Understanding the Causes of Sleepwalking: Unveiling the Mysterious Nocturnal Wanderings
Have you ever woken up in the middle of the night to find yourself walking aimlessly around your house, completely unaware of what you’re doing? Sleepwalking, also known as somnambulism, is a perplexing phenomenon that has fascinated and puzzled scientists for centuries. In this comprehensive guide, we delve into the mysterious world of sleepwalking, exploring its causes and shedding light on why some individuals may embark on nocturnal adventures while others peacefully slumber. So, grab a cup of tea, settle into a cozy corner, and join us on this fascinating journey of unraveling the enigma behind sleepwalking.
Overview of Sleepwalking

Sleepwalking, or somnambulism, is a fascinating sleep disorder that involves performing complex behaviors while in a deep state of sleep. This condition typically occurs during the first few hours of sleep, as the individual transitions from deep sleep to lighter stages of sleep. Sleepwalkers may engage in a variety of activities, ranging from simple actions like talking or sitting up in bed to more complex behaviors such as walking, cooking, or even driving a car.
Sleepwalking episodes can last anywhere from a few seconds to 30 minutes or longer, and often occur with minimal or no memory of the event upon waking. It is estimated that approximately 1-15% of the general population experiences sleepwalking at some point in their lives.
While the exact cause of sleepwalking remains mysterious, researchers have identified several factors that can contribute to its occurrence. Explore the sections below to gain a deeper understanding of the potential triggers, medical conditions, developmental factors, genetic predisposition, environmental influences, and other contributing factors that might play a role in the manifestation of sleepwalking episodes.
Common Triggers
Common triggers can play a significant role in the occurrence of sleepwalking episodes. These triggers vary from person to person, but often include:
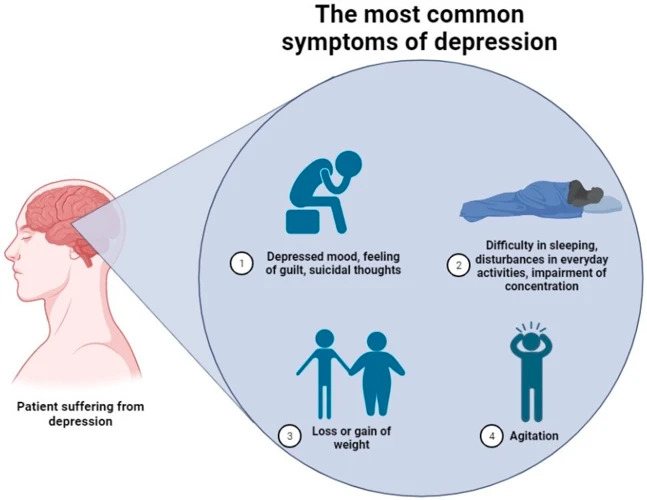
- Stress and Anxiety: High levels of stress and anxiety can disrupt the normal sleep patterns, potentially leading to sleepwalking. Stress management techniques and finding ways to relax before bed may help reduce the frequency of sleepwalking episodes.
- Sleep Deprivation: Lack of quality sleep or not getting enough sleep can increase the risk of sleepwalking. It is important to establish a regular sleep schedule and prioritize sufficient sleep each night to minimize the likelihood of sleepwalking incidents.
- Medication and Substance Use: Certain medications, such as sedatives or sleep aids, can trigger sleepwalking in some individuals. Additionally, alcohol and drug use can disrupt sleep patterns and increase the likelihood of sleepwalking episodes. It is essential to speak with a healthcare professional about the potential side effects of medications and substances.
To learn more about different types of sleepwalking, check out our detailed guide on types of sleepwalking. There is a relationship between sleepwalking and other sleep disorders which you can read about in our article Sleepwalking and its Relationship with Sleep Disorders. Parents of children who sleepwalk may find our article on sleepwalking in children informative and helpful to better understand this phenomenon.
Stress and Anxiety
Stress and anxiety are well-known triggers for sleepwalking episodes. When individuals experience heightened levels of stress or anxiety, it can disrupt their regular sleep patterns and increase the likelihood of sleepwalking. The exact mechanisms behind this connection are not fully understood, but it is believed that the body’s stress response can interfere with normal sleep processes, leading to sleep disturbances and potential sleepwalking episodes.
In times of stress, the brain may struggle to transition smoothly between sleep stages, causing individuals to enter a state of mixed arousal where the body is partially awake but still engaged in sleep-like behaviors. This can result in sleepwalking episodes characterized by individuals carrying out complex actions while remaining in a dream-like state.
Additionally, stress and anxiety can lead to poor sleep quality, which can further contribute to sleepwalking. When individuals are unable to achieve restful sleep due to stress or anxiety, they may experience increased sleep fragmentation and disruptions in the normal sleep cycle. These disruptions can disrupt the delicate balance of sleep stages and increase the likelihood of sleepwalking.
If you’re experiencing high levels of stress or anxiety and notice an increase in sleepwalking episodes, it’s important to address and manage your stress levels. Engaging in relaxation techniques, practicing good sleep hygiene, and seeking support from a healthcare professional or therapist can all be beneficial in reducing stress and promoting better sleep, ultimately reducing the occurrence of sleepwalking episodes. Remember, taking care of your mental well-being plays a significant role in maintaining healthy sleep patterns and minimizing the risks associated with sleepwalking.
Sleep Deprivation
Sleep deprivation is a commonly recognized trigger for sleepwalking. When individuals do not get enough sleep, it can disrupt their regular sleep patterns and increase the likelihood of experiencing sleepwalking episodes. Chronic sleep deprivation, which can result from factors such as work demands, lifestyle choices, or medical conditions, can have a significant impact on the quality and duration of sleep.
Here are some key points to understand about the relationship between sleep deprivation and sleepwalking:
- Imbalance in sleep stages: Sleep deprivation can disrupt the normal progression of sleep stages, particularly the transition from deep sleep to lighter stages. This disruption can increase the chances of sleepwalking.
- Changes in brain activity: Lack of sleep can affect the brain’s functioning and lead to abnormal behaviors during sleep, including sleepwalking.
- Stress amplification: Sleep deprivation often goes hand in hand with increased stress levels. Stress is another known trigger for sleepwalking, and when combined with sleep deprivation, it can further contribute to the occurrence of sleepwalking episodes.
- Altered sleep-wake cycle: Sleep deprivation can disrupt the body’s natural sleep-wake cycle, making it more difficult for individuals to achieve restful sleep. This disruption can disrupt the brain’s ability to regulate sleep and wakefulness, potentially leading to sleepwalking.
If you’d like to learn more about different types of sleepwalking, click here.
Medication and Substance Use
Medication and substance use can play a significant role in triggering sleepwalking episodes. Certain medications, such as sedatives, hypnotics, and some antidepressants, can disrupt the normal sleep cycle and increase the likelihood of sleepwalking. These medications may interfere with the brain’s ability to transition smoothly between sleep stages, leading to increased arousal and the potential for sleepwalking.
Additionally, the use of substances like alcohol, illicit drugs, and even certain prescription medications can also contribute to sleepwalking. Alcohol, in particular, is known to disrupt the quality and duration of sleep, often causing fragmented and restless sleep patterns. This can increase the likelihood of sleepwalking episodes, especially in individuals who are already prone to this behavior.
It’s important to note that certain individuals may be more susceptible to the effects of medication and substances, and their impact on sleepwalking can vary from person to person. If you’re experiencing sleepwalking episodes and are taking medication or using substances, it’s crucial to consult with a healthcare professional to evaluate any potential connections.
Medical Conditions
Medical conditions can significantly influence the occurrence and frequency of sleepwalking episodes. Individuals who experience sleep disorders such as nightmares or sleep terrors may be more prone to sleepwalking. Nightmares can create a sense of fear and anxiety, leading to disrupted sleep patterns and potentially triggering sleepwalking episodes. Additionally, restless leg syndrome, a condition characterized by uncomfortable sensations and the urge to move the legs, has been linked to sleepwalking. The discomfort caused by restless leg syndrome can disrupt the sleep cycle and contribute to sleepwalking episodes. Obstructive sleep apnea, a condition where the airway becomes partially or completely blocked during sleep, has been associated with an increased risk of sleepwalking. The interruptions in breathing can disrupt the sleep cycle and lead to sleepwalking behaviors. By understanding these medical conditions, individuals and healthcare professionals can take appropriate measures to manage and reduce the occurrence of sleepwalking episodes.
Nightmares and Sleep Disorders
Nightmares and certain sleep disorders can contribute to the occurrence of sleepwalking episodes. Nightmares, which are vivid and disturbing dreams that often evoke fear or anxiety, can disrupt the normal sleep cycle and lead to sleepwalking. The emotional intensity experienced during a nightmare can trigger a sleepwalker to act out the contents of the dream, resulting in sleepwalking episodes.
Additionally, individuals with other sleep disorders such as sleep apnea, restless leg syndrome, or REM sleep behavior disorder (RBD) may be more prone to sleepwalking. Sleep apnea, characterized by interrupted breathing during sleep, can cause sleep disturbances that may contribute to sleepwalking. Restless leg syndrome, which is characterized by uncomfortable sensations in the legs that worsen at night, can disrupt sleep and increase the likelihood of sleepwalking episodes.
REM sleep behavior disorder (RBD), a condition in which individuals physically act out their dreams during REM sleep, can also increase the risk of sleepwalking. In RBD, the normal paralysis that occurs during REM sleep, which prevents movement, is incomplete or absent, allowing individuals to physically act out their dream scenarios, potentially leading to sleepwalking episodes.
Restless Leg Syndrome
Restless Leg Syndrome (RLS) is a neurological disorder that can contribute to sleepwalking episodes. People with RLS experience uncomfortable sensations in their legs, often described as crawling, tingling, itching, or aching. These sensations typically worsen at rest, such as when lying down or sitting for extended periods.
RLS can disrupt sleep and cause the affected individual to have an irresistible urge to move their legs to alleviate the discomfort. This urge to move can initiate sleepwalking episodes, as the person seeks relief by getting out of bed and engaging in movement. Although the exact cause of RLS is still unknown, it is believed to involve a malfunction in the brain’s dopamine system.
Treating RLS can help reduce the occurrence of sleepwalking. Lifestyle changes such as regular exercise, avoiding caffeine and alcohol, and practicing good sleep hygiene may provide relief. Medications that increase dopamine levels or provide symptomatic relief may also be prescribed to manage RLS symptoms and alleviate sleepwalking episodes. If you suspect that RLS may be contributing to your sleepwalking, it is essential to consult with a healthcare professional for accurate diagnosis and appropriate treatment.
Obstructive Sleep Apnea
Obstructive Sleep Apnea (OSA) is a medical condition that can contribute to the occurrence of sleepwalking. OSA is characterized by repetitive pauses in breathing during sleep, typically caused by the collapse of the airway. These pauses in breathing can lead to decreased oxygen levels in the blood and fragmented sleep, which can disrupt the normal sleep cycle.
There is evidence to suggest that individuals with OSA may be more prone to sleepwalking episodes. The fragmented sleep and periods of low oxygen levels that occur in OSA can disrupt the normal sleep architecture and increase the likelihood of sleepwalking. Additionally, the sleep disruption caused by OSA can lead to increased sleep inertia, which is the transitional period between sleep and wakefulness where sleepwalkers are more likely to engage in automatic behaviors.
Treating OSA can help reduce the occurrence of sleepwalking episodes. Continuous positive airway pressure (CPAP) therapy is a common treatment for OSA, which involves wearing a mask over the nose or mouth during sleep to deliver a steady stream of air to keep the airway open. By effectively treating the underlying OSA, the sleep architecture can be improved, reducing the risk of sleepwalking.
Developmental Factors
Developmental factors can also play a significant role in sleepwalking episodes. Children and adolescents are particularly prone to sleepwalking, with studies estimating that around 15% of children experience at least one episode. Sleepwalking in this age group is often seen as a normal part of development and generally resolves on its own as they grow older. The exact reasons behind the higher incidence of sleepwalking in children and adolescents are not fully understood, but experts suggest that it may be related to factors such as immaturity of the central nervous system, slower development of sleep patterns, and increased amounts of deep sleep. Additionally, hormonal changes during puberty may also contribute to the prevalence of sleepwalking in this age group. For parents seeking guidance and support in addressing their child’s sleepwalking, understanding the intricacies of this developmental factor is crucial.
Children and Adolescents
Sleepwalking is most commonly observed in children and adolescents, with studies suggesting that around 15% of children experience at least one episode of sleepwalking during their childhood. There are several reasons why sleepwalking is more prevalent in this age group.
- Immature Nervous System: The nervous systems of children and adolescents are still developing, and this immaturity can contribute to sleep disturbances and the occurrence of sleepwalking episodes.
- Overstimulation: Children are often exposed to high levels of stimulation throughout the day, including electronic devices, excessive screen time, and stimulating activities. This overstimulation can disrupt their sleep patterns and increase the likelihood of sleepwalking.
- Sleep Environment: Children may be more susceptible to sleepwalking if they have an uncomfortable sleep environment, such as sleeping in a new place or sharing a bed with a sibling.
- Increased Sleep Needs: Children and adolescents require more sleep than adults, and disruptions in their sleep patterns can lead to sleepwalking episodes.
- Genetic Factors: There is evidence to suggest that sleepwalking may have a genetic component, meaning that children with a family history of sleepwalking are more likely to experience it themselves.
If you’re a parent concerned about your child’s sleepwalking episodes, it’s important to create a safe sleep environment, establish a consistent bedtime routine, and ensure that your child is getting enough quality sleep. If the sleepwalking becomes frequent or causes distress, it is advisable to consult a healthcare professional who can provide further guidance.
For more information about sleepwalking in children, check out our article on Sleepwalking in Children: What Parents Need to Know.
Pregnancy
- Changes in Hormone Levels: During pregnancy, there is a significant increase in hormone levels, including progesterone. These hormonal changes can lead to disruptions in the sleep-wake cycle, potentially increasing the likelihood of sleepwalking episodes.
- Increased Fatigue and Disrupted Sleep: Pregnant women often experience increased fatigue and disruptions in their sleep patterns, particularly during the later stages of pregnancy. These sleep disturbances can contribute to sleepwalking, as the body struggles to maintain a proper balance between deep sleep and lighter stages of sleep.
- Stress and Anxiety: Pregnancy can bring about various emotional and psychological stressors, such as worries about the health of the baby, labor, and motherhood. This increased stress and anxiety may contribute to sleepwalking episodes as the mind and body attempt to process and cope with these feelings.
- Restless Leg Syndrome: Pregnant women are also more prone to experiencing restless leg syndrome, a condition characterized by uncomfortable sensations and the urge to move the legs. Restless leg syndrome can disrupt sleep and increase the likelihood of sleepwalking.
- Physical Discomfort: As the pregnancy progresses, physical discomfort, such as back pain, leg cramps, and frequent urination, can interfere with sleep quality. These discomforts may disrupt the sleep-wake cycle and contribute to sleepwalking episodes.
Genetic Predisposition
Genetic predisposition has long been recognized as a potential factor in the occurrence of sleepwalking. It is believed that certain individuals may have a genetic susceptibility to sleepwalking based on their family history or inherited traits. Studies have shown that if one or both parents have a history of sleepwalking, their children are more likely to experience sleepwalking episodes as well, suggesting a hereditary component.
Researchers have identified several genes that may be associated with sleepwalking. The DEC2 gene, for example, has been linked to shorter sleep duration and an increased likelihood of sleepwalking. Additionally, variations in the HLA gene, which plays a role in the immune system, have also been found to be more prevalent in individuals with a history of sleepwalking.
However, it is important to note that genetic predisposition alone does not guarantee the occurrence of sleepwalking. Other contributing factors, such as environmental influences, stress levels, or the presence of certain medical conditions, may interact with genetic factors to trigger sleepwalking episodes. Further research is needed to fully understand the complex interplay between genetics and other factors in the development of sleepwalking.
Environmental Influences
Environmental factors can play a significant role in triggering sleepwalking episodes. Certain situations or changes in the sleep environment can disrupt the normal sleep cycle and increase the likelihood of sleepwalking episodes. Here are some key environmental influences:
- Alcohol Consumption: Excessive alcohol consumption can disrupt sleep patterns and increase the likelihood of sleepwalking. Alcohol acts as a sedative, affecting the quality of sleep and potentially leading to sleepwalking episodes.
- Feeling Unsafe or Sleeping in a New Environment: Sleeping in an unfamiliar or unfamiliar environment can make individuals more prone to sleepwalking. Feelings of anxiety or unease can disrupt the sleep cycle and trigger sleepwalking episodes.
It is important to create a safe and comfortable sleep environment to minimize the risk of sleepwalking. This can include ensuring that the sleeping area is free of obstacles or hazards, using nightlights to provide a sense of security, and implementing relaxation techniques to reduce stress and promote better sleep quality.
Other Contributing Factors
There are several other contributing factors that can increase the likelihood of sleepwalking episodes. One such factor is alcohol consumption. Alcohol has a sedative effect on the body, which can disrupt the normal sleep cycle and increase the chances of sleepwalking. Additionally, feeling unsafe or sleeping in a new environment can trigger sleepwalking episodes. The unfamiliar surroundings can cause heightened anxiety and stress, leading to sleepwalking as a result. It is important to create a safe and comfortable sleep environment to minimize the occurrence of sleepwalking episodes.
Alcohol Consumption
Alcohol consumption has long been known to have an impact on sleep patterns and can potentially trigger episodes of sleepwalking. When consumed in large quantities or close to bedtime, alcohol can disrupt the normal sleep cycle and affect the quality of sleep. Alcohol acts as a sedative, initially causing drowsiness and promoting falling asleep faster. However, as the body metabolizes the alcohol, it can interfere with the different stages of sleep, including REM (rapid eye movement) sleep, which is crucial for restorative rest.
During the disruption of REM sleep, sleepwalking incidents may be more likely to occur, as the brain struggles to maintain a stable sleep-wake cycle. Additionally, alcohol can cause fragmented sleep, leading to increased arousal during sleep, which can trigger abnormal behaviors like sleepwalking.
Moreover, alcohol also relaxes inhibitions and impairs judgment, which can lead individuals to engage in risky behaviors, such as leaving their bed and navigating their surroundings while still asleep. It’s important to note that the effects of alcohol on sleep and sleepwalking can vary from person to person, and some individuals may be more susceptible to sleepwalking after consuming alcohol than others.
To mitigate the risk of sleepwalking incidents, it is advisable to avoid excessive alcohol consumption, particularly close to bedtime. Creating a healthy sleep routine, practicing good sleep hygiene, and limiting alcohol intake can help promote a more restful sleep and reduce the likelihood of experiencing sleepwalking episodes.
Feeling Unsafe or Sleeping in a New Environment
One of the contributing factors to sleepwalking episodes is the feeling of being unsafe or sleeping in a new environment. When someone is in an unfamiliar or unsettling environment, their brain may not fully relax during sleep, leading to an increased likelihood of sleepwalking. This phenomenon is known as “first-night effect.”
Research suggests that the brain’s hemispheres are more active during the initial night of sleep in a new location, as a survival mechanism to remain alert to potential dangers. This heightened brain activity can disrupt the normal sleep cycle and increase the chances of sleepwalking.
In addition to feeling unsafe or sleeping in a new environment, other environmental factors such as extreme temperatures, noise disturbances, or uncomfortable bedding can also contribute to sleepwalking episodes. These factors can disrupt the quality and depth of sleep, making a person more susceptible to sleepwalking behaviors.
It’s important to note that individuals who frequently experience sleepwalking may benefit from creating a sleep-friendly environment. This includes ensuring the bedroom is comfortable, quiet, and free from potential hazards that may trigger a sleepwalking episode.
Conclusion
In conclusion, understanding the causes of sleepwalking is crucial for both individuals experiencing this sleep disorder and the medical community. While the exact reasons behind sleepwalking are still not fully understood, research has suggested that stress and anxiety, sleep deprivation, medication and substance use, as well as certain medical conditions and developmental factors, can contribute to the occurrence of sleepwalking episodes.
Furthermore, genetic predisposition and environmental influences, such as alcohol consumption or feeling unsafe in a new environment, may also play a role in triggering sleepwalking episodes. By identifying these potential causes, individuals can take steps to minimize their risk of sleepwalking and seek appropriate treatment if necessary.
It’s important to note that sleepwalking on its own is usually not a cause for serious concern. However, if sleepwalking episodes become frequent, disruptive, or pose a risk to the individual’s safety, it is advisable to consult with a healthcare professional or sleep specialist for further evaluation and guidance.
By continuing to explore the underlying factors contributing to sleepwalking and promoting public awareness about this intriguing sleep disorder, we can enhance our understanding and potentially improve the quality of sleep for those affected. So, let’s keep investigating and unlocking the mysterious world of sleepwalking together.
Frequently Asked Questions
1. What is the typical age range for sleepwalking episodes?
Sleepwalking can occur at any age, but it is most common in children between the ages of 4 and 8. However, it can also affect adolescents and adults.
2. Can sleepwalking be dangerous?
In some cases, sleepwalking can lead to injuries if the individual engages in potentially dangerous activities while asleep. It is important to take precautions such as removing obstacles from the bedroom and ensuring a safe sleeping environment for sleepwalkers.
3. Is sleepwalking a sign of a serious sleep disorder?
Sleepwalking itself is considered a sleep disorder, but it can also be associated with other sleep disorders such as sleep apnea or restless leg syndrome. If you suspect you have a sleep disorder, it is recommended to consult a healthcare professional for an accurate diagnosis.
4. Can stress trigger sleepwalking episodes?
Yes, stress and anxiety can be common triggers for sleepwalking. High levels of stress can disrupt the quality of sleep and increase the likelihood of sleepwalking episodes.
5. Are there any known genetic factors associated with sleepwalking?
Yes, research suggests that there may be a genetic predisposition to sleepwalking. If a family member has a history of sleepwalking, there is a higher likelihood of experiencing sleepwalking episodes.
6. Can medication or substance use contribute to sleepwalking?
Yes, certain medications and substances such as sedatives, hypnotics, and alcohol can increase the likelihood of sleepwalking. It is important to be aware of the potential side effects of these substances on sleep patterns.
7. Can sleepwalking be triggered by nightmares?
Yes, sleepwalking can sometimes be triggered by nightmares or other sleep disturbances. Disturbed sleep can disrupt the sleep cycle and increase the chances of sleepwalking episodes.
8. Do sleepwalkers remember their sleepwalking episodes?
Most sleepwalkers have little to no memory of their sleepwalking episodes. This is because sleepwalking occurs during non-REM sleep, when the brain is not fully aware of its surroundings.
9. Can sleepwalking be treated?
In some cases, sleepwalking can be managed through certain lifestyle changes and creating a consistent sleep routine. However, for individuals with severe or frequent sleepwalking episodes, a healthcare professional may recommend other treatment options, such as medication or therapy.
10. Can sleepwalking be prevented?
While it may not be possible to completely prevent sleepwalking, there are steps that can be taken to reduce the occurrence of episodes. These include ensuring a calm and stress-free sleep environment, practicing good sleep hygiene, and avoiding triggers like sleep deprivation or excessive alcohol consumption.