Welcome to the world of sleepless nights and restless minds. Insomnia is a pesky little problem that affects millions of people worldwide, leaving them tossing and turning in bed, desperate for a peaceful slumber. But fear not, for in this comprehensive article, we will delve into the depths of insomnia, exploring its causes, symptoms, and treatment options. Whether you’re a night owl struggling to drift off or a daytime zombie yearning for a refreshing sleep, this article will equip you with the knowledge and tools to conquer insomnia and reclaim your nights of blissful rest. So, fasten your seatbelts and prepare for a journey through the fascinating world of insomnia. Let’s uncover the secrets behind those sleepless nights and find the path to peaceful slumber.
What is Insomnia?
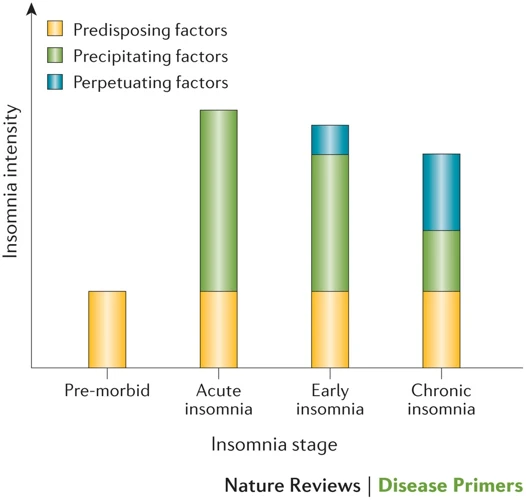
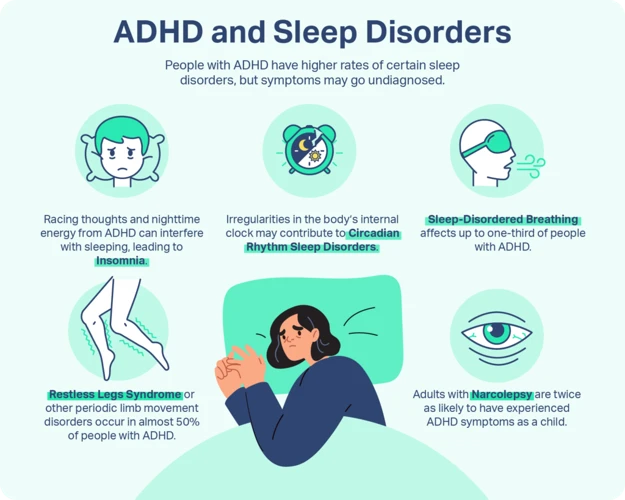
Insomnia, one of the most common sleep disorders, is characterized by the inability to initiate or maintain adequate sleep. It is a condition that affects both the quality and quantity of sleep, leaving individuals feeling tired and unrefreshed during the day. Insomnia can manifest in different ways, including difficulty falling asleep, frequent awakening throughout the night, waking up too early in the morning, or experiencing non-restorative sleep. When someone suffers from insomnia, it can have a significant impact on their overall well-being and quality of life. Insomnia can be acute, lasting for a short period, or chronic, lasting for several months or even years. While occasional episodes of insomnia are common and usually resolve on their own, chronic insomnia requires intervention and treatment to restore healthy sleep patterns and improve overall sleep quality.
There are various factors that can contribute to the development of insomnia. These may include lifestyle factors such as excessive caffeine or alcohol consumption, irregular sleep schedules, and high levels of stress. Medical conditions such as chronic pain, respiratory disorders, and hormonal imbalances can also disrupt sleep and lead to insomnia. Additionally, psychological factors like anxiety, depression, and certain psychiatric disorders can play a role in the onset and persistence of insomnia.
Understanding the causes of insomnia is crucial in order to address and manage the condition effectively. By identifying the underlying factors contributing to sleep disturbances, individuals can take appropriate steps to improve their sleep hygiene and seek appropriate treatment. In the following sections, we will explore the causes, symptoms, diagnosis, and treatment options for insomnia in detail, providing you with the knowledge and tools to better understand and manage this sleep disorder.
Internal Link: Unraveling Narcolepsy: Symptoms and Treatment
Causes of Insomnia
Insomnia can be caused by a variety of factors, including lifestyle choices, underlying medical conditions, and psychological factors. In terms of lifestyle factors, habits such as consuming excessive amounts of caffeine or alcohol, irregular sleep schedules, and poor sleep hygiene can contribute to the development of insomnia. Medical conditions such as chronic pain, respiratory disorders, gastrointestinal issues, and hormonal imbalances can also disrupt sleep and lead to insomnia. Additionally, psychological factors like stress, anxiety, depression, and certain psychiatric disorders can play a role in the onset and persistence of insomnia. Identifying the specific causes of insomnia is crucial in order to address and manage the condition effectively. By addressing lifestyle factors, seeking appropriate medical care, and managing psychological well-being, individuals can take steps to alleviate insomnia symptoms and improve sleep quality.
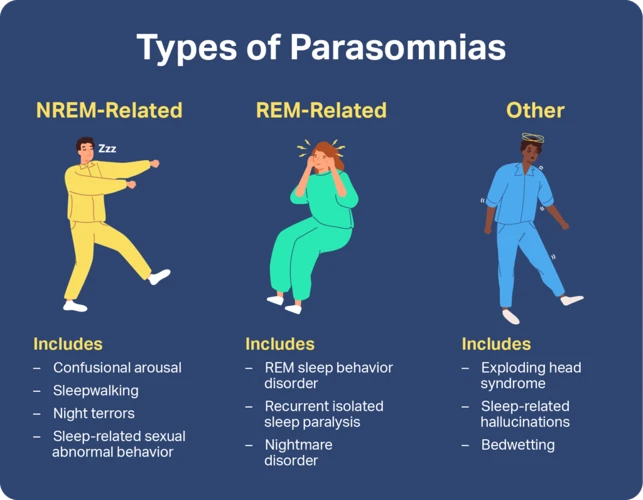
Internal Link: Sleepwalking: Causes, Risks, and Prevention Strategies
1. Lifestyle Factors
Lifestyle factors play a significant role in the development of insomnia. The choices we make in our daily routines and habits can have a direct impact on our ability to fall asleep and maintain a restful sleep throughout the night. Here are some common lifestyle factors that can contribute to insomnia:
1. Stress: Stress is a major culprit when it comes to sleep disturbances. High levels of stress can lead to racing thoughts, anxiety, and difficulty relaxing, making it challenging to fall asleep. It’s crucial to incorporate stress management techniques into your daily routine, such as practicing relaxation techniques, engaging in regular exercise, and prioritizing self-care activities.
2. Caffeine and Alcohol: Consuming caffeine in the late afternoon or evening can interfere with sleep. It is a stimulant that can keep you awake and disrupt your natural sleep-wake cycle. Similarly, while alcohol may initially make you feel drowsy, it can disrupt the quality of your sleep, causing frequent awakenings and a decrease in deep, restorative sleep.
3. Irregular Sleep Schedule: Erratic sleep patterns can throw off your body’s internal clock, making it difficult to fall asleep and wake up at consistent times. It’s important to establish a regular sleep schedule, going to bed and waking up at the same time each day, even on weekends.
4. Electronic Devices: The blue light emitted by electronic devices such as smartphones, tablets, and computers can interfere with your body’s production of melatonin, a hormone that regulates your sleep-wake cycle. Avoiding the use of electronic devices at least one hour before bedtime can help signal to your body that it’s time to wind down and prepare for sleep.
5. Environmental Factors: The sleeping environment plays a crucial role in promoting quality sleep. Factors such as excessive noise, uncomfortable mattress, or an unsupportive pillow can contribute to sleep disturbances. Creating a calming sleep environment with minimal noise, comfortable bedding, and a cool temperature can help improve your sleep quality.
By addressing and modifying these lifestyle factors, individuals can take proactive steps to improve their sleep hygiene and promote better sleep. Adopting healthy sleep habits, such as practicing relaxation techniques before bed, avoiding stimulants, maintaining a consistent sleep schedule, and creating a conducive sleep environment, can significantly reduce the likelihood of experiencing insomnia.
Internal Link: Understanding Sleep Paralysis: Causes, Symptoms, and Coping Strategies
2. Medical Conditions
Medical conditions can significantly contribute to the development of insomnia. Various physical ailments and disorders can disrupt sleep patterns, making it difficult to fall asleep or stay asleep throughout the night. Some common medical conditions associated with insomnia include:
1. Chronic Pain: Conditions such as arthritis, fibromyalgia, or back pain can cause discomfort that makes it challenging to find a comfortable position for sleep. The pain can interrupt sleep and lead to frequent awakenings, resulting in insomnia.
2. Respiratory Disorders: Conditions like asthma, chronic obstructive pulmonary disease (COPD), or sleep apnea can cause breathing difficulties during sleep. Sleep apnea, for example, results in periodic disruptions in breathing and can cause individuals to wake up numerous times throughout the night, leading to poor sleep quality and insomnia.
3. Gastroesophageal Reflux Disease (GERD): This chronic digestive disorder causes acid from the stomach to flow back into the esophagus, leading to heartburn and discomfort. Symptoms often worsen when lying down, making it challenging to sleep peacefully and increasing the likelihood of insomnia.
4. Neurological Disorders: Certain neurological conditions like Parkinson’s disease, Alzheimer’s disease, and multiple sclerosis can disrupt the normal sleep-wake cycle. These disorders may lead to fragmented sleep, frequent awakenings, and difficulty falling back asleep, ultimately resulting in insomnia.
5. Hormonal Imbalances: Hormonal changes, such as those experienced during menopause, can contribute to the development of insomnia. Fluctuations in hormone levels can disrupt sleep patterns and lead to night sweats, hot flashes, and other symptoms that interfere with sleep.
Managing insomnia caused by medical conditions often involves treating the underlying condition in addition to addressing the sleep disturbances. Seeking medical guidance and treatment for the specific medical condition can help alleviate the symptoms and improve sleep quality. Additionally, implementing good sleep hygiene practices, such as maintaining a regular sleep schedule, creating a comfortable sleep environment, and practicing relaxation techniques, can further support the management of insomnia linked to medical conditions.
3. Psychological Factors
Psychological factors play a significant role in the development and persistence of insomnia. Stress, anxiety, depression, and other mental health conditions can heavily impact sleep quality and contribute to the onset of insomnia. Here are some common psychological factors that can disrupt sleep patterns:
| Stress: | High levels of stress can keep the mind racing, making it difficult to relax and fall asleep. Stressful life events, such as work pressure, financial worries, or relationship problems, can all contribute to insomnia. |
| Anxiety: | Generalized anxiety disorder, panic disorder, post-traumatic stress disorder (PTSD), and other anxiety disorders can lead to racing thoughts, restlessness, and hyperarousal, making it challenging to achieve a calm state conducive to sleep. |
| Depression: | Depression often disrupts sleep patterns, leading to insomnia. Insomniacs with depression may experience difficulty falling asleep, early morning awakening, or fragmented sleep. Sleep disturbance is one of the key diagnostic criteria for major depressive disorder. |
| Other Mental Health Conditions: | Conditions such as bipolar disorder, schizophrenia, and postpartum depression can also affect sleep quality and duration, leading to insomnia in some cases. |
These psychological factors can create a cycle where lack of sleep exacerbates psychological distress, and in turn, the distress further worsens sleep quality, creating a vicious cycle of insomnia. It is essential to address and manage these psychological factors to break the cycle and improve sleep. Techniques such as relaxation exercises, stress management strategies, therapy, and medication, when necessary, can help individuals with insomnia related to psychological factors.
By understanding the impact of psychological factors on sleep and taking steps to manage them, individuals can work towards improving their sleep quality and overall well-being. Identifying and addressing any underlying psychological issues can be an important part of a comprehensive treatment plan for insomnia.
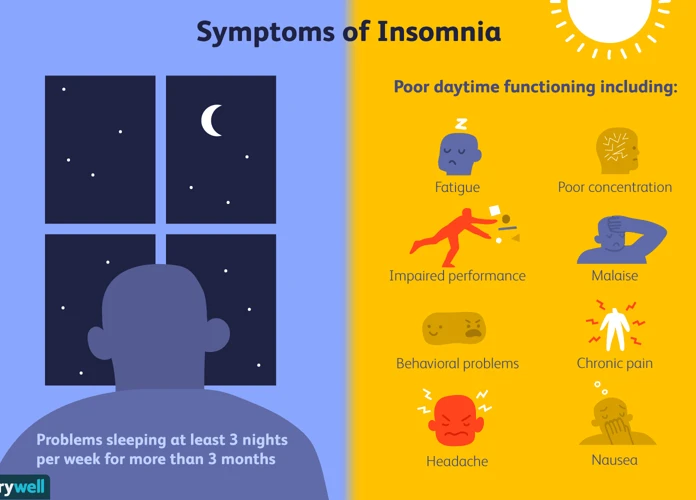
Symptoms of Insomnia
Insomnia is often characterized by a range of distressing symptoms that can significantly impact a person’s sleep and daily functioning. The most common symptoms of insomnia include difficulty falling asleep, where individuals may spend a significant amount of time tossing and turning before finally dozing off. Waking up frequently at night is another common symptom, disrupting the continuity of sleep and making it difficult to achieve deep, restful rest. Early morning awakening is yet another telltale sign of insomnia, where individuals wake up significantly earlier than desired and struggle to fall back asleep. Finally, non-restorative sleep is a frustrating symptom wherein individuals wake up feeling tired, groggy, and unrefreshed, despite having spent a significant amount of time in bed. These symptoms can lead to daytime fatigue, irritability, difficulty concentrating, and overall impairment in daily functioning. It is important to recognize and address these symptoms to effectively manage and treat insomnia.
1. Difficulty Falling Asleep
One of the hallmark symptoms of insomnia is difficulty falling asleep, also known as sleep onset insomnia. Individuals experiencing this type of insomnia may find themselves lying in bed for extended periods, unable to drift off into sleep. They may feel restless or agitated, with racing thoughts preventing them from entering a relaxed state conducive to sleep.
The causes of difficulty falling asleep can vary. Stress and anxiety are common culprits, as the mind becomes preoccupied with worries and thoughts, making it difficult to relax and transition into sleep. Other lifestyle factors, such as consuming caffeine or engaging in stimulating activities before bedtime, can also interfere with sleep onset. Additionally, certain medical conditions, such as chronic pain or respiratory disorders, can contribute to difficulty falling asleep.
To address difficulty falling asleep, implementing good sleep hygiene practices can be beneficial. These include establishing a consistent sleep schedule, creating a relaxing bedtime routine, and creating a sleep-friendly environment. Avoiding stimulating activities and electronics before bed, as well as limiting caffeine intake, can also help calm the mind and promote easier sleep onset.
If difficulty falling asleep persists and significantly impacts daily functioning, it is important to consult with a healthcare professional. They can provide a thorough evaluation, assess for any underlying medical or psychological factors, and recommend appropriate treatment options to address sleep onset insomnia effectively.
Internal Link: Sleep Paralysis: Causes, Symptoms, and Coping Strategies
2. Waking Up Frequently at Night
Waking up frequently at night is a common symptom experienced by those with insomnia. It refers to the repeated awakenings throughout the night, interrupting the natural sleep cycle and making it difficult to achieve restful sleep. This symptom can be a result of various factors, both external and internal.
External factors that contribute to waking up frequently at night include environmental disturbances, such as noise, light, or uncomfortable room temperature. These disruptions can jolt individuals out of their sleep and make it challenging to fall back asleep. Additionally, certain lifestyle choices, such as consuming stimulating substances like caffeine or nicotine close to bedtime, can also increase the likelihood of waking up during the night.
Internal factors, on the other hand, are often more closely linked to underlying health conditions and psychological factors. Physical ailments, such as chronic pain, gastrointestinal issues, or respiratory problems, can trigger awakenings throughout the night. Similarly, individuals with mental health conditions, including anxiety and depression, may experience intrusive thoughts, racing minds, or nightmares that wake them up repeatedly.
It is important to note that frequent awakenings at night can perpetuate a cycle of anxiety and frustration, as individuals become increasingly worried about their ability to get back to sleep. This heightened anxiety can further contribute to difficulties falling asleep and maintaining uninterrupted sleep.
Addressing the underlying causes of waking up frequently at night is essential for managing insomnia. Creating a sleep-friendly environment by minimizing distractions, implementing a relaxing bedtime routine, and practicing stress-reducing techniques can help improve sleep quality. Additionally, addressing any medical or psychological conditions through appropriate treatment is crucial in alleviating this symptom and achieving more restful nights.
By understanding the factors that contribute to waking up frequently at night, individuals can take proactive steps to improve their sleep habits and overall well-being. It is always recommended to consult with a healthcare professional to receive an accurate diagnosis and develop an individualized treatment plan.
Internal Link: Sleep Paralysis: Causes, Symptoms, and Coping Strategies
3. Early Morning Awakening
3. Early Morning Awakening:
Early morning awakening is a common symptom experienced by individuals with insomnia. It refers to the tendency to wake up earlier than desired and being unable to fall back asleep. This can occur as early as 4 or 5 in the morning, leaving individuals feeling groggy, fatigued, and unable to go back to sleep.
There are several potential causes for early morning awakening in individuals with insomnia. One possible explanation is an underlying disruption in the body’s internal circadian rhythm, which regulates sleep-wake cycles. When this rhythm is disrupted, it can lead to premature waking and difficulty returning to sleep.
Another contributing factor to early morning awakening may be related to stress and anxiety. Individuals experiencing high levels of stress or anxiety often find their minds racing with worry during the early hours of the morning, making it challenging to fall back asleep. The combination of intrusive thoughts and an increase in physiological arousal can further disrupt the sleep process.
Additionally, medical conditions such as sleep apnea, chronic pain, or certain psychiatric disorders can contribute to early morning awakening in individuals with insomnia. These conditions may cause discomfort or pain, leading to sleep disturbances and premature waking.
To address early morning awakening, individuals can try implementing good sleep hygiene practices. This includes establishing a regular sleep-wake schedule, creating a comfortable sleep environment, and practicing relaxation techniques before bedtime. Engaging in activities that promote relaxation, such as reading a book or taking a warm bath, can help calm the mind and prepare the body for sleep.
If early morning awakening persists despite these strategies, it may be beneficial to seek professional help. Cognitive-behavioral therapy for insomnia (CBTI) is a behavioral treatment approach that has shown promising results in helping individuals with insomnia, including those experiencing early morning awakening. CBTI focuses on identifying and modifying unhelpful thoughts and behaviors that contribute to sleep difficulties, helping individuals develop healthier sleep patterns.
Remember, if you consistently struggle with early morning awakening, it is essential to consult with a healthcare professional who can provide a comprehensive evaluation and recommend appropriate treatment options.
Internal Links: None.
4. Non-Restorative Sleep
Non-restorative sleep is a common symptom experienced by individuals with insomnia. It refers to a lack of feeling refreshed and rested after a night’s sleep. Even though a person may have spent an adequate amount of time in bed, they wake up feeling tired, fatigued, and unrefreshed. This can have a significant impact on their daytime functioning and overall quality of life.
There are several factors that can contribute to non-restorative sleep in individuals with insomnia. One of the main culprits is the quality of sleep. Even if someone with insomnia manages to fall asleep, they may experience disruptions throughout the night, such as frequent awakenings or difficulty staying asleep. These interruptions prevent them from getting the deep, restorative sleep that is necessary for feeling refreshed.
Another factor that can contribute to non-restorative sleep is the presence of other sleep disorders or medical conditions. Conditions such as restless legs syndrome, sleep apnea, or chronic pain can interfere with the quality of sleep and prevent individuals from experiencing restorative sleep.
Additionally, psychological factors can also play a role in non-restorative sleep. Stress, anxiety, and depression can disrupt sleep patterns and prevent individuals from reaching the restorative stages of sleep. This can leave them feeling tired and unrefreshed, even after a full night’s sleep.
Addressing non-restorative sleep in individuals with insomnia requires a comprehensive approach to managing the underlying causes. This may involve improving sleep hygiene practices, such as creating a relaxing bedtime routine and optimizing the sleep environment. Cognitive-behavioral therapy for insomnia (CBTI) is a highly effective treatment approach that focuses on changing negative thoughts and behaviors around sleep. It helps individuals develop healthy sleep habits and improve their overall sleep quality.
In cases where non-restorative sleep persists despite these interventions, it is important to consult a healthcare professional. They can assess for any underlying medical or psychiatric conditions that may be contributing to the problem and provide appropriate treatment.
Non-restorative sleep is a frustrating symptom of insomnia, but with the right strategies and interventions, it is possible to improve sleep quality and wake up feeling refreshed and rejuvenated.
Diagnosing Insomnia
Diagnosing insomnia involves a careful evaluation of an individual’s sleep patterns and medical history. The process typically begins with keeping a sleep diary for a certain period of time. This diary helps track sleep patterns, including the time the individual goes to bed, how long it takes to fall asleep, any awakenings during the night, and the overall quality of sleep. Alongside the sleep diary, a medical evaluation is conducted to rule out any underlying medical conditions or medications that may be contributing to the sleep disturbances. The evaluation may involve discussions about lifestyle factors, mental health, and physical symptoms. In some cases, a sleep study may be recommended to observe and measure various physiological aspects during sleep, such as brain waves, heart rate, and breathing patterns. These methods help healthcare professionals gather comprehensive information to accurately diagnose insomnia and determine the appropriate course of treatment.
1. Sleep Diary
A sleep diary is a valuable tool that can help diagnose and understand insomnia. It involves keeping a record of your sleep patterns and habits over a period of time, typically for a couple of weeks. The purpose of a sleep diary is to gather detailed information about your sleep-wake cycle, which can then be analyzed to identify patterns, triggers, and potential causes of insomnia.
To maintain a sleep diary, you will record various aspects of your sleep each day. These may include the time you go to bed, the time you attempt to fall asleep, how long it takes you to fall asleep, the number and duration of awakenings during the night, and the time you wake up in the morning. You can also track factors that may affect your sleep, such as caffeine or alcohol consumption, exercise, medication use, and levels of stress or anxiety.
In addition to sleep-related information, you can also include details about your daily routines, such as your bedtime rituals, activities before bed, and your subjective experience of sleep quality (e.g., how rested you feel upon waking). It is also helpful to note any specific events or circumstances that may have influenced your sleep, such as a stressful day at work or a change in environment.
By consistently maintaining a sleep diary, you create a comprehensive record of your sleep patterns and behaviors. This information can be shared with a healthcare professional, such as a sleep specialist or therapist, to assist in the evaluation and diagnosis of insomnia. The data collected in the sleep diary can provide valuable insights into your sleep habits, potential triggers for insomnia, and areas where improvements can be made to promote better sleep hygiene.
Remember, the accuracy and consistency of your sleep diary are essential for obtaining reliable results. Try to record information as soon as possible after waking, using specific details and being as objective as possible. This will help healthcare professionals gain a better understanding of your sleep patterns and tailor treatment plans that best suit your needs.
A sleep diary is a simple yet powerful tool that can shed light on the complexities of insomnia. By diligently tracking and analyzing your sleep patterns, you take an active role in managing your sleep health and working towards the goal of restful nights and rejuvenating days.
2. Medical Evaluation
During a medical evaluation for insomnia, your healthcare provider will conduct a thorough assessment to evaluate any potential underlying medical conditions that may be contributing to your sleep problems. This evaluation typically involves a comprehensive medical history, physical examination, and possibly some diagnostic tests. The goal is to identify and address any medical factors that may be causing or exacerbating your insomnia.
1. Medical History: Your healthcare provider will review your medical history to gather information about your overall health, sleep patterns, and any symptoms or concerns you may have. They will ask questions about your sleep habits, sleep environment, and daytime functioning. It is important to be open and honest and provide accurate details to help your provider gain a complete understanding of your condition.
2. Physical Examination: A physical examination may be conducted to assess your general health and identify any physical factors that could be contributing to your sleep disturbances. This may involve checking your vital signs, examining your body for signs of underlying conditions, and evaluating your neurological status.
3. Diagnostic Tests: In some cases, your healthcare provider may recommend specific diagnostic tests to further investigate underlying medical conditions. These tests can vary depending on your specific symptoms and medical history. Some common tests that may be conducted include blood tests to assess hormone levels or screen for specific medical conditions, imaging tests to evaluate the structure of your brain or airways, or a sleep study (polysomnography) to monitor your sleep patterns and physiological responses during the night.
Through a comprehensive medical evaluation, your healthcare provider can gain valuable insights into any medical factors that may be contributing to your insomnia. Identifying and addressing these underlying conditions is an essential step in developing an effective treatment plan to manage your sleep disorder.
HTML List:
- Medical History: Gather information about sleep patterns, symptoms, and concerns.
- Physical Examination: Assess general health and identify physical factors.
- Diagnostic Tests: Conduct tests to investigate underlying medical conditions.
3. Sleep Study
A sleep study, also known as polysomnography, is a specialized diagnostic tool used to evaluate and diagnose various sleep disorders, including insomnia. During a sleep study, a patient spends a night in a sleep laboratory, where their sleep patterns and physiological parameters are monitored and recorded.
The main purpose of a sleep study is to gather objective data about a person’s sleep, including brain activity, eye movements, muscle tone, heart rate, and oxygen levels. This information helps sleep specialists evaluate the quality and quantity of sleep, identify any disruptions or abnormalities, and make an accurate diagnosis.
The process of a sleep study involves the attachment of electrodes and sensors to the patient’s scalp, face, chest, and legs. These instruments measure brain waves, eye movements, muscle activity, heart rate, and breathing patterns throughout the night. Video and audio recordings may be used to capture any unusual behaviors or movements during sleep.
The data collected during the sleep study is then analyzed by sleep specialists who are trained to interpret sleep patterns and identify any abnormalities. They look for specific markers of insomnia, such as prolonged periods of wakefulness, frequent awakenings, or insufficient deep sleep. This analysis helps in determining the underlying causes of insomnia and formulating an appropriate treatment plan.
Sleep studies are typically conducted in a sleep laboratory, but advancements in technology have made it possible to perform certain types of sleep studies in the comfort of the patient’s own home. Portable devices can record essential sleep parameters and provide valuable information for diagnosis and treatment.
A sleep study plays a crucial role in diagnosing insomnia and other sleep disorders. By monitoring and analyzing the various aspects of sleep, a sleep study helps healthcare professionals understand the underlying causes of insomnia and develop personalized treatment plans. It is a valuable tool in ensuring accurate diagnosis and effective management of sleep disorders.
Additional resource:
Learn more about another sleep disorder: Sleep Paralysis: Causes, Symptoms, and Coping Strategies.
Treatment of Insomnia

When it comes to treating insomnia, several options are available to help restore healthy sleep patterns and improve overall sleep quality. These treatment approaches range from lifestyle modifications to therapeutic interventions and medications.
Sleep Hygiene: One of the first steps in treating insomnia is practicing good sleep hygiene. This involves establishing a regular sleep schedule, creating a calming bedtime routine, and optimizing the sleep environment by ensuring it is dark, quiet, and comfortable.
Cognitive Behavioral Therapy for Insomnia (CBTI): CBTI is a highly effective therapeutic approach that focuses on identifying and addressing the underlying thoughts, behaviors, and emotions that contribute to insomnia. It involves techniques such as sleep restriction, stimulus control, and relaxation training to promote better sleep.
Medications: In some cases, medication may be prescribed to treat insomnia. These may include short-term sleep aids or medications that target specific sleep-related issues, such as sleep onset or sleep maintenance difficulties. It’s important to use these medications under the guidance of a healthcare professional.
Alternative Therapies: Some individuals may find relief from insomnia through alternative therapies such as acupuncture, herbal supplements, or relaxation techniques like yoga or meditation. While the evidence for these approaches varies, they can be worth exploring for those seeking non-pharmacological options.
It’s important to remember that the most effective treatment approach for insomnia may vary from person to person. Consulting with a healthcare professional who specializes in sleep disorders can help determine the most appropriate treatment strategy for individual needs, considering factors such as the underlying cause of insomnia and any co-existing medical or mental health conditions.
1. Sleep Hygiene
Maintaining good sleep hygiene plays a crucial role in promoting healthy sleep patterns and combating insomnia. Sleep hygiene refers to a set of habits and practices that contribute to optimal sleep quality and duration. By following these practices, individuals can create an environment conducive to falling asleep quickly and staying asleep throughout the night. Here are some essential tips for improving sleep hygiene:
1. Establish a Consistent Sleep Schedule: Going to bed and waking up at the same time every day, even on weekends, helps regulate the body’s internal clock. This consistency reinforces the natural sleep-wake cycle and trains the body to become sleepy at the appropriate time.
2. Create a Relaxing Bedtime Routine: Develop a pre-sleep ritual that signals to your body that it’s time to unwind and prepare for sleep. This may include activities such as reading a book, taking a warm bath, practicing relaxation techniques like deep breathing or meditation, or listening to calming music.
3. Optimize Your Sleep Environment: Ensure that your bedroom is cool, dark, and quiet. Use blackout curtains, earplugs, or a white noise machine to minimize external disturbances. Invest in a comfortable mattress, pillows, and bedding that support a restful sleep experience.
4. Avoid Stimulants and Heavy Meals: Limit or avoid consuming caffeine, nicotine, and alcohol close to bedtime, as these substances can interfere with the ability to fall asleep and stay asleep. Additionally, avoid large, heavy meals before bedtime, as they can cause discomfort and disrupt sleep.
5. Limit Exposure to Electronics: The blue light emitted by electronic devices such as smartphones, tablets, and computers can interfere with the production of melatonin, a hormone that regulates sleep. Avoid using electronic devices at least an hour before bed, or use blue light filters or amber-tinted glasses to reduce the impact.
6. Engage in Regular Physical Activity: Regular exercise during the day can promote better sleep at night. However, avoid intense workouts close to bedtime as they may increase alertness and make it harder to fall asleep.
By implementing these sleep hygiene practices consistently, individuals can create an environment and routine that promote restful and rejuvenating sleep. However, if insomnia persists despite practicing good sleep hygiene, it may be necessary to explore other treatment options such as cognitive-behavioral therapy for insomnia (CBTI) or medications. It’s important to consult with a healthcare professional for a comprehensive evaluation and personalized treatment plan.
Internal Link: Sleepwalking: Causes, Risks, and Prevention Strategies
2. Cognitive Behavioral Therapy for Insomnia (CBTI)
Cognitive Behavioral Therapy for Insomnia (CBTI) is a widely recognized and effective treatment approach for managing and overcoming insomnia. Unlike medications that provide temporary relief, CBTI addresses the root causes and underlying factors contributing to insomnia, helping individuals develop long-term strategies for improved sleep.
CBTI focuses on changing negative thought patterns and behaviors that can interfere with sleep. It is typically conducted by a trained therapist or sleep specialist and involves several components:
1. Sleep Education: The therapist provides information about sleep and helps individuals better understand the factors that may be contributing to their insomnia. This includes educating them about healthy sleep habits, addressing misconceptions about sleep, and explaining the importance of a consistent sleep schedule.
2. Sleep Restriction: This technique involves reducing the amount of time an individual spends in bed to match the actual amount of sleep they are getting. By gradually increasing sleep time as sleep improves, it helps to consolidate sleep and strengthen the association between the bed and sleep.
3. Stimulus Control Therapy: This component focuses on creating a sleep-friendly bedroom environment and establishing a consistent bedtime routine. It helps individuals associate the bed with sleep and relaxation, rather than wakefulness and frustration. This may involve avoiding stimulating activities in bed, using the bed only for sleep and intimacy, and establishing a relaxing pre-sleep routine.
4. Cognitive Therapy: CBTI also addresses the negative thoughts and beliefs that can contribute to insomnia. Therapists work with individuals to identify and challenge these thoughts, replacing them with more positive and realistic ones. This helps reduce anxiety and stress surrounding sleep, improving the chances of falling asleep and staying asleep.
5. Relaxation Techniques: CBTI often includes teaching relaxation exercises, such as deep breathing, progressive muscle relaxation, and mindfulness meditation. These techniques can help calm the mind and body, promoting a state of relaxation that is conducive to sleep.
CBTI is typically a short-term treatment, with sessions conducted over several weeks. It empowers individuals to take an active role in managing their sleep and provides them with the tools and skills to overcome insomnia on their own. CBTI has been shown to be highly effective, even for individuals with chronic insomnia, and its benefits can be long-lasting.
Cognitive Behavioral Therapy for Insomnia (CBTI) is a comprehensive and effective approach for treating insomnia. By addressing the thoughts, behaviors, and environmental factors that contribute to sleep disturbances, CBTI helps individuals develop healthier sleep habits and regain control over their sleep. Whether used as a standalone treatment or in combination with other interventions, CBTI offers a promising solution for those seeking long-term relief from insomnia.
3. Medications
Medications can be a valuable tool in the treatment of insomnia, especially in cases where non-pharmacological approaches have proven ineffective. There are various types of medications that are commonly used to help improve sleep quality and reduce insomnia symptoms.
1. Sedative-Hypnotics: Sedative-hypnotic medications are commonly prescribed for insomnia and work by slowing down brain activity, promoting relaxation, and inducing sleep. These medications include benzodiazepines, such as diazepam and temazepam, as well as non-benzodiazepine medications, such as zolpidem and eszopiclone. They are typically used on a short-term basis due to the risk of tolerance and dependence with long-term use.
2. Antidepressants: Certain antidepressant medications can be prescribed as an off-label treatment for insomnia. These medications, such as trazodone and amitriptyline, can help improve sleep by targeting underlying depressive symptoms or by directly promoting sleep-inducing effects.
3. Melatonin: Melatonin is a hormone naturally produced by the body that helps regulate the sleep-wake cycle. Synthetic melatonin supplements are available over-the-counter and can be used to help regulate sleep patterns. They are particularly helpful for individuals who experience disruptions in their natural melatonin production, such as those with jet lag or shift work.
4. Antihistamines: Some over-the-counter antihistamine medications, such as diphenhydramine, can have sedating effects and are commonly used as sleep aids. However, they should be used with caution as they can cause daytime drowsiness and may lead to dependency if used regularly.
It is important to note that medication should be used under the guidance and supervision of a healthcare professional. They will consider various factors such as the individual’s medical history, potential drug interactions, and the severity of the insomnia before determining the appropriate medication and dosage. Additionally, medications should be used as part of a comprehensive treatment plan that may include lifestyle modifications and behavioral therapy to address the underlying causes of insomnia.
Note: Medications should always be used responsibly and as directed by a healthcare professional.
4. Alternative Therapies
Alternative therapies can be a valuable addition to the treatment plan for insomnia. These therapies aim to promote relaxation, reduce stress, and improve sleep quality through non-conventional methods. While they may not be supported by extensive scientific evidence, many individuals find them helpful in managing their sleep disturbances. Here are a few alternative therapies that you may consider exploring:
1. Aromatherapy: Aromatherapy involves using essential oils extracted from plants to promote relaxation. Lavender, chamomile, and valerian are commonly used oils believed to have calming effects on the mind and body. You can use these oils in a diffuser, add a few drops to your bath, or apply them topically to help create a peaceful environment that promotes better sleep.
2. Acupuncture: Acupuncture, a traditional Chinese practice, involves inserting thin needles into specific points on the body. It is believed to rebalance the flow of energy and promote relaxation. Some studies suggest that acupuncture may help improve sleep quality and reduce insomnia symptoms. If you’re considering acupuncture, seek a licensed practitioner with experience in treating sleep disorders.
3. Meditation: Meditation is a mindfulness practice that involves focusing attention and eliminating the stream of thoughts. Regular meditation practice can help calm the mind, reduce stress, and promote better sleep. You can try various meditation techniques such as guided meditation, mindfulness meditation, or loving-kindness meditation. Engaging in a meditation practice before bedtime can help prepare your mind and body for a restful sleep.
4. Herbal Supplements: Certain herbal supplements, such as chamomile, passionflower, and valerian root, have been used for centuries to promote relaxation and improve sleep. These supplements are available in different forms, including teas, capsules, or tinctures. It is important to consult with a healthcare professional before starting any herbal supplementation to ensure safety and avoid potential interactions with other medications.
5. Yoga: Yoga combines physical postures, breathing exercises, and meditation to promote relaxation and stress reduction. Practicing certain yoga poses, such as legs-up-the-wall pose or forward bends, can help calm the nervous system and prepare the body for sleep. Additionally, incorporating deep breathing techniques, such as alternate nostril breathing or box breathing, can help reduce anxiety and induce a state of relaxation conducive to sleep.
It’s essential to remember that alternative therapies should be used as complementary approaches and not as standalone treatments for insomnia. If you decide to explore alternative therapies, it is advisable to inform your healthcare provider and seek guidance to ensure their safety and appropriateness for your specific situation.
Prevention of Insomnia
Preventing insomnia is a proactive approach to maintaining healthy sleep habits and avoiding sleep disturbances. By implementing certain strategies and lifestyle changes, individuals can reduce the risk of developing insomnia and promote restful sleep. Here are some effective measures for preventing insomnia:
1. Maintain a Consistent Sleep Schedule: Set a regular sleep schedule by going to bed and waking up at the same time every day, even on weekends. This helps regulate the body’s internal clock and promotes better sleep quality.
2. Create a Sleep-Friendly Environment: Make your bedroom a tranquil and comfortable space conducive to sleep. Keep the room cool, dark, and quiet. Use earplugs, an eye mask, or white noise machines if necessary.
3. Establish a Bedtime Routine: Develop a relaxing routine before bedtime to signal your body that it’s time to sleep. Engage in calming activities like reading a book, taking a warm bath, or practicing relaxation techniques like deep breathing or meditation.
4. Avoid Stimulants: Limit the intake of caffeine, nicotine, and alcohol, especially close to bedtime. These substances can interfere with sleep quality and make it difficult to fall asleep or stay asleep.
5. Exercise Regularly: Engage in regular physical activity during the day, but avoid intense exercise close to bedtime. Regular exercise promotes better sleep, helps relieve stress, and improves overall sleep quality.
6. Manage Stress: Find healthy ways to manage stress, such as practicing mindfulness or engaging in stress-reducing activities like yoga or journaling. Stress can disrupt sleep and contribute to the onset of insomnia.
7. Avoid Screen Time Before Bed: Limit the use of electronic devices, such as smartphones, tablets, and computers, before bedtime. The blue light emitted by these devices can interfere with the production of melatonin, a hormone that regulates sleep-wake cycles.
8. Create a Restful Sleep Environment: Invest in a comfortable mattress, pillow, and bedding that suit your preferences. Make sure your sleep environment is free from distractions and promotes relaxation.
By implementing these preventive measures, individuals can significantly reduce the risk of developing insomnia and maintain healthy sleep patterns. However, if insomnia persists or becomes chronic despite these efforts, it is essential to consult a healthcare professional for further evaluation and treatment options. Remember, prevention is always better than cure when it comes to insomnia.
Tips for a Good Night’s Sleep
Getting a good night’s sleep is essential for overall health and well-being. If you’re struggling with insomnia, implementing healthy sleep habits can greatly improve your chances of achieving a restful sleep. Here are some tips to help you achieve a good night’s sleep:
1. Stick to a consistent sleep schedule: Try to go to bed and wake up at the same time every day, even on weekends. This helps regulate your body’s internal clock and promotes a more balanced sleep-wake cycle.
2. Create a relaxing bedtime routine: Establishing a soothing routine before bed can signal to your body that it’s time to unwind and prepare for sleep. Activities like reading a book, taking a warm bath, or practicing relaxation techniques can help calm your mind and promote a peaceful transition to sleep.
3. Create a sleep-friendly environment: Make sure your bedroom is conducive to sleep. Keep the room cool, dark, and quiet, and invest in a comfortable mattress and pillows. Consider using earplugs, eye masks, or white noise machines if needed.
4. Limit exposure to electronic devices: The blue light emitted by smartphones, tablets, and computers can interfere with your sleep. Try to avoid using electronic devices at least an hour before bed, or use blue light filters or night mode settings to minimize its impact.
5. Avoid stimulants: Limit your intake of caffeine, nicotine, and alcohol, especially in the hours leading up to bedtime. Stimulants can disrupt your sleep patterns and make it harder to fall asleep.
6. Get regular exercise: Engaging in regular physical activity can promote better sleep quality. However, it’s best to avoid exercising close to bedtime as it can have an energizing effect and make it harder to fall asleep.
7. Manage stress: Stress and anxiety can greatly impact your sleep. Find healthy coping mechanisms for managing stress, such as practicing relaxation techniques, journaling, or seeking support from a therapist.
8. Avoid daytime napping: If you’re having trouble sleeping at night, it’s best to avoid daytime napping as it can interfere with your sleep drive. If you must nap, keep it short and early in the day.
9. Avoid heavy meals and liquids before bed: Eating a heavy meal or consuming a lot of fluids close to bedtime can cause discomfort and disrupt your sleep. It’s best to have a light snack if needed and avoid excessive fluids before sleep.
10. Seek professional help if needed: If your insomnia persists despite implementing these tips, it’s important to consult a healthcare professional. They can provide further guidance, diagnose any underlying conditions, and recommend appropriate treatments.
By implementing these tips, you can create an environment and routine that promotes relaxation and better sleep. Remember that consistency is key, and it may take some time to establish new habits. Be patient with yourself and make sleep a priority. Sleep well and wake up refreshed!
Conclusion
In conclusion, insomnia is a complex sleep disorder that can significantly impact a person’s well-being and daily functioning. It is not simply a matter of difficulty falling asleep; it can manifest in various ways, including frequent awakenings throughout the night, early morning awakening, and non-restorative sleep. The causes of insomnia can be multifaceted, ranging from lifestyle factors and medical conditions to psychological factors. Identifying the underlying causes of insomnia is essential in order to address and manage the condition effectively.
Fortunately, there are various treatment options available for insomnia. Sleep hygiene practices, such as maintaining a consistent sleep schedule, creating a relaxing bedtime routine, and optimizing the sleep environment, can greatly improve sleep quality. Cognitive Behavioral Therapy for Insomnia (CBTI) is also a highly effective treatment approach that helps individuals develop healthier sleep habits and manage the psychological factors contributing to insomnia.
In some cases, medication may be prescribed to help regulate sleep, but it should be used cautiously and under the guidance of a healthcare professional. Alternative therapies, such as relaxation techniques, acupuncture, or herbal remedies, may also be explored as additional options for managing insomnia.
Prevention is also key in maintaining healthy sleep patterns. By adopting and maintaining good sleep habits and managing stress levels, individuals can significantly reduce the likelihood of developing insomnia.
Remember, if you are struggling with persistent sleep difficulties, it is important to seek medical advice and undergo a thorough evaluation to determine the underlying causes of your insomnia and develop an appropriate treatment plan. Don’t let insomnia control your life; take action and reclaim your nights of restful sleep.
Internal Link: Sleep Paralysis: Causes, Symptoms, and Coping Strategies
Frequently Asked Questions
1. What are the different types of insomnia?
Insomnia can be classified into three types: transient insomnia, which lasts for a few days or weeks; acute insomnia, which persists for several weeks or months; and chronic insomnia, which lasts for more than three months.
2. Does anxiety contribute to insomnia?
Yes, anxiety can contribute to the development and maintenance of insomnia. Individuals who experience high levels of anxiety often have racing thoughts and heightened arousal, making it difficult for them to relax and fall asleep.
3. Can medications cause insomnia?
Yes, certain medications can disrupt sleep patterns and contribute to insomnia. Stimulant medications, antidepressants, and some asthma medications are known to interfere with sleep and can lead to insomnia.
4. How does lifestyle impact insomnia?
Lifestyle factors play a significant role in insomnia. Poor sleep hygiene, irregular sleep schedules, excessive caffeine or alcohol intake, and lack of physical activity can all contribute to the development of insomnia.
5. Can insomnia be a symptom of an underlying medical condition?
Yes, insomnia can be a symptom of various medical conditions, including chronic pain, heartburn, respiratory disorders, hormonal imbalances, and neurological conditions.
6. Is it normal to experience occasional episodes of insomnia?
Yes, it is normal to experience occasional episodes of insomnia, especially during times of stress or significant life events. However, if insomnia becomes persistent and starts affecting daily functioning, it is important to seek help and address the underlying causes.
7. How can cognitive behavioral therapy help with insomnia?
Cognitive Behavioral Therapy for Insomnia (CBTI) is a highly effective treatment approach that helps individuals change thoughts, behaviors, and habits that contribute to insomnia. It focuses on improving sleep hygiene, reducing anxiety, and establishing a regular sleep schedule.
8. Are there any alternative therapies for insomnia?
Yes, there are alternative therapies that can be used alongside conventional treatments for insomnia. These may include relaxation techniques, meditation, acupuncture, and herbal remedies like valerian root or chamomile.
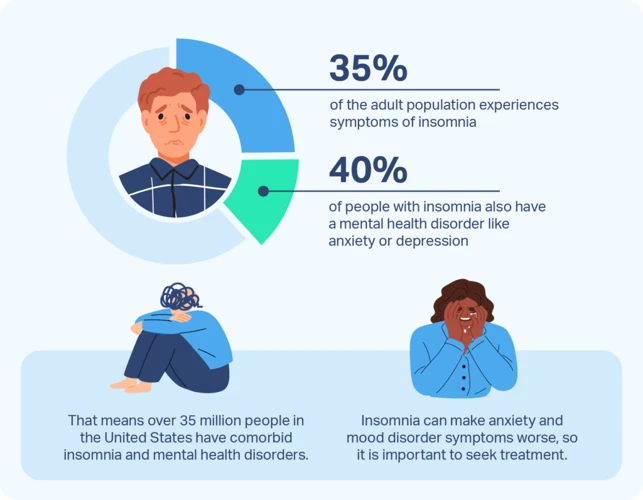
9. Can insomnia affect mental health?
Yes, insomnia is strongly associated with mental health conditions such as depression and anxiety. Lack of sleep can exacerbate symptoms of these conditions and make it more difficult for individuals to cope with daily challenges.
10. How can I improve my sleep hygiene?
To improve sleep hygiene, establish a consistent sleep schedule, create a calming bedtime routine, limit exposure to electronic devices before bed, create a comfortable sleep environment, and avoid consuming stimulating substances like caffeine or nicotine close to bedtime.