Narcolepsy is a mysterious and perplexing disorder that affects the daily lives of those who have it. Struggling with sudden and uncontrollable bouts of sleepiness and fatigue, individuals with narcolepsy often find themselves overcoming overwhelming challenges. In this article, we will delve into the causes and symptoms of narcolepsy, shedding light on this enigmatic condition that impacts millions of people globally. Whether you are personally affected by narcolepsy or simply curious to learn more, this article will provide you with a comprehensive understanding of the disorder and its various aspects. So, let’s embark on this journey of discovery together and unravel the mysteries of narcolepsy.
What is Narcolepsy?

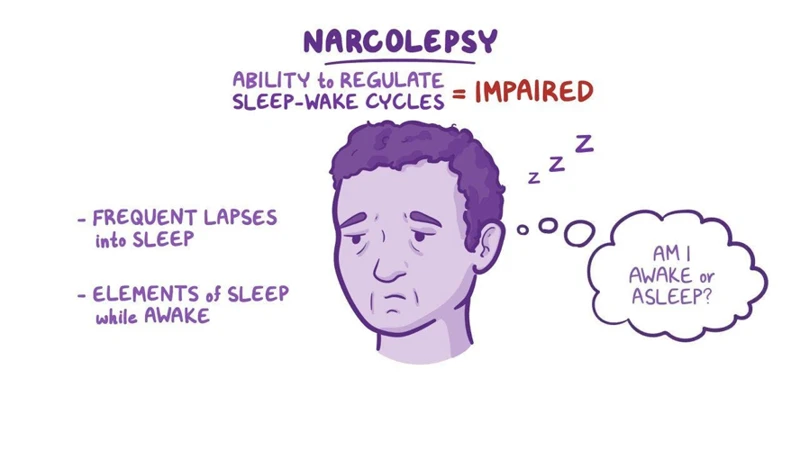
Narcolepsy is a neurological disorder characterized by excessive daytime sleepiness (EDS) and a disruption in sleep patterns. People with narcolepsy often experience sudden and uncontrollable sleep attacks during the day, making it difficult for them to stay awake and alert. These sleep attacks can happen at any time, regardless of the individual’s level of activity. In addition to EDS, narcolepsy may also manifest in other symptoms such as cataplexy, sleep paralysis, hallucinations, and fragmented sleep. Cataplexy refers to a sudden loss of muscle tone, often triggered by strong emotions. Sleep paralysis occurs when a person is unable to move or speak upon waking up or falling asleep. Hallucinations can be vivid and dream-like, occurring when a person is transitioning between sleep and wakefulness. Fragmented sleep, specifically disrupted rapid eye movement (REM) sleep, can lead to fragmented and non-restorative nighttime sleep. While the exact cause of narcolepsy is still not fully understood, research indicates that genetic factors, neurological abnormalities, and autoimmune reactions may all play a role in its development. Some studies suggest that certain genes may increase the risk of developing narcolepsy, although the exact inheritance pattern is still being investigated (/role-genetics-narcolepsy-inheritance/). There is growing recognition of the connection between narcolepsy and mental health, particularly in relation to dreaming and emotional well-being (/narcolepsy-mental-health-connection-dreaming-emotional-wellbeing/). Understanding narcolepsy and its various symptoms is essential for proper diagnosis and management of this disorder, which can greatly impact an individual’s quality of life.
Causes of Narcolepsy

The causes of narcolepsy are still not fully understood, but research has identified several factors that may contribute to the development of this neurological disorder. These include genetic factors, neurological abnormalities, and autoimmune reactions.
1. Genetic Factors: Studies have suggested that genetics may play a role in narcolepsy. Certain genes, such as the HLA-DQB1 gene, have been found to be associated with an increased risk of developing the disorder. However, it is important to note that not everyone with these genetic factors will develop narcolepsy, indicating that other factors are also involved in its development.
2. Neurological Abnormalities: Neurological abnormalities in the brain may also contribute to the development of narcolepsy. Specifically, a deficiency of the neurotransmitter hypocretin (also known as orexin) has been observed in individuals with narcolepsy. Hypocretin helps regulate wakefulness and REM sleep, and its deficiency can lead to excessive daytime sleepiness and fragmented sleep patterns.
3. Autoimmune Reactions: Some research suggests that narcolepsy may involve an autoimmune reaction in which the body’s immune system mistakenly attacks and destroys the cells that produce hypocretin in the brain. This autoimmune reaction may be triggered by environmental factors or infections, although the exact mechanisms are not yet fully understood.
While the exact causes of narcolepsy remain elusive, understanding these potential factors is crucial for advancing research and developing effective treatments for this complex disorder. Exploring famous narcolepsy success stories can also provide inspiration and hope for individuals living with narcolepsy (/famous-narcolepsy-success-stories/). By continuing to unravel the mysteries of narcolepsy, we can improve the lives of those affected and enhance our understanding of the human brain and sleep regulation.
1. Genetic Factors
Genetic factors are believed to play a significant role in the development of narcolepsy. Research has shown that certain genetic variations can increase a person’s susceptibility to the disorder. One of the main genetic factors associated with narcolepsy is the presence of specific variations in the HLA-DQB1 gene. This gene codes for a protein involved in the immune system, and variations in this gene have been found to be more common in individuals with narcolepsy. Specifically, a variation known as HLA-DQB1*06:02 has been strongly associated with an increased risk of developing narcolepsy with cataplexy. This genetic variation is found in a majority of individuals with narcolepsy type 1, which is characterized by the presence of cataplexy. It is important to note that while these genetic variations increase the risk of developing narcolepsy, they do not guarantee its occurrence. There is still much research being conducted to uncover the precise mechanisms by which these genetic factors contribute to the development of narcolepsy. By understanding the genetic factors involved, researchers hope to gain further insights into the underlying mechanisms of narcolepsy and potentially develop new diagnostic and therapeutic approaches.
2. Neurological Abnormalities
Neurological abnormalities play a significant role in the development of narcolepsy. Research suggests that there are specific areas of the brain that are involved in regulating sleep and wakefulness, and abnormalities in these regions can contribute to narcoleptic symptoms. One such area is the hypothalamus, which plays a crucial role in regulating the sleep-wake cycle. In individuals with narcolepsy, there is often a deficiency of a neuropeptide called hypocretin, also known as orexin, in the hypothalamus. Hypocretin is responsible for promoting wakefulness and regulating REM sleep. The lack of hypocretin in narcoleptic individuals leads to a dysregulation in the sleep-wake cycle, resulting in excessive sleepiness and disruptions in REM sleep. Another neurological abnormality associated with narcolepsy involves the neurotransmitter dopamine. Studies have shown that there may be an imbalance in dopamine levels in individuals with narcolepsy, which can contribute to the excessive daytime sleepiness experienced by these individuals. Additionally, abnormalities in other neurotransmitters such as serotonin, gamma-aminobutyric acid (GABA), and norepinephrine have also been observed in narcolepsy. These neurotransmitters play a crucial role in regulating various aspects of sleep and wakefulness. Understanding these neurological abnormalities in narcolepsy is essential for developing targeted treatments and interventions to manage the disorder effectively and improve the quality of life for those affected.
3. Autoimmune Reactions
Autoimmune reactions have been considered as one of the possible causes of narcolepsy. In individuals with narcolepsy, there is evidence of an autoimmune response that targets certain cells in the brain, specifically the orexin-producing cells in the hypothalamus. Orexin, also known as hypocretin, is a neurotransmitter that plays a crucial role in regulating wakefulness and sleep. Studies have shown that individuals with narcolepsy often have significantly lower levels of orexin in their cerebrospinal fluid compared to those without the condition. This deficiency in orexin is thought to be a result of autoimmune destruction of the orexin-producing cells. The exact trigger for this autoimmune response is not yet fully understood, but it is believed to involve a combination of genetic susceptibility and environmental factors. In some cases, viral infections have been associated with the development of narcolepsy, suggesting that an infection may act as a trigger for the autoimmune response. However, further research is needed to unravel the complex mechanisms underlying autoimmune reactions in narcolepsy. Understanding the role of autoimmune reactions in narcolepsy is crucial for developing targeted treatments that can help alleviate the symptoms and improve the quality of life for those affected by this chronic sleep disorder.
Symptoms of Narcolepsy

Symptoms of Narcolepsy:
1. Excessive Daytime Sleepiness (EDS): The hallmark symptom of narcolepsy is excessive daytime sleepiness, which is characterized by an overwhelming and persistent feeling of sleepiness throughout the day. Individuals with narcolepsy often find it difficult to stay awake and alert, even after getting a full night’s sleep. This constant state of sleepiness can significantly impact their daily functioning, making it challenging to concentrate, engage in activities, or maintain normal productivity.
2. Cataplexy: Cataplexy is another common symptom of narcolepsy, occurring in approximately 70% of individuals with the disorder. It refers to a sudden loss of muscle tone, often triggered by strong emotions such as laughter, excitement, or anger. During a cataplectic episode, affected individuals may experience temporary muscle weakness or even partial or complete paralysis. These episodes can range from mild, with drooping of the facial muscles, to severe, where a person may collapse completely.
3. Sleep Paralysis: Sleep paralysis is a temporary inability to move or speak that occurs when waking up from sleep or falling asleep. It is a somewhat terrifying experience, as individuals feel conscious but completely unable to move their body. Sleep paralysis often lasts for a few seconds to a couple of minutes and can be accompanied by hallucinations or a sense of impending doom.
4. Hallucinations: Narcolepsy can cause vivid and dream-like hallucinations, primarily during the transition between sleep and wakefulness. These hallucinations can seem incredibly realistic and may involve seeing people, animals, or objects that are not actually there. They can be quite disturbing, leading to feelings of fear or confusion.
5. Disrupted Nighttime Sleep: People with narcolepsy often experience disrupted nighttime sleep. They may have trouble falling asleep or staying asleep throughout the night. Wakefulness during the night can further contribute to excessive daytime sleepiness.
6. Fragmented Rapid Eye Movement (REM) Sleep: REM sleep fragmentation is another characteristic symptom of narcolepsy. REM sleep is the stage of sleep associated with dreaming, muscle paralysis, and rapid eye movements. In individuals with narcolepsy, REM sleep can occur almost immediately upon falling asleep, instead of following the usual sleep cycle pattern. This fragmentation can lead to frequent awakenings during the night and contribute to disrupted nighttime sleep.
Recognizing and understanding these symptoms is crucial for early detection and management of narcolepsy. If you or someone you know experiences these symptoms, it is essential to seek medical evaluation and consultation with a healthcare professional specializing in sleep disorders.
1. Excessive Daytime Sleepiness (EDS)
Excessive daytime sleepiness (EDS) is one of the defining symptoms of narcolepsy. It is characterized by an overwhelming and persistent feeling of drowsiness throughout the day, regardless of how much sleep a person gets at night. Individuals with narcolepsy often struggle to stay awake and alert, which can interfere with their daily activities, work, and social interactions. This excessive sleepiness can be debilitating and have a significant impact on a person’s overall quality of life. They may find themselves falling asleep in inappropriate situations, such as during meetings, while driving, or even in the middle of a conversation. The sleepiness experienced by individuals with narcolepsy is often described as an irresistible urge to sleep, and no amount of effort can effectively ward off these sleep attacks. The cause of EDS in narcolepsy is related to underlying neurological abnormalities that disrupt the normal sleep-wake cycle. These abnormalities can result in fragmented sleep patterns, preventing individuals with narcolepsy from obtaining restful and restorative sleep. It is important for those experiencing EDS to seek medical attention and proper diagnosis to manage their symptoms effectively. Treatment options, such as medications and lifestyle changes, will be discussed later in this article.
2. Cataplexy
Cataplexy is a unique symptom of narcolepsy that involves a sudden loss of muscle tone or control. It is often triggered by intense emotions such as laughter, surprise, anger, or excitement. When experiencing a cataplectic episode, individuals with narcolepsy may temporarily lose control of their muscles, leading to weakness or even complete collapse. The severity of cataplexy can vary from mild muscle weakness to a complete loss of muscle control, causing a person to fall to the ground. These episodes typically last for a few seconds to a couple of minutes. Although cataplexy is most commonly associated with narcolepsy type 1 (with cataplexy), it can also occur in a subset of individuals with narcolepsy type 2 (without cataplexy). It is important to note that cataplexy is not usually associated with loss of consciousness. This symptom can greatly affect a person’s daily life and may lead to social isolation or anxiety, as individuals may fear triggering an episode in public or embarrassing situations. Understanding and managing cataplexy is crucial in providing support and improving the overall quality of life for those living with narcolepsy.
3. Sleep Paralysis
Sleep paralysis is a frightening and often bewildering symptom experienced by individuals with narcolepsy. During sleep paralysis, a person is temporarily unable to move or speak, typically upon waking up or falling asleep. This immobilization can last for a few seconds up to a couple of minutes, causing significant distress and anxiety. During sleep paralysis episodes, people may feel a sense of pressure on their chest, as if someone is sitting on them or holding them down. They may also experience hallucinations, which can be vivid and realistic, adding to the feeling of terror. These hallucinations can involve seeing shadowy figures, hearing voices, or feeling a presence in the room. It is important to note that while sleep paralysis is more commonly associated with narcolepsy, it can also occur in individuals without narcolepsy as a result of sleep deprivation, irregular sleep schedules, or certain sleep disorders. Understanding the nature of sleep paralysis can provide reassurance and help individuals with narcolepsy better manage this unsettling symptom.
4. Hallucinations
Hallucinations are a distinct symptom of narcolepsy that can be both vivid and unsettling. These hallucinations occur during the awake state, typically when a person is transitioning between wakefulness and sleep. Known as hypnagogic hallucinations when they occur while falling asleep, and hypnopompic hallucinations when they occur while waking up, they can be visually and auditory in nature. People with narcolepsy may experience a range of hallucinations, from seeing shadowy figures or strange objects to hearing voices or sounds that aren’t really there. These hallucinations can feel incredibly real and can be accompanied by intense emotions. It’s important to note that hallucinations in narcolepsy are different from those associated with mental health conditions or drug use. They are a result of the brain’s abnormal transition between sleep and wakefulness. While hallucinations can be distressing, understanding their connection to narcolepsy can help individuals feel more at ease, knowing that they are a symptom of the disorder and not a sign of mental illness.
5. Disrupted Nighttime Sleep
Disrupted nighttime sleep is a common symptom experienced by individuals with narcolepsy. This sleep disturbance can have a significant impact on their overall well-being and daily functioning. One of the main contributors to disrupted nighttime sleep in narcolepsy is the fragmentation of Rapid Eye Movement (REM) sleep. REM sleep is the stage of sleep where most dreaming occurs. In individuals with narcolepsy, REM sleep can occur more frequently and at inappropriate times throughout the sleep cycle. This results in interrupted and fragmented sleep patterns, making it difficult for individuals to achieve deep, restorative sleep.
The disruptions in nighttime sleep can lead to several consequences. Individuals with narcolepsy may experience frequent awakenings during the night, leading to a sense of unrefreshing sleep. They may also have difficulty staying asleep for a continuous period, causing them to wake up multiple times throughout the night. As a result, they may feel fatigued and groggy during the daytime, exacerbating the excessive daytime sleepiness (EDS) that is characteristic of narcolepsy.
In addition to the fragmentation of REM sleep, other factors can further disrupt nighttime sleep in individuals with narcolepsy. These can include frequent awakenings due to vivid dreams or nightmares, frequent need to use the bathroom, or even the presence of other co-existing sleep disorders such as sleep apnea.
It is important to address and manage disrupted nighttime sleep in individuals with narcolepsy to improve their overall sleep quality and daytime functioning. Implementing good sleep hygiene practices such as maintaining a regular sleep schedule, creating a comfortable sleep environment, and avoiding stimulants and excessive daytime napping can help improve sleep continuity and quality.
Disrupted nighttime sleep is a significant symptom of narcolepsy, primarily caused by the fragmentation of REM sleep. Managing and addressing sleep disruptions are crucial for individuals with narcolepsy to improve their overall sleep quality and reduce excessive daytime sleepiness.
6. Fragmented Rapid Eye Movement (REM) Sleep
Fragmented Rapid Eye Movement (REM) sleep is a key symptom of narcolepsy that is characterized by disruptions in the normal sleep cycle. REM sleep is a stage of sleep where most vivid dreaming occurs and is crucial for restorative rest. In individuals with narcolepsy, this stage of sleep becomes fragmented, leading to frequent awakenings throughout the night. As a result, these individuals often experience a lack of restfulness and wake up feeling unrefreshed. The fragmented REM sleep can also contribute to the development of other narcolepsy symptoms, such as excessive daytime sleepiness (EDS) and hallucinations. During REM sleep, the body experiences temporary paralysis to prevent acting out dreams. However, in narcolepsy, this mechanism may become dysregulated, leading to episodes of sleep paralysis where individuals are unable to move or speak while transitioning between sleep and wakefulness. Fragmented REM sleep can have a significant impact on an individual’s overall sleep quality and can contribute to the chronic fatigue experienced by those with narcolepsy. Understanding and addressing this disruption in REM sleep is essential for managing and treating narcolepsy effectively.
Diagnosing Narcolepsy
Diagnosing Narcolepsy involves a comprehensive evaluation of a person’s symptoms and sleep patterns. A healthcare professional will typically consider the individual’s medical history, conduct a physical examination, and may refer the patient for specialized sleep studies.
1. Sleep Studies: Sleep studies, such as polysomnography, are commonly used to diagnose narcolepsy. This involves monitoring the individual’s brain waves, eye movements, muscle activity, and other physiological changes during sleep. It helps identify abnormalities in sleep patterns and ensures accurate diagnosis.
2. Multiple Sleep Latency Test (MSLT): The MSLT is a diagnostic test performed after overnight polysomnography. It measures a person’s tendency to fall asleep during the day and assesses the presence of excessive daytime sleepiness. The test consists of several nap opportunities throughout the day, during which the patient is monitored for signs of sleep onset.
In addition to these tests, a thorough assessment of the individual’s symptoms is crucial for making an accurate diagnosis. It is important to rule out other possible causes of excessive daytime sleepiness, such as sleep apnea or other sleep disorders.
Diagnosing narcolepsy can be challenging, as the symptoms can overlap with those of other conditions. It is essential to consult with a qualified healthcare professional who specializes in sleep disorders to ensure an accurate diagnosis and appropriate treatment.
1. Sleep Studies
Sleep studies are a crucial component in diagnosing narcolepsy. These studies, conducted in specialized sleep centers, involve monitoring an individual’s sleep patterns and brain activity during the night. There are several different types of sleep studies that can be performed to assess various aspects of sleep. One commonly used test is called polysomnography, which involves monitoring brain waves, eye movements, muscle activity, and heart rate during sleep. This test helps identify any abnormalities in sleep architecture and rule out other sleep disorders. Another test often used in diagnosing narcolepsy is the multiple sleep latency test (MSLT). This test is conducted during the day and measures the individual’s tendency to fall asleep and enter REM sleep during specified nap periods. During the MSLT, individuals are given several opportunities to take short naps at regular intervals, allowing the clinicians to evaluate their overall propensity for daytime sleepiness and the onset of REM sleep. The MSLT can help differentiate narcolepsy from other conditions that may cause excessive daytime sleepiness. In addition to sleep studies, medical history, physical examinations, and assessments of the individual’s symptoms are also taken into consideration for an accurate diagnosis of narcolepsy. It is important for individuals experiencing symptoms of narcolepsy to consult with a healthcare professional and undergo the necessary sleep studies to receive a proper diagnosis.
2. Multiple Sleep Latency Test (MSLT)
The Multiple Sleep Latency Test (MSLT) is a diagnostic tool commonly used to confirm a suspected diagnosis of narcolepsy. This test measures the speed at which a person falls asleep and enters rapid eye movement (REM) sleep during a series of scheduled naps throughout the day. The MSLT is typically performed after an overnight sleep study called a polysomnogram, which helps evaluate the individual’s overall sleep architecture and rule out other sleep disorders. During the MSLT, the person is instructed to nap at regular intervals usually every two hours in a dark and comfortable room. Electrodes are placed on the scalp to monitor brain wave activity, eye movements, and muscle tone. The test measures the time it takes for the person to fall asleep and enter REM sleep. A short latency period of less than 8 minutes is considered a strong indicator of narcolepsy. Additionally, the MSLT can help distinguish between narcolepsy type 1 (with cataplexy) and narcolepsy type 2 (without cataplexy). This test is crucial in the diagnostic process of narcolepsy and helps healthcare professionals determine the best treatment plan for individuals living with this condition.
Treating Narcolepsy
Treating narcolepsy involves a combination of medications and lifestyle changes to help manage the symptoms and improve overall quality of life. Medications used to treat narcolepsy aim to address the excessive sleepiness and other symptoms associated with the disorder. Stimulants, such as modafinil and amphetamines, are commonly prescribed to help promote wakefulness and combat daytime sleepiness. These medications work by stimulating the central nervous system and increasing alertness. Another medication option is sodium oxybate, which can help manage symptoms like cataplexy and improve overall nighttime sleep quality. Sodium oxybate is typically taken in two doses – one before bedtime and one during the night. In addition to medication, implementing certain lifestyle changes can further support narcolepsy management. Maintaining a consistent sleep schedule with regular sleep and wake times can promote better sleep and reduce symptoms. Taking scheduled short naps throughout the day can help alleviate excessive daytime sleepiness and improve overall alertness. Avoiding caffeine and heavy meals close to bedtime can help improve nighttime sleep quality. Regular exercise can also have a positive impact on sleep patterns and overall well-being. It’s important to work closely with a healthcare professional to determine the most appropriate treatment plan for managing narcolepsy symptoms effectively. Each individual’s treatment needs may vary, and regular follow-ups with a healthcare provider can help ensure the best outcomes for managing this chronic condition.
1. Medications
When it comes to treating narcolepsy, medications play a crucial role in managing the symptoms and improving overall wakefulness. There are several types of medications prescribed to individuals with narcolepsy, each targeting different aspects of the disorder.
Stimulants: Stimulant medications, such as modafinil and methylphenidate, are commonly prescribed to help promote wakefulness and reduce excessive daytime sleepiness. They work by stimulating the central nervous system and increasing alertness.
Sodium Oxybate: Sodium oxybate is a medication that is taken at night to improve nighttime sleep and reduce the occurrence of cataplexy. It helps consolidate sleep and reduce the frequency of sleep disruptions.
Antidepressants: Some antidepressant medications, particularly selective serotonin reuptake inhibitors (SSRIs) like fluoxetine, can be used to manage symptoms of cataplexy. These medications work by regulating serotonin levels in the brain and helping to prevent or reduce the severity of cataplectic episodes.
Other Medications: In certain cases, other medications may be prescribed to address specific symptoms or complications associated with narcolepsy. For example, medications may be prescribed to manage sleep paralysis, hallucinations, or other related conditions.
It is important to note that medication should be taken under the guidance and supervision of a healthcare professional, as they can determine the most suitable medication and dosage for each individual. Additionally, lifestyle changes, such as maintaining a regular sleep schedule, practicing good sleep hygiene, and managing stress levels, can also complement medication therapy and contribute to improved symptom management (/famous-narcolepsy-success-stories/).
2. Lifestyle Changes
Lifestyle changes can play a significant role in managing narcolepsy symptoms and improving overall quality of life for individuals with this disorder. While medications are often prescribed to help control symptoms, incorporating certain lifestyle adjustments can further enhance the effectiveness of treatment. Here are some lifestyle changes that can be beneficial for individuals with narcolepsy.
1. Establish a Consistent Sleep Schedule: Maintaining a regular sleep schedule is crucial for people with narcolepsy. Going to bed and waking up at the same time every day helps regulate the body’s internal clock and promotes better sleep quality.
2. Create a Sleep-Friendly Environment: Making adjustments to your sleep environment can contribute to more restful sleep. Ensure that your bedroom is cool, dark, and quiet. Consider using blackout curtains, earplugs, or a white noise machine to minimize disruptions.
3. Take Short, Scheduled Naps: Planned naps throughout the day can help manage excessive daytime sleepiness. These naps should be short (around 15-20 minutes) and strategically timed to prevent interfering with nighttime sleep.
4. Avoid Stimulants: Stimulants such as caffeine and nicotine can disrupt sleep patterns. It’s best to minimize or avoid their consumption, especially close to bedtime.
5. Engage in Regular Exercise: Regular physical activity can promote better sleep and overall well-being. Engage in moderate exercise, such as walking or swimming, for at least 30 minutes a day.
6. Maintain a Healthy Diet: A balanced diet can support energy levels and overall health. Incorporate nutritious foods, including fruits, vegetables, lean proteins, and whole grains into your meals.
7. Consider a Supportive Sleep Environment: If cataplexy is a symptom of your narcolepsy, it may be helpful to make some adjustments to your surroundings. Remove or secure any items that may cause injury during episodes of cataplexy.
By implementing these lifestyle changes, individuals with narcolepsy can better manage their symptoms, improve their sleep quality, and enhance their overall well-being. However, it’s important to consult with a healthcare professional for personalized advice and guidance in managing narcolepsy effectively.
Conclusion
In conclusion, narcolepsy is a complex and multifaceted disorder that can significantly impact the lives of those affected. While the exact causes of narcolepsy are still being researched, it is believed to involve a combination of genetic factors, neurological abnormalities, and autoimmune reactions. The symptoms of narcolepsy, such as excessive daytime sleepiness, cataplexy, sleep paralysis, hallucinations, disrupted nighttime sleep, and fragmented REM sleep, can be disruptive and challenging to manage. Proper diagnosis through sleep studies and the multiple sleep latency test (MSLT) is crucial for developing an effective treatment plan. Treatment options for narcolepsy may include medications to manage symptoms and lifestyle changes to improve sleep hygiene. Despite the challenges, it’s important to recognize that individuals with narcolepsy can still lead fulfilling lives with the right support and management strategies. Through ongoing research and awareness, we can continue to improve our understanding of narcolepsy and provide the necessary resources and support for those living with this condition.
Frequently Asked Questions
1. How common is narcolepsy?
Narcolepsy affects approximately 1 in 2,000 people, making it a relatively rare disorder.
2. At what age does narcolepsy typically onset?
Narcolepsy symptoms often begin to appear in adolescence or early adulthood, although it can occur at any age.
3. Can narcolepsy be inherited?
There is evidence to suggest that there may be a genetic component to narcolepsy. Certain genetic factors may increase the risk of developing the disorder, but it is not directly inherited in a predictable manner.
4. Is narcolepsy a form of insomnia?
No, narcolepsy is not a form of insomnia. Whereas insomnia is characterized by difficulty falling asleep or staying asleep, narcolepsy involves excessive daytime sleepiness and disrupted sleep patterns.
5. Can narcolepsy be cured?
Narcolepsy currently has no cure. However, symptoms can be managed with medication and lifestyle modifications to improve quality of life.
6. How is narcolepsy diagnosed?
Narcolepsy is typically diagnosed through a combination of clinical evaluation, medical history, and specialized sleep studies such as polysomnography and the Multiple Sleep Latency Test (MSLT).
7. Are there any famous individuals with narcolepsy?
Yes, there are well-known individuals who have openly spoken about their experiences with narcolepsy, including successful athletes, actors, and public figures (/famous-narcolepsy-success-stories/).
8. Can narcolepsy be mistaken for laziness?
Due to the excessive sleepiness associated with narcolepsy, it can sometimes be mistaken for laziness or lack of motivation. However, narcolepsy is a legitimate neurological disorder that requires proper understanding and support.
9. Can stress exacerbate narcolepsy symptoms?
Yes, stress can worsen narcolepsy symptoms. High levels of stress can trigger sleep attacks and increase the frequency of other symptoms such as cataplexy and sleep paralysis.
10. Does narcolepsy affect emotional well-being?
Narcolepsy can impact emotional well-being due to the unpredictable nature of symptoms and the challenges that individuals with narcolepsy may face on a daily basis. Seeking emotional support and therapeutic interventions can be beneficial (/narcolepsy-mental-health-connection-dreaming-emotional-wellbeing/).








