to contribute to or exacerbate Restless Leg Syndrome (RLS) symptoms. It is important to note that not everyone who takes these medications or substances will develop RLS, but they may increase the risk or severity of symptoms.
1. Antidepressants: Certain antidepressant medications, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), have been associated with RLS symptoms. These medications affect the levels of neurotransmitters in the brain, which can trigger or worsen the uncomfortable sensations and urge to move.
2. Antipsychotics: Some antipsychotic medications, including haloperidol and risperidone, have been linked to RLS symptoms. These drugs alter dopamine levels in the brain, which plays a role in the regulation of movement and can contribute to RLS symptoms.
3. Anti-nausea drugs: Medications used to treat nausea, such as metoclopramide and prochlorperazine, have been known to trigger or worsen RLS symptoms. These drugs work by blocking dopamine receptors in the brain, which can disrupt the normal dopamine signaling and lead to RLS symptoms.
4. Caffeine and tobacco: Substances like caffeine and tobacco have stimulant properties that can interfere with sleep quality and exacerbate RLS symptoms. These substances can also disrupt the normal dopamine balance in the brain, contributing to RLS symptoms.
5. Certain cold and allergy medications: Some over-the-counter cold and allergy medications that contain antihistamines, such as diphenhydramine, can worsen RLS symptoms. These medications have sedating effects and can disrupt sleep patterns, making RLS symptoms more prominent.
If you are taking any medications or using substances that you suspect may be worsening your RLS symptoms, it is important to consult with your healthcare provider. They can help determine if there are suitable alternatives or adjustments that can be made to alleviate your symptoms.
Underlying Conditions
Restless Leg Syndrome (RLS) can sometimes be linked to certain underlying conditions or factors that contribute to its development. One such condition is iron deficiency, as low levels of iron in the brain can disrupt dopamine activity, which plays a crucial role in controlling muscle movement. This disruption can lead to the characteristic symptoms of RLS. Additionally, chronic diseases such as kidney failure, diabetes, and peripheral neuropathy have been associated with an increased risk of developing RLS. These conditions can affect the nerves and blood flow to the limbs, contributing to the uncomfortable sensations experienced by individuals with RLS. Other factors that may contribute to RLS include pregnancy, where hormonal and circulatory changes can trigger symptoms, and certain medications like antipsychotics and antidepressants, which can exacerbate or cause RLS symptoms to occur. It is important to address and manage any underlying conditions that may be contributing to the development of RLS in order to effectively treat and alleviate its symptoms.
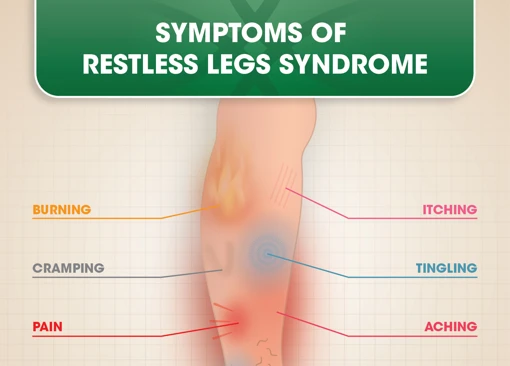
Common Symptoms
- Uncomfortable Sensations: The hallmark symptom of Restless Leg Syndrome is the presence of uncomfortable sensations in the legs, such as aching, itching, or crawling. These sensations can vary in intensity and may be accompanied by a deep sense of restlessness.
- Urge to Move the Legs: Individuals with RLS often experience an overwhelming urge to move their legs to relieve the uncomfortable sensations. The need to move is often described as involuntary, and providing temporary relief through movement is one of the key distinguishing features of this condition.
- Worsening Symptoms at Rest: Rest and inactivity tend to exacerbate the symptoms of RLS. Typically, the uncomfortable sensations and urge to move intensify when the affected individual is at rest or trying to fall asleep, causing significant disruption to sleep patterns and leading to daytime fatigue.
These common symptoms can significantly impact daily life, making it difficult to relax, concentrate, or engage in activities that require prolonged periods of inactivity. It’s important to note that the severity and frequency of symptoms can vary among individuals and may fluctuate over time, with some experiencing sporadic episodes while others have chronic symptoms. If you suspect you may be experiencing these symptoms, it is advisable to consult a healthcare professional for a proper diagnosis and appropriate management.
Uncomfortable Sensations
Uncomfortable Sensations: Deciphering the Disturbing Feelings of Restless Leg Syndrome
One of the hallmark symptoms of Restless Leg Syndrome (RLS) is the presence of uncomfortable sensations in the affected limbs. Individuals with RLS often describe these sensations as a variety of unpleasant feelings, such as crawling, creeping, tingling, or burning. The sensations can range in intensity from mild to severe and can be difficult to put into words. Some individuals compare the sensations to having insects crawling on their skin or experiencing an electric current running through their limbs. The uncomfortable feelings are typically localized in the legs, but they can also occur in the arms or torso in rare cases. These sensations can be quite distressing and disrupt daily activities, especially during periods of rest or relaxation when the urge to move the legs intensifies. It’s important to remember that these uncomfortable sensations are not caused by external factors and are a result of the underlying neurological dysfunction.
Urge to Move the Legs
The hallmark symptom of Restless Leg Syndrome (RLS) is the intense and overwhelming urge to move the legs. This sensation is often accompanied by an uncomfortable feeling deep within the muscles, making it difficult to resist the urge to constantly move or fidget the legs. The urge to move is usually preceded by an unpleasant sensation that can be best described as a creeping or crawling feeling. Some individuals may also experience aching, throbbing, or tingling sensations in their legs. The urge to move the legs is temporarily relieved by movement and activity but returns once the legs are at rest again. This can make it particularly difficult to relax or fall asleep, leading to sleep disruptions and fatigue. It’s important to note that the urge to move the legs is not solely driven by discomfort but is a neurological response linked to the underlying causes of RLS.
Worsening Symptoms at Rest
One of the hallmark features of Restless Leg Syndrome is the worsening of symptoms at rest. Individuals with RLS may experience an increase in the uncomfortable sensations and urge to move their legs when they are sitting or lying down, especially during periods of relaxation or inactivity. This can present significant challenges when trying to unwind in the evening or get a good night’s sleep. The exact reason why symptoms worsen at rest is not fully understood, but several theories have been proposed. One theory suggests that the decreased level of physical activity during rest triggers the release of neurotransmitters, such as dopamine, that are involved in controlling movement. Another theory suggests that the body’s typical circadian rhythm, or sleep-wake cycle, may play a role in the exacerbation of symptoms. Additionally, some studies have suggested a possible link between RLS and anxiety, with increased anxiety levels contributing to the intensification of symptoms at rest. Although these mechanisms are still being explored, what is clear is the effect of worsening symptoms at rest can significantly impact an individual’s quality of life, leading to sleep disturbances, daytime fatigue, and increased emotional distress.
Diagnosing Restless Leg Syndrome

Diagnosing Restless Leg Syndrome (RLS) can be challenging since there is no definitive test to confirm its presence. However, healthcare professionals follow a specific process to determine if a patient has RLS. The diagnosis primarily relies on the individual’s medical history, symptoms, and physical examination.
During the medical history assessment, the doctor will inquire about the nature of the discomfort, when it occurs, and how it affects the patient’s sleep patterns. They will also explore any underlying health conditions or medications that could potentially contribute to the development of RLS.
A physical examination may be conducted to rule out other possible causes of the symptoms. The doctor will evaluate the patient’s legs for any signs of swelling, redness, or underlying medical conditions. In some cases, a blood test may be recommended to check for iron deficiency or other abnormalities that could be related to RLS.
In certain situations, a sleep study, known as a polysomnography, might be conducted. This study records brain waves, oxygen levels, and muscle movements during sleep. This procedure helps to distinguish RLS from other sleep disorders and provides valuable insights into the severity of symptoms.
It is crucial to communicate openly with your healthcare provider and provide accurate information about your symptoms and medical history. Proper diagnosis is essential to ensure appropriate treatment and management of RLS symptoms.
Medical History and Symptoms
Medical History and Symptoms:
When diagnosing Restless Leg Syndrome (RLS), healthcare professionals typically begin by taking a detailed medical history and carefully evaluating the symptoms. Patients are asked to provide information about the frequency, duration, and intensity of their leg discomfort or sensations. Descriptions of the sensations, such as crawling, tingling, or burning, can help differentiate RLS from other conditions. Additionally, healthcare providers inquire about any triggers or factors that may worsen or alleviate the symptoms, including physical activity, rest, or specific medications. It is important to note any family history of RLS, as there is a strong genetic connection. Healthcare professionals may inquire about any underlying medical conditions, such as iron deficiency or kidney problems, which are associated with RLS. A thorough medical history is crucial in determining the likelihood of RLS and forming the basis for an accurate diagnosis.
Physical Examination
During a physical examination, the healthcare provider will assess the patient’s legs and overall musculoskeletal system to rule out other possible causes of the symptoms. The examination may involve checking for signs of peripheral neuropathy, checking for muscle weakness or atrophy, and assessing joint flexibility and range of motion. The healthcare provider may also perform a sensory examination to evaluate for any abnormalities in sensation. Additionally, they may look for any visible signs of skin conditions or inflammation that may be contributing to the symptoms. It is important to note that while a physical examination can help rule out other conditions, there is no specific diagnostic test for RLS. The diagnosis of RLS is primarily based on the patient’s reported symptoms and medical history, in combination with the exclusion of other potential causes through physical examination and other diagnostic tests.
Sleep Study
A sleep study, also known as polysomnography, is a diagnostic test used to evaluate and monitor various sleep disorders, including Restless Leg Syndrome (RLS). During a sleep study, a patient spends the night at a sleep center or hospital while their sleep patterns and brain activity are monitored. The study involves attaching electrodes to the scalp, face, chest, and legs to measure brain waves, eye movements, muscle activity, and heart rate. These measurements provide valuable information about the quality and stages of sleep a person experiences. For individuals suspected of having RLS, specific attention is given to the leg movements during the study. A sleep study can detect the presence of periodic limb movements of sleep (PLMS), which are characteristic of RLS. PLMS are repetitive, involuntary movements of the legs that occur during sleep and can disrupt sleep continuity. The sleep study results, along with the patient’s medical history and symptoms, assist healthcare professionals in confirming a diagnosis of RLS and determining the most appropriate treatment plan. It is important to note that while a sleep study can be helpful in diagnosing RLS, it is not always necessary for everyone experiencing symptoms.
Treating Restless Leg Syndrome
Finding relief from the symptoms of Restless Leg Syndrome (RLS) can greatly improve your quality of life and help you regain control over your sleep patterns. Treatment options for RLS are aimed at managing and reducing the severity of symptoms. Here are some approaches that may be recommended:
Lifestyle Changes: Making certain lifestyle modifications can often alleviate RLS symptoms. Regular exercise, such as walking or stretching, can help reduce discomfort and improve sleep quality. Avoiding caffeine, nicotine, and alcohol close to bedtime may also help minimize symptoms. Additionally, practicing good sleep hygiene, such as maintaining a regular sleep schedule and creating a relaxing bedtime routine, can promote better sleep.
Medications: In more severe cases, medications may be prescribed to manage RLS symptoms. Dopamine agonists, such as pramipexole or ropinirole, are often used as first-line treatment options. These medications work by increasing dopamine levels in the brain, which helps alleviate the uncomfortable sensations and reduce the urge to move the legs. Other medications, such as gabapentin or opioids, may be considered if dopamine agonists are ineffective or not tolerated.
Alternative Therapies: Some individuals find relief from RLS symptoms through complementary and alternative therapies. These may include acupuncture, massage, yoga, or meditation. While the effectiveness of these therapies may vary from person to person, they can provide a natural and holistic approach to managing RLS symptoms.
It is important to consult with a healthcare professional before starting any treatment regimen, as they can provide personalized recommendations and guidance based on the severity of your symptoms and overall health. By actively managing and treating RLS, you can regain control over your sleep and improve your daily well-being.
Lifestyle Changes
Making certain lifestyle modifications can play a crucial role in managing Restless Leg Syndrome (RLS) symptoms. Here are some changes that you can incorporate into your daily routine:
1. Regular Exercise: Engaging in regular physical activity can help reduce RLS symptoms. Consider activities such as walking, jogging, swimming, or cycling. Exercise promotes better circulation and releases endorphins, which can contribute to a more restful sleep.
2. Establish a Consistent Sleep Schedule: Maintaining a consistent sleep schedule can help regulate your body’s internal clock and improve sleep quality. Aim for a set bedtime and wake-up time each day.
3. Practice Good Sleep Hygiene: Create a sleep-friendly environment by ensuring your bedroom is cool, dark, and quiet. Avoid stimulating activities, such as watching TV or using electronic devices, close to your bedtime.
4. Avoid Triggers: Identify and avoid triggers that worsen your RLS symptoms. These may include certain medications, caffeine, tobacco, and alcohol. Keeping a journal to track your symptoms can help identify any patterns or triggers.
5. Incorporate Relaxation Techniques: Engaging in relaxation techniques, such as deep breathing exercises, meditation, or yoga, can help reduce stress and promote a sense of calmness, potentially alleviating RLS symptoms.
6. Massage and Heat Therapy: Gently massaging your legs or applying heat to the affected areas can provide temporary relief. Experiment with warm baths, heating pads, or hot water bottles to find what works best for you.
It’s important to remember that lifestyle changes may not completely eliminate RLS symptoms but can significantly improve your overall well-being. Consulting with a healthcare professional can help tailor a personalized plan and provide additional guidance for managing RLS effectively.
Medications
Medications:
When it comes to treating Restless Leg Syndrome (RLS), medications can play a crucial role in managing the symptoms and improving quality of life. There are several types of medications that doctors may prescribe, depending on the severity and specific needs of the individual. Here are some commonly used medications for RLS:
1. Dopamine Agonists: These medications work by increasing dopamine levels in the brain, which helps to regulate movement and reduce the symptoms of RLS. Examples of dopamine agonists include pramipexole, ropinirole, and rotigotine. It is important to note that these medications may cause side effects such as nausea, dizziness, and daytime sleepiness.
2. Benzodiazepines: These drugs are commonly prescribed to help improve sleep and reduce muscle spasms. They work by enhancing the effects of GABA, a neurotransmitter that promotes relaxation. Clonazepam and diazepam are examples of benzodiazepines that may be used in RLS treatment. However, these medications should be used with caution due to the risk of dependence and sedation.
3. Gabapentinoids: Drugs like gabapentin and pregabalin are commonly used to treat neuropathic pain and can also be effective in relieving RLS symptoms. They work by reducing the abnormal electrical activity in the nerves, thereby alleviating discomfort and improving sleep quality. These medications may cause drowsiness, dizziness, and weight gain.
4. Opioids: In cases of severe RLS that do not respond to other treatments, opioids may be prescribed. Opioids are powerful painkillers that can help relieve the discomfort associated with RLS. However, they are typically reserved for short-term use due to the potential for dependence and other side effects.
It is important to consult with a healthcare professional to determine the most appropriate medication and dosage for your specific case of RLS. They will consider factors such as your overall health, other medications you may be taking, and any potential interactions or contraindications. Regular follow-up appointments will also be necessary to monitor the effectiveness of the medication and make any necessary adjustments.
Alternative Therapies
Alternative Therapies: While conventional treatments play a crucial role in managing Restless Leg Syndrome (RLS), alternative therapies offer additional options that may provide relief for individuals seeking alternative or complementary approaches. Acupuncture is one such therapy that involves the insertion of thin needles into specific points on the body to help restore the flow of energy and alleviate symptoms. Some anecdotal evidence suggests that acupuncture can effectively reduce the severity and frequency of RLS symptoms. Massage therapy is another alternative therapy that involves applying manual pressure and manipulation techniques to reduce muscle tension and improve circulation. This can help alleviate discomfort and promote relaxation, potentially alleviating RLS symptoms. Yoga and stretching exercises may also be beneficial for individuals with RLS. These practices help improve flexibility, reduce muscle stiffness, and promote relaxation, which can lead to a decrease in RLS symptoms. Practices like mindfulness meditation and aromatherapy may help manage stress and improve overall well-being, potentially reducing the impact of RLS on daily life. It’s important to note that while alternative therapies may offer relief for some individuals, it is crucial to consult with a healthcare professional before incorporating them into your treatment plan to ensure they are safe and appropriate for your specific situation.
Conclusion
In conclusion, Restless Leg Syndrome is a complex neurological disorder that can have a significant impact on an individual’s quality of life. While the exact cause of RLS is still not fully understood, research points to a combination of genetic, environmental, and physiological factors. It is important to recognize the common symptoms of RLS, such as uncomfortable sensations and the urge to move the legs, especially at rest. If you suspect you may have RLS, it is crucial to seek a medical diagnosis and explore treatment options to alleviate symptoms and improve sleep quality. Lifestyle changes, such as regular exercise, managing stress, and maintaining a healthy sleep routine, can play a significant role in managing RLS. Additionally, medications and alternative therapies can be helpful in reducing symptoms and promoting restful sleep. Remember, each individual experiences RLS differently, and finding the right treatment approach may involve trial and error. With proper diagnosis and a tailored treatment plan, individuals with RLS can find relief and regain control over their lives.
Frequently Asked Questions
1. Can children have Restless Leg Syndrome?
Yes, Restless Leg Syndrome can affect children as well. It is estimated that about 2% of children experience RLS symptoms. The condition may go undiagnosed in children due to difficulties in expressing their sensations accurately.
2. Is there a link between Restless Leg Syndrome and anxiety?
While Restless Leg Syndrome and anxiety can coexist, there is no direct causal relationship between the two. However, individuals with RLS may experience increased anxiety or stress due to the discomfort and disruption of sleep caused by the syndrome.
3. Are there any home remedies to alleviate Restless Leg Syndrome symptoms?
While there is no cure for RLS, certain lifestyle changes may help manage symptoms. These include regular exercise, avoiding caffeine and alcohol, implementing a consistent sleep schedule, and practicing relaxation techniques like yoga or meditation.
4. Can Restless Leg Syndrome be a sign of an underlying medical condition?
Yes, in some cases, RLS may be secondary to an underlying medical condition such as iron deficiency, peripheral neuropathy, kidney disease, or pregnancy. Treating the underlying condition can alleviate or improve RLS symptoms.
5. Does Restless Leg Syndrome only affect the legs?
While Restless Leg Syndrome primarily affects the legs, it can also affect other parts of the body, such as the arms, torso, or even the face. These sensations may vary in intensity and location.
6. Is Restless Leg Syndrome hereditary?
There is evidence to suggest that genetics plays a role in the development of Restless Leg Syndrome. If you have a family member with RLS, you might have an increased risk of developing the condition.
7. Can certain medications worsen Restless Leg Syndrome symptoms?
Yes, certain medications such as antihistamines, antidepressants, and antipsychotics can exacerbate Restless Leg Syndrome symptoms. If you suspect your medication is causing or worsening your RLS, consult with your healthcare provider for possible alternatives.
8. Can pregnancy cause Restless Leg Syndrome?
Yes, pregnancy can trigger or worsen Restless Leg Syndrome symptoms. Hormonal changes, iron deficiency, and increased blood volume during pregnancy are thought to contribute to the development of RLS in expectant mothers.
9. Can Restless Leg Syndrome be diagnosed through a sleep study?
A sleep study, also known as polysomnography, can be used to diagnose Restless Leg Syndrome. During the study, your leg movements and brain activity are monitored to assess the presence and severity of RLS.
10. Can Restless Leg Syndrome be cured?
While there is currently no cure for Restless Leg Syndrome, there are various treatment options available to manage the symptoms effectively. Lifestyle changes, medications, and alternative therapies can provide relief and improve the quality of life for individuals living with RLS.