Do you ever find yourself tossing and turning at night, unable to fall asleep? Or perhaps you wake up suddenly in the middle of the night, drenched in sweat and gasping for air? These are just a couple of examples of the many sleep disorders that affect millions of people around the world. Sleep disorders can disrupt our daily lives, leaving us feeling exhausted, irritable, and unable to function at our best. In this comprehensive guide, we will explore the top 10 sleep disorders, examining their symptoms, causes, and treatment options. So, whether you’re struggling with insomnia, narcolepsy, or restless legs syndrome, we’ve got you covered. Get ready to dive into the world of sleep disorders and discover the solutions that can help you get the restful sleep you deserve.
Insomnia
Insomnia is one of the most common sleep disorders, affecting millions of people worldwide. Insomnia is characterized by difficulty falling asleep, staying asleep, or both, leading to inadequate sleep and daytime drowsiness. The symptoms of insomnia can include difficulty initiating sleep, waking up frequently during the night, waking up too early in the morning, and feeling unrefreshed upon waking. There are several potential causes of insomnia, such as stress, anxiety, depression, medications, and underlying medical conditions. Treatment for insomnia often involves implementing good sleep hygiene practices, such as establishing a consistent sleep schedule, creating a comfortable sleep environment, and avoiding stimulating activities before bedtime. Additionally, certain medications or therapies, like cognitive-behavioral therapy for insomnia (CBT-I), may be recommended to manage insomnia symptoms. If you want to learn more about managing nightmares, you can check out our article on managing nightmares in children.
Symptoms of Insomnia
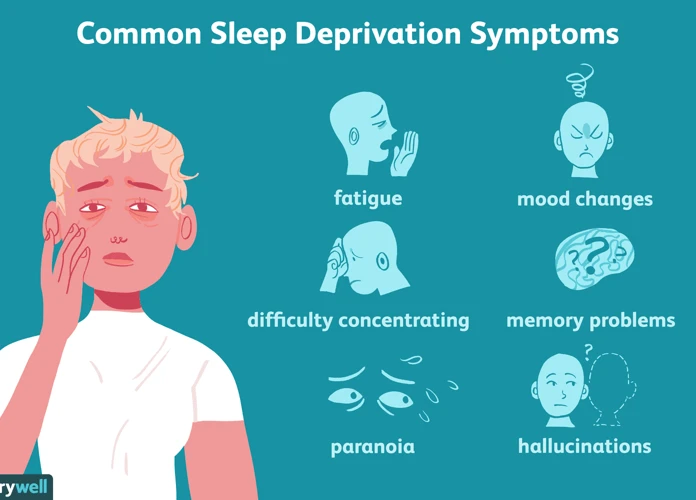
Insomnia can manifest in a variety of ways, making it important to recognize the symptoms of insomnia in order to seek appropriate treatment. One of the primary symptoms is difficulty falling asleep at night, also known as sleep-onset insomnia. Individuals with insomnia may find themselves lying awake in bed for extended periods, unable to drift off into a state of restful sleep. Another symptom is known as sleep maintenance insomnia, which involves waking up frequently during the night and struggling to fall back asleep. This can result in a fragmented and non-restorative sleep pattern. Some individuals with insomnia experience early morning awakening, where they wake up much earlier than desired and find it difficult to fall back asleep. This can lead to feeling tired and groggy throughout the day. Additionally, individuals with insomnia often report feeling unrefreshed upon waking, even after a seemingly adequate amount of sleep. This can result in persistent fatigue, difficulty concentrating, and reduced overall functioning during the daytime. If you want to explore more about sleep disorders and their impact on mental health, you can read our informative guide on the impact of sleep disorders on mental health.
Causes of Insomnia
Insomnia can have various causes, ranging from external factors to internal imbalances within the body. Here are some common factors that contribute to the development of insomnia:
1. Stress and Anxiety: Psychological stress, such as work or relationship problems, can keep the mind active and prevent relaxation necessary for sleep. Anxiety disorders can also lead to racing thoughts and restlessness at night.
2. Depression: Depression is often accompanied by insomnia. The sleep-wake cycle can be disrupted due to changes in brain chemistry and mood.
3. Medical Conditions: Certain medical conditions, such as chronic pain, arthritis, asthma, heartburn, and hormonal imbalances, can cause discomfort that interferes with sleep.
4. Medications: Some medications, such as antidepressants, pain medications, and stimulants, can disrupt sleep patterns as a side effect.
5. Substance Abuse: The use of substances like caffeine, nicotine, and alcohol close to bedtime can interfere with sleep quality and duration.
6. Irregular Sleep Schedule: Inconsistent sleep patterns, such as frequent changes in work shifts or jet lag, can disrupt the body’s internal clock and make it difficult to establish a regular sleep routine.
7. Poor Sleep Environment: Factors such as noise, excessive light, uncomfortable bedding, or an improper sleep environment can make it hard to fall asleep or stay asleep.
8. Underlying Sleep Disorders: Other sleep disorders, such as sleep apnea or restless legs syndrome, can contribute to insomnia.
Understanding the potential causes of insomnia is crucial in determining the appropriate treatment approach. If you’re interested in learning more about sleep-related topics, you can explore our article on understanding sleep paralysis.
Treatment for Insomnia
When it comes to treating insomnia, a multi-faceted approach is often necessary to address the underlying causes and promote better sleep. Here are some common treatment options for insomnia:
1. Sleep Hygiene: Implementing good sleep hygiene practices can have a significant impact on improving sleep quality. This includes establishing a regular sleep schedule, creating a comfortable sleep environment, avoiding stimulating activities before bedtime, and limiting daytime napping.
2. Cognitive-Behavioral Therapy for Insomnia (CBT-I): CBT-I is a highly effective treatment for insomnia that focuses on identifying and changing negative thoughts and behaviors around sleep. It may involve techniques such as relaxation training, stimulus control, sleep restriction, and cognitive restructuring.
3. Medications: In some cases, doctors may prescribe medications to manage insomnia symptoms. These can include over-the-counter sleep aids or prescription medications that help regulate sleep patterns. It’s important to consult with a healthcare professional before starting any medication regimen.
4. Addressing Underlying Medical Conditions: Insomnia can sometimes be a symptom of an underlying medical condition such as chronic pain, depression, or sleep apnea. Treating the underlying condition may help alleviate insomnia symptoms.
5. Alternative Therapies: Some individuals find relief from insomnia through alternative therapies such as acupuncture, massage, or herbal supplements. While the effectiveness of these approaches may vary, they can be worth exploring under the guidance of a qualified practitioner.
6. Lifestyle Changes: Making certain lifestyle changes can also contribute to better sleep. Regular exercise, avoiding caffeine and alcohol close to bedtime, and managing stress levels are all factors that can positively impact sleep quality.
It’s important to remember that what works for one individual may not work for another when it comes to treating insomnia. It may take a combination of approaches and some trial and error to find the most effective treatment plan. Consulting with a healthcare professional or sleep specialist can provide further guidance and support in managing insomnia symptoms.
Narcolepsy
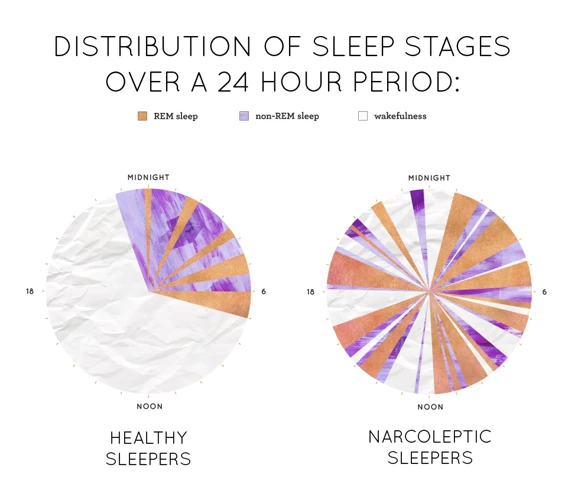
Narcolepsy is a neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. Individuals with narcolepsy experience excessive daytime sleepiness and have difficulty staying awake during the day. The symptoms of narcolepsy include sudden and uncontrollable sleep attacks, cataplexy (sudden loss of muscle tone), sleep paralysis, and vivid hallucinations during sleep onset or upon awakening. The exact cause of narcolepsy is not fully understood, but it is believed to involve a combination of genetic and environmental factors. It is thought that narcolepsy may be linked to a lack of a brain chemical called hypocretin, which helps regulate wakefulness and sleep. Treatment for narcolepsy focuses on managing symptoms and improving quality of life. This may involve the use of medications, lifestyle changes (such as practicing good sleep hygiene and scheduled napping), and supportive therapies. For individuals with narcolepsy, understanding and managing the condition is crucial to maintaining a balanced and fulfilling life.
Symptoms of Narcolepsy
Narcolepsy is a neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. People with narcolepsy experience excessive daytime sleepiness, regardless of the amount of sleep they get at night. The symptoms of narcolepsy can vary from person to person but often include: sudden and uncontrollable episodes of sleepiness or the urge to sleep (known as sleep attacks), temporary muscle weakness or loss of muscle control (cataplexy), hallucinations or vivid dreams that occur while falling asleep or waking up (hypnagogic or hypnopompic hallucinations), and sleep paralysis, a temporary inability to speak or move when waking up or falling asleep. These symptoms can have a significant impact on a person’s daily life, making it difficult to concentrate, stay awake during the day, or participate in normal activities. If you find the topic of sleep paralysis interesting, you can read our article on understanding sleep paralysis.
Causes of Narcolepsy
The exact causes of narcolepsy are still not fully understood, but research suggests that it is a combination of genetic predisposition and environmental factors. One of the primary factors is the deficiency of a brain chemical called hypocretin, which regulates sleep-wake cycles. In individuals with narcolepsy, there is a significant decrease in the production of hypocretin, leading to disrupted sleep patterns. Additionally, certain genetic mutations have been identified that increase the risk of developing narcolepsy. Other potential factors include abnormal immune system responses, hormonal changes, and brain injuries. It is important to note that narcolepsy is not caused by laziness, a lack of sleep, or a psychological issue. While the exact causes may vary from person to person, understanding the underlying factors can help in the diagnosis and management of narcolepsy.
Treatment for Narcolepsy
Treatment for Narcolepsy typically involves a combination of medications and lifestyle adjustments to manage the symptoms and improve the quality of life for individuals with this sleep disorder. Stimulant medications are often prescribed to help increase wakefulness and reduce excessive daytime sleepiness. These medications, such as modafinil or armodafinil, work by stimulating the central nervous system and promoting alertness. Additionally, selective norepinephrine reuptake inhibitors (SNRIs) and selective serotonin reuptake inhibitors (SSRIs) may be prescribed to help manage narcolepsy symptoms, as they can help regulate sleep-wake cycles and alleviate cataplexy and other symptoms.
Lifestyle adjustments are also crucial in managing narcolepsy. Establishing a consistent sleep schedule is essential to help regulate sleep patterns. It is recommended to prioritize regular, sufficient sleep each night and implement scheduled naps throughout the day to combat excessive sleepiness. Creating a sleep-conducive environment, utilizing relaxation techniques before bedtime, and avoiding stimulating activities and substances close to bedtime are also beneficial.
In addition to medication and lifestyle adjustments, behavioral therapies can be beneficial for individuals with narcolepsy. Cognitive-behavioral therapy (CBT) can help address any underlying psychological issues related to narcolepsy and assist in developing coping strategies. Some individuals may also benefit from support groups and counseling to manage the emotional and social challenges associated with narcolepsy.
It’s important for individuals with narcolepsy to work closely with healthcare professionals to find the most effective treatment plan for their specific needs. Regular follow-ups and communication with healthcare providers are critical to monitor progress and make any necessary adjustments to the treatment regimen.
Restless Legs Syndrome

Restless Legs Syndrome (RLS) is a neurological condition that causes an uncontrollable urge to move the legs, often accompanied by uncomfortable sensations. Symptoms of Restless Legs Syndrome include a crawling or tingling sensation in the legs, an irresistible urge to move the legs, worsening of symptoms at rest, and relief through movement. This condition can disrupt sleep and lead to daytime fatigue and irritability. The exact cause of Restless Legs Syndrome is unknown, but it is believed to involve a combination of genetic and environmental factors. Treatment for Restless Legs Syndrome may involve lifestyle changes such as regular exercise, avoiding caffeine and alcohol, and taking warm baths before bedtime. Medications may also be prescribed to manage the symptoms of RLS. If you’re interested in learning more about the impact of sleep disorders on mental health, you can check out our article on the link between sleep disorders and mental health.
Symptoms of Restless Legs Syndrome
Restless Legs Syndrome (RLS) is a sleep disorder that can cause uncomfortable sensations in the legs and an irresistible urge to move them. The symptoms of Restless Legs Syndrome typically worsen during periods of inactivity, such as when sitting or lying down, and are most prominent in the evening or at night. Individuals with RLS often describe unpleasant sensations, such as creeping, crawling, tingling, or itching, deep within their legs. These sensations can range from mild to severe and can vary in frequency and intensity. People with RLS often feel a strong urge to move their legs to relieve these sensations, which can temporarily provide relief. However, this relief is often short-lived, and the symptoms of RLS can return shortly after ceasing movement. The restless legs and accompanying discomfort can significantly disrupt sleep, leading to excessive daytime sleepiness and fatigue. In severe cases, RLS can even interfere with daily activities and quality of life.
Causes of Restless Legs Syndrome
The causes of restless legs syndrome can vary, and in many cases, the exact underlying cause is unknown. However, there are several factors that have been associated with the development of this condition. Here are some possible causes of restless legs syndrome:
1. Genetics: Studies have shown that there is a genetic component to restless legs syndrome. Individuals with a family history of the disorder are more likely to develop it themselves.
2. Dopamine dysfunction: Restless legs syndrome has been linked to abnormalities in the dopamine pathway in the brain. Dopamine is a neurotransmitter that plays a crucial role in controlling movement and muscle activity. When there is a disruption in dopamine function, it can contribute to the symptoms of restless legs syndrome.
3. Iron deficiency: Low levels of iron in the brain may also play a role in the development of restless legs syndrome. Iron is essential for dopamine production and function, so a deficiency can impact the dopamine signaling in the brain.
4. Pregnancy: Restless legs syndrome is known to be more common during pregnancy. The hormonal changes and increased blood volume during pregnancy may contribute to the symptoms.
5. Chronic diseases: Certain chronic conditions, such as kidney failure, diabetes, and peripheral neuropathy, have been associated with restless legs syndrome. The exact mechanisms linking these conditions to restless legs syndrome are still being studied.
6. Medications: Some medications, including certain antidepressants, antipsychotics, and antihistamines, can trigger or worsen symptoms of restless legs syndrome.
It’s important to note that while these factors may contribute to the development of restless legs syndrome, individual experiences may vary. It is always recommended to consult a healthcare professional for a proper diagnosis and personalized treatment plan. If you want to learn more about the impact of sleep disorders on mental health, you can check our guide on the impact of sleep disorders on mental health.
Treatment for Restless Legs Syndrome
1. Lifestyle Changes: Making certain lifestyle changes can help improve the symptoms of restless legs syndrome (RLS). These may include:
– Regular exercise: Engaging in moderate exercise can alleviate symptoms and promote better sleep.
– Avoiding caffeine and alcohol: Both substances can worsen RLS symptoms, so it is best to minimize or avoid them altogether.
– Massage and hot baths: Massaging the legs and taking warm baths before bed can provide temporary relief.
2. Medications: In some cases, medication may be prescribed to manage the symptoms of RLS. These medications include:
– Dopamine agonists: Medications that mimic the effects of dopamine, a chemical messenger in the brain, can help reduce RLS symptoms.
– Benzodiazepines: These sedative medications can promote relaxation and relieve discomfort associated with RLS.
– Anticonvulsants: Certain anticonvulsant drugs may be prescribed to control the abnormal sensations and movements caused by RLS.
– Iron supplements: For individuals with iron deficiency, iron supplements may be prescribed to address the underlying cause of RLS.
3. Alternative Therapies: Some individuals find relief from RLS symptoms through alternative therapies like acupuncture, yoga, and meditation. While further research is needed to determine their efficacy, these therapies may be worth exploring for individuals seeking additional relief.
4. Ruling out Underlying Conditions: It is important to identify and address any underlying medical conditions that may be causing or exacerbating RLS. These conditions may include iron deficiency, peripheral neuropathy, kidney disease, or diabetes. Treating these underlying conditions can have a positive impact on RLS symptoms.
Consulting a healthcare professional is crucial for establishing an accurate diagnosis and developing an appropriate treatment plan. They will help determine the best course of action tailored to the individual’s specific needs and medical history. Treating RLS can significantly improve sleep quality and overall quality of life.
Sleep Apnea

Sleep apnea is a sleep disorder characterized by pauses in breathing or shallow breathing during sleep. These pauses can last for a few seconds to a few minutes and may occur multiple times throughout the night. Symptoms of sleep apnea include loud snoring, episodes of gasping or choking during sleep, daytime sleepiness, and morning headaches. There are two main types of sleep apnea: obstructive sleep apnea (OSA) and central sleep apnea (CSA). OSA is caused by a blockage of the airway, while CSA occurs when the brain fails to send proper signals to the muscles that control breathing. Common causes of sleep apnea include obesity, age, smoking, and family history. Treatment for sleep apnea may involve lifestyle changes, such as weight loss and quitting smoking, as well as the use of continuous positive airway pressure (CPAP) devices or oral appliances to help keep the airway open during sleep. If left untreated, sleep apnea can contribute to various health problems, including high blood pressure, heart disease, and stroke. It is important to seek medical attention if you suspect you may have sleep apnea.
Symptoms of Sleep Apnea
Sleep apnea is a sleep disorder that is characterized by pauses in breathing or shallow breathing during sleep. These pauses can last for a few seconds to several minutes and can occur multiple times throughout the night. The symptoms of sleep apnea can vary from mild to severe and may include loud snoring, gasping or choking sounds during sleep, restless sleep, morning headaches, dry mouth or sore throat upon waking, difficulty concentrating, excessive daytime sleepiness, and irritability. Additionally, if you share a bed or bedroom with someone, they may notice your episodes of breathing pauses or loud snoring. It’s important to note that not everyone with sleep apnea experiences all of these symptoms, and some may not even be aware that they have the disorder. It is crucial to seek medical evaluation if any of these symptoms are present. Sleep apnea is a serious condition that can have negative impacts on both physical and mental health. If left untreated, it can increase the risk of other health issues such as high blood pressure, heart disease, stroke, and diabetes. So, if you suspect that you or someone you know may be experiencing symptoms of sleep apnea, it’s essential to consult with a healthcare professional for a proper diagnosis and appropriate treatment. If you’re interested in learning more about the impact of sleep disorders on mental health, you can explore our comprehensive guide on the connection between sleep disorders and mental health.
Causes of Sleep Apnea
Causes of Sleep Apnea:
There are several factors that can contribute to the development of sleep apnea. It is important to note that sleep apnea can affect individuals of all ages and backgrounds. Below are some of the common causes and risk factors associated with this sleep disorder:
– Obesity: Excess weight and obesity are known to increase the risk of sleep apnea. The accumulation of fat in the upper body, including the neck area, can put pressure on the airway, leading to obstruction and breathing difficulties during sleep.
– Age: Sleep apnea is more prevalent in older adults. The muscles in the throat area tend to lose tone and become more relaxed with age, making it easier for them to collapse and block the airway.
– Gender: Men are more likely to develop sleep apnea compared to women. However, the risk for women increases after menopause, suggesting hormonal factors may play a role.
– Family History: There is evidence to suggest that genetics may be a contributing factor in the development of sleep apnea. If a close family member has been diagnosed with sleep apnea, the risk of developing the condition may be higher.
– Smoking and Alcohol: Smoking and excessive alcohol consumption can contribute to the relaxation of the muscles in the throat and increase the likelihood of airway obstruction during sleep.
– Nasal Congestion: Conditions like allergies, sinus problems, or nasal congestion can make it harder to breathe through the nose, leading to increased reliance on mouth-breathing, which can in turn contribute to sleep apnea.
– Medical Conditions: Certain medical conditions, such as high blood pressure, diabetes, and hormonal disorders, have been associated with an increased risk of sleep apnea.
– Anatomy of the Airway: Some individuals may have naturally narrow airways or structural abnormalities that predispose them to sleep apnea. These may include a large tongue, tonsils, or adenoids, or a small jawbone.
– Sleep Position: Sleeping on the back can worsen sleep apnea symptoms. In this position, gravity can cause the tongue and soft tissues in the throat to collapse more readily, leading to airway blockage.
Understanding the potential causes and risk factors of sleep apnea is crucial for early detection and effective management of the disorder. If you want to learn more about the impact of sleep disorders on mental health, you can check out our article on the impact of sleep disorders on mental health.
Treatment for Sleep Apnea
Treatment for Sleep Apnea aims to alleviate symptoms, improve sleep quality, and reduce the risk of complications. One commonly prescribed treatment option is continuous positive airway pressure (CPAP). This involves wearing a mask over the nose or mouth during sleep, which delivers a constant stream of air to keep the airways open. CPAP machines are highly effective in treating sleep apnea and can significantly improve symptoms such as snoring and daytime sleepiness.
Another treatment option for sleep apnea is BiPAP (bilevel positive airway pressure). BiPAP machines provide different pressures for inhalation and exhalation, making it easier for individuals to breathe out against airway pressure. This option may be prescribed for individuals who cannot tolerate CPAP treatment or have certain medical conditions.
Oral appliances can also be used to treat sleep apnea. These custom-made devices fit in the mouth and help to keep the airway open by repositioning the jaw and tongue. Oral appliances are often recommended for individuals with mild to moderate sleep apnea or those who are unable to use CPAP therapy.
In some cases, surgery may be considered as a treatment option for sleep apnea. Surgical procedures can help to remove excess tissue, correct structural abnormalities, or reposition the jaw to improve airflow. However, surgery is usually reserved for severe cases of sleep apnea where other treatments have been ineffective or when a specific anatomical issue needs to be addressed.
Additionally, lifestyle changes can play a crucial role in managing sleep apnea. These include maintaining a healthy weight, avoiding alcohol and sedatives, sleeping on your side, and practicing good sleep hygiene. These lifestyle modifications can help to reduce the severity of sleep apnea symptoms and improve overall sleep quality.
It is important for individuals with sleep apnea to consult with a healthcare professional to determine the most appropriate treatment plan based on their specific needs and medical history. Treatment for sleep apnea can significantly improve sleep quality, overall health, and quality of life.
REM Sleep Behavior Disorder
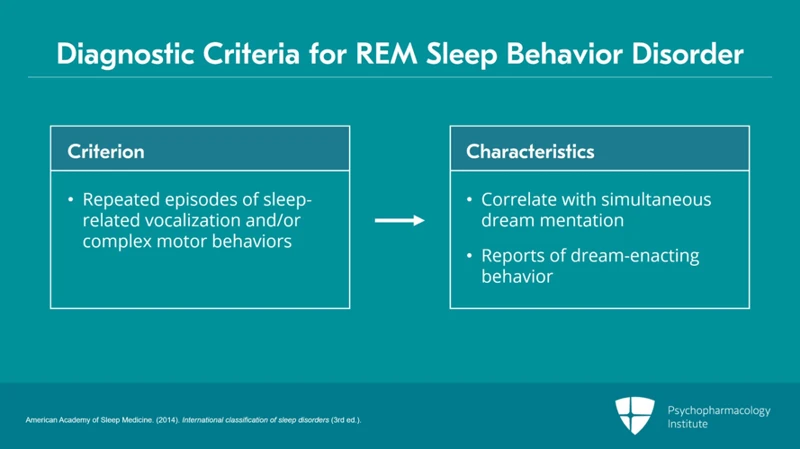
REM Sleep Behavior Disorder (RBD) is a unique sleep disorder that involves the loss of normal muscle paralysis during the REM (Rapid Eye Movement) stage of sleep. This results in individuals physically acting out their dreams, which can be potentially harmful to themselves and their sleep partners. The symptoms of REM Sleep Behavior Disorder include vivid and intense dreams that are often disruptive and violent in nature, accompanied by vocalizations, sudden body movements, and even sleep talking. Unlike other sleep disorders, the exact cause of REM Sleep Behavior Disorder is still unknown, but it has been associated with certain neurological conditions and degenerative disorders. Management and treatment of REM Sleep Behavior Disorder typically involves safety measures to prevent injury during sleep, along with medications that help reduce muscle activity during REM sleep. If you want to learn more about sleep-related conditions, you can check out our comprehensive guide on the understanding of sleep paralysis.
Symptoms of REM Sleep Behavior Disorder
During REM Sleep Behavior Disorder (RBD), an individual typically experiences unusual and often intense physical behavior during the REM (rapid eye movement) phase of sleep. These behaviors can range from simple limb movements to complex and violent actions. Symptoms of REM Sleep Behavior Disorder commonly include vivid and disturbing dreams accompanied by physically acting out these dreams. People with RBD may talk, shout, punch, kick, or even jump out of bed while asleep. This can potentially lead to injuries to themselves or their sleep partners. Some individuals may exhibit behavior that is disruptive and out of character, such as aggression or being combative during sleep. It is important to note that these behaviors occur during REM sleep, which is normally a state of temporary paralysis that prevents physical movements during dreaming. The exact cause of RBD is not yet fully understood, but it is associated with neurological conditions such as Parkinson’s disease, multiple system atrophy, and Lewy body dementia. Diagnosis of RBD typically involves a comprehensive evaluation conducted by a sleep specialist, which may include a detailed medical history, sleep diary, and sometimes a sleep study. If you are experiencing symptoms of RBD or know someone who is, seeking medical attention is crucial to determine an accurate diagnosis and develop a suitable treatment plan.
Causes of REM Sleep Behavior Disorder
The exact causes of REM Sleep Behavior Disorder (RBD) are not yet fully understood, but several factors have been identified as potential contributors to its development. Some of the possible causes of RBD include:
1. Neurodegenerative disorders: RBD is commonly associated with neurodegenerative disorders, such as Parkinson’s disease, multiple system atrophy, and Lewy body dementia. These conditions disrupt the normal functioning of the brain structures involved in regulating REM sleep, leading to the loss of muscle atonia during dreams.
2. Medications: Certain medications, including antidepressants, antipsychotics, and some sleep aids, have been linked to the development of RBD. These drugs can interfere with the brain’s control over muscle paralysis during REM sleep, resulting in the manifestation of dream-enacted behaviors.
3. Brainstem abnormalities: Structural abnormalities in the brainstem, where the sleep-wake cycle is regulated, have been associated with RBD. Damage or dysfunction in this region can disrupt the inhibitory mechanisms that prevent muscle activity during REM sleep.
4. Genetic factors: Some cases of RBD have been found to have a genetic component. Specific gene mutations or variations may predispose individuals to develop RBD, although more research is needed to fully understand the genetic mechanisms involved.
It’s important to note that RBD can also occur idiopathically, meaning that there may be no identifiable cause. In such cases, the disorder seems to arise spontaneously without any underlying medical condition or external factors. Further research is needed to shed more light on the causes of RBD and the complex interplay between various factors contributing to its development.
Treatment for REM Sleep Behavior Disorder
Treatment for REM Sleep Behavior Disorder:
1. Medications: The primary treatment for REM Sleep Behavior Disorder (RBD) involves the use of medications. Clonazepam (Klonopin) is commonly prescribed as it helps reduce the movement and episodes of acting out dreams during REM sleep. Other medications such as melatonin and certain antidepressants may also be used to control symptoms.
2. Lifestyle modifications: Making certain lifestyle changes can also help manage REM Sleep Behavior Disorder. These include avoiding alcohol and caffeine consumption, as they can worsen symptoms. Creating a relaxing bedtime routine, maintaining a regular sleep schedule, and establishing a sleep-friendly environment can promote better sleep quality and reduce the occurrence of episodes.
3. Safety precautions: To prevent potential injuries during RBD episodes, it’s vital to take safety precautions. This may involve securing or removing sharp objects, positioning pillows or cushions around the bed, and ensuring the sleeping area is free from hazards.
4. Psychological support: In some cases, individuals with RBD may benefit from psychological support, such as therapy or counseling. These interventions can help address any underlying psychological issues that may contribute to the disorder and provide coping strategies for managing symptoms.
Remember, treatment approaches may vary depending on the severity and individual needs of each person with REM Sleep Behavior Disorder. It’s essential to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan.
Nightmares
Nightmares are vivid, disturbing dreams that can cause intense fear, anxiety, and even a sense of terror. These unsettling dreams often awaken individuals from their sleep, leaving them feeling fearful and agitated. The symptoms of nightmares include vivid and detailed recollections of the dream, rapid heart rate, sweating, and an overwhelming sense of fear or horror. Causes of nightmares can vary, ranging from stress and anxiety to medications, sleep deprivation, and certain sleep disorders. Some individuals may also experience nightmares as a result of trauma or pre-existing mental health conditions. Treating nightmares often involves identifying and addressing the underlying cause, practicing relaxation techniques before bed, and creating a calming sleep environment. For parents concerned about their children’s nightmares, our article on managing nightmares in children provides helpful tips and strategies.
Symptoms of Nightmares
Nightmares can be incredibly unsettling and can leave individuals feeling anxious and fearful even after they wake up. Here are some of the common symptoms experienced by individuals who suffer from nightmares:
- Vivid and Distressing Dreams: Nightmares are characterized by vivid imagery and intense emotions. These dreams often involve threats to personal safety or well-being, and individuals may wake up feeling frightened or distressed.
- Recollection of the Dream: Unlike other sleep disorders, nightmares are often remembered in detail upon waking up. Individuals may recall specific aspects of the dream, including the storyline, characters, and settings.
- Physical Symptoms: Nightmares can evoke physical reactions in the body. Individuals may experience increased heart rate, rapid breathing, sweating, and trembling during or after a nightmare episode.
- Disturbed Sleep: Nightmares can disrupt the normal sleep cycle, causing frequent awakenings and difficulty falling back asleep. This can lead to feelings of fatigue or exhaustion during the day.
- Irritability and Distress: Waking up from a nightmare can leave individuals feeling anxious, irritable, or troubled. The lingering emotions from these intense dreams can impact mood and overall well-being.
- Fear of Going to Sleep: Fear of experiencing another nightmare can develop, leading to anxiety around bedtime and reluctance to fall asleep. This fear can contribute to sleep difficulties and further exacerbate the impact of nightmares on daily life.
Recognizing these symptoms is crucial in identifying and addressing the presence of nightmares. If nightmares are significantly impacting your quality of life, it may be helpful to seek professional guidance to develop strategies for managing and reducing the frequency of these distressing dreams. To learn more about sleep disorders and their impact on mental health, you can refer to our article on the impact of sleep disorders on mental health.
Causes of Nightmares
Nightmares can be caused by a variety of factors, ranging from psychological to physiological. Understanding the potential causes can help shed light on why someone may be experiencing frequent nightmares. Here are some possible causes of nightmares:
- Stress and Anxiety: High levels of stress and anxiety can contribute to the occurrence of nightmares. When we are stressed or anxious, our brain remains active during sleep, which can lead to vivid and disturbing dreams.
- Traumatic Experiences: Trauma, such as having been in a car accident or experiencing a natural disaster, can lead to the development of nightmares. The brain processes and tries to make sense of traumatic events during sleep, resulting in nightmares.
- Medications and Substances: Certain medications, such as antidepressants, blood pressure medications, and sleep aids, have been known to cause nightmares as a side effect. Additionally, the use of substances like alcohol and illicit drugs can disrupt the sleep cycle and contribute to the occurrence of nightmares.
- Sleep Disorders: Sleep disorders, such as sleep apnea and restless legs syndrome, can increase the likelihood of nightmares. These disorders interfere with the sleep cycle and can lead to more vivid and intense dreams.
- Eating Habits: Consuming heavy meals or spicy foods close to bedtime may increase the risk of nightmares. These foods can affect the digestive system and lead to disrupted sleep, which can trigger nightmares.
- Emotional Upheaval: Major life changes, emotional upheaval, or unresolved emotional issues can cause an increase in nightmares. These dreams may serve as a way for the brain to process and work through these difficult emotions.
- Sleep Deprivation: Lack of sufficient sleep, whether due to insomnia or other factors, can lead to an increase in nightmares. When the body is sleep-deprived, it can affect the REM (rapid eye movement) stage of sleep, where most dreams occur.
It’s important to note that while these factors can contribute to the occurrence of nightmares, each individual’s experience may vary. Identifying and addressing the underlying cause of frequent nightmares can help in finding appropriate treatment or coping strategies. If you would like to learn more about sleep disorders and their impact on mental health, you can check out our comprehensive guide on the impact of sleep disorders on mental health.
Treatment for Nightmares
Treatment for Nightmares can vary depending on the underlying cause and severity of the nightmares. Here are some common approaches to managing and treating nightmares:
1. Trauma-focused therapy: If the nightmares are related to past trauma, therapy techniques such as cognitive processing therapy (CPT) or eye movement desensitization and reprocessing (EMDR) may be recommended. These therapies aim to address and process the traumatic memories and reduce the occurrence of nightmares.
2. Image Rehearsal Therapy (IRT): This therapy involves rewriting and rehearsing the content of nightmares during waking hours. By visualizing an alternative, less distressing outcome, individuals can reduce the frequency and intensity of nightmares over time.
3. Medications: In some cases, medications may be prescribed to help manage nightmares. This may include medications such as Prazosin, which is commonly used to treat nightmares associated with post-traumatic stress disorder (PTSD).
4. Relaxation Techniques: Learning relaxation techniques, such as deep breathing exercises, progressive muscle relaxation, or mindfulness meditation, can help reduce anxiety and promote a more restful sleep, potentially decreasing the occurrence of nightmares.
5. Sleep Hygiene Practices: Establishing good sleep hygiene practices can also be beneficial in managing nightmares. This may include maintaining a consistent sleep schedule, creating a comfortable sleep environment, avoiding stimulating activities before bedtime, and limiting the consumption of caffeine and alcohol.
6. Identifying Triggers: Keeping a dream journal and identifying any potential triggers or patterns in the nightmares can be helpful. By recognizing and addressing these triggers, individuals can work towards resolving the underlying issues contributing to the nightmares.
7. Support Groups: Joining a support group or seeking counseling can provide a safe space to discuss nightmares and share experiences with others who may be going through similar struggles. This can offer additional support and validation.
Remember, it’s essential to consult with a healthcare professional or sleep specialist to determine the most appropriate treatment approach for nightmares. They can assess your specific situation and provide personalized recommendations for effective management. If you want to learn more about the impact of sleep disorders on mental health, you can check out our comprehensive guide on the impact of sleep disorders on mental health.
Sleepwalking
Sleepwalking, also known as somnambulism, is a sleep disorder that involves performing complex behaviors while asleep. The symptoms of sleepwalking typically involve getting out of bed and walking or performing other activities, such as talking, eating, or even driving, while still in a state of sleep. Sleepwalkers often have a blank stare and may appear confused or disoriented when awakened. The exact causes of sleepwalking are not fully understood, but certain factors like sleep deprivation, underlying medical conditions, and family history can contribute to its development. Treatment for sleepwalking often involves creating a safe sleeping environment to prevent injury, implementing good sleep hygiene practices, and addressing any underlying issues that may be contributing to the sleepwalking episodes. In some cases, medications or therapies, such as hypnosis or relaxation techniques, may be recommended to manage sleepwalking.
Symptoms of Sleepwalking
Sleepwalking, also known as somnambulism, is a sleep disorder characterized by complex actions performed during sleep. People who sleepwalk may exhibit a variety of symptoms, which can vary in intensity and frequency. Here are some common symptoms of sleepwalking:
1. Walking or moving around: Sleepwalkers typically get out of bed and move around, often in a slow and clumsy manner. They may wander aimlessly within their sleep environment or even venture into different rooms.
2. Incoherent speech: Sleepwalkers may occasionally mumble or speak unintelligibly while sleepwalking. Their speech is often disorganized and may not make sense to those around them.
3. Blank or glassy-eyed expression: While sleepwalking, individuals typically have a vacant or glassy-eyed look. They may appear dazed and unaware of their surroundings.
4. Performing routine actions: Some sleepwalkers engage in routine activities during their episodes, such as getting dressed, eating, or rearranging objects. These actions may seem purposeful but are performed unconsciously.
5. Agitation or confusion upon awakening: When a sleepwalker is awakened during an episode, they might feel confused, disoriented, or agitated, as they have no recollection of their sleepwalking behavior.
6. Clumsiness or unsteady movements: Sleepwalkers may display uncoordinated movements, stumbling, or bumping into objects due to impaired motor control during sleepwalking episodes.
It is essential to note that sleepwalking can pose some risks, such as leaving the safety of the house or engaging in potentially dangerous activities unknowingly. Taking safety precautions, such as keeping the sleep environment free of potential hazards, is crucial for individuals who experience sleepwalking. If you want to learn more about sleep disorders and their impact on mental health, check out our comprehensive guide on the impact of sleep disorders on mental health.
Causes of Sleepwalking
While the exact cause of sleepwalking is not fully understood, there are several factors that may contribute to this puzzling phenomenon. Genetic predisposition is believed to play a role, as sleepwalking tends to run in families. Certain medical conditions or medications can also increase the likelihood of sleepwalking. For example, sleepwalking may be more common in individuals with sleep disorders such as sleep apnea or restless legs syndrome. Additionally, certain medications, particularly those used to treat psychiatric disorders, may have sleepwalking as a side effect. Sleep deprivation or irregular sleep schedules can also trigger sleepwalking episodes. Stress and anxiety have been linked to sleepwalking, as they can disrupt the normal sleep patterns and increase the likelihood of nighttime wandering. Interestingly, alcohol consumption and substance abuse have also been associated with sleepwalking. While these factors have been identified as potential triggers, it is important to note that they do not necessarily cause sleepwalking in every individual.
Treatment for Sleepwalking
When it comes to the treatment for sleepwalking, the primary goal is to ensure the safety of the individual and minimize the frequency and intensity of sleepwalking episodes. Here are several approaches that may be used in the treatment of sleepwalking:
- Creating a Safe Sleep Environment: Removing any potential hazards or obstacles from the bedroom can help prevent injuries during sleepwalking episodes. This may involve keeping the bedroom clutter-free, installing safety gates on staircases, and securing windows and doors.
- Establishing Consistent Sleep Patterns: Maintaining a regular sleep schedule can help regulate the sleep cycle and reduce the likelihood of sleepwalking. Adequate sleep and a relaxed bedtime routine are also essential factors in managing sleepwalking episodes.
- Avoiding Triggers: Identifying and avoiding triggers that may contribute to sleepwalking can be helpful. These triggers may include sleep deprivation, excessive stress, certain medications, and the consumption of alcohol or caffeine close to bedtime.
- Stress Management: Implementing stress-reducing techniques, such as relaxation exercises, meditation, or therapy, can assist in managing sleepwalking episodes that are associated with stress or anxiety.
- Medication: In some cases, medication may be prescribed to help control sleepwalking. However, the use of medication is typically reserved for severe cases or when other non-pharmacological approaches have been ineffective.
- Underlying Condition Treatment: Sleepwalking can sometimes be a symptom of an underlying medical condition, such as sleep apnea or restless legs syndrome. In such cases, treating the underlying condition may help alleviate sleepwalking episodes.
It’s important to note that treatment approaches may vary depending on the individual and the severity of the sleepwalking episodes. Consulting with a healthcare professional specialized in sleep disorders can provide a more personalized and effective treatment plan.
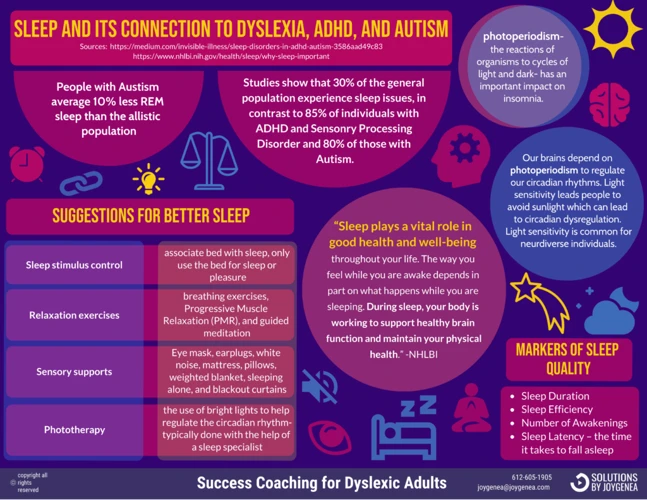
Shift Work Sleep Disorder
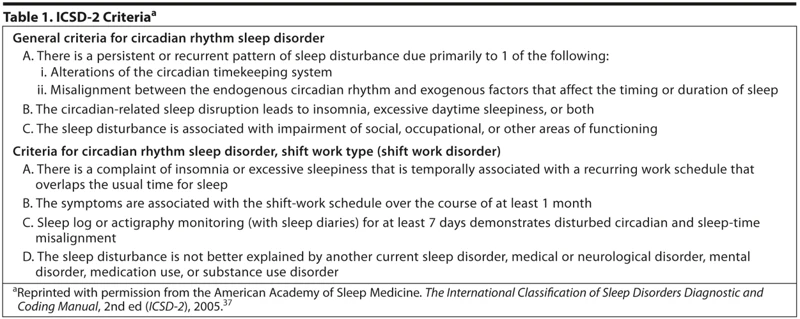
Shift Work Sleep Disorder is a sleep disorder that affects individuals who work non-traditional hours, such as night shifts or rotating shifts. The symptoms of Shift Work Sleep Disorder include excessive sleepiness during working hours, difficulty falling asleep or staying asleep, and general fatigue. These symptoms can significantly impact an individual’s quality of life and overall well-being. The causes of Shift Work Sleep Disorder are multifaceted, involving a disruption of the body’s natural sleep-wake cycle, also known as the circadian rhythm. Factors such as irregular sleep patterns, exposure to bright light at night, and the general challenges of adjusting to a non-traditional work schedule contribute to this disorder. Treatment for Shift Work Sleep Disorder focuses on managing sleep patterns and promoting optimal wakefulness during work hours. Strategies may include maintaining a consistent sleep schedule, creating a sleep-conducive environment, and taking short naps during breaks. Additionally, light therapy and medications that promote wakefulness may be utilized for individuals struggling with this disorder. If you want more information about the impact of sleep disorders on mental health, you can check out our guide here.
Symptoms of Shift Work Sleep Disorder
Shift Work Sleep Disorder is a sleep disorder that specifically affects individuals who work non-traditional or rotating shifts. As the name suggests, the symptoms of Shift Work Sleep Disorder are predominantly related to sleep disturbances. One of the main symptoms is excessive sleepiness or difficulty staying awake during work hours, which can significantly impair job performance and increase the risk of accidents. Individuals with this disorder may also experience difficulty falling asleep or staying asleep when they are off-shift, leading to chronic sleep deprivation. Other symptoms include irritability, difficulty concentrating, decreased energy levels, and a general feeling of fatigue. It is important to note that not everyone who works non-traditional shifts will develop Shift Work Sleep Disorder, but those who do experience these symptoms should seek medical evaluation and consider implementing strategies to improve their sleep quality.
Causes of Shift Work Sleep Disorder
The causes of Shift Work Sleep Disorder are directly linked to the disruption of the body’s natural sleep-wake cycle due to irregular or overnight work schedules. Here are some key factors contributing to the development of this sleep disorder:
1. Shift Work Schedule: Working night shifts, rotating shifts, or irregular schedules can cause a misalignment between the body’s internal clock and the external environment. This disconnection can confuse the body about when it should be awake or asleep, leading to sleep disturbances.
2. Light Exposure: Exposure to bright light during the night shift and trying to sleep during the day can interfere with the body’s production of melatonin, a hormone that regulates sleep-wake cycles. This disruption can make it challenging to fall asleep and stay asleep during the daytime.
3. Workload and Job Demands: Shift work often involves demanding physical or mental tasks, which can increase stress levels and make it harder to relax and unwind before sleep. High job demands and irregular work schedules can contribute to heightened levels of anxiety and sleep difficulties.
4. Social and Family Obligations: Shift workers may face challenges in balancing work responsibilities with family and social obligations. Juggling these responsibilities while trying to maintain good sleep habits can be challenging, leading to increased stress and sleep disturbances.
5. Lifestyle Factors: Shift workers often face lifestyle challenges, such as irregular meal times, limited access to healthy food options, and decreased opportunities for physical activity. These factors can negatively impact overall sleep quality and exacerbate shift work sleep disorder symptoms.
It’s important for individuals with shift work sleep disorder to take steps to manage their condition effectively. Creating a consistent sleep routine, optimizing the sleep environment, and implementing strategies to promote relaxation and stress reduction can help mitigate the effects of this sleep disorder. For more information on how sleep disorders can impact mental health, check out our article on the impact of sleep disorders on mental health.
Treatment for Shift Work Sleep Disorder
Treatment for Shift Work Sleep Disorder:
1. Adjusting the Sleep Environment:
– Creating a dark, quiet, and comfortable sleep environment can help promote better sleep during the day.
– Using blackout shades or curtains to block out sunlight can be beneficial for shift workers trying to sleep during daylight hours.
2. Establishing a Consistent Sleep Schedule:
– Maintaining a regular sleep routine, even on non-work days, can help regulate the body’s internal clock.
– Going to bed and waking up at the same time each day can improve sleep quality and reduce the symptoms of shift work sleep disorder.
3. Taking Strategic Naps:
– Incorporating short naps during breaks or before the shift can help combat fatigue and sleepiness.
– Limiting the duration of naps to 20-30 minutes can prevent grogginess upon waking.
4. Light Therapy:
– Exposure to bright light, such as using specialized light boxes or lamps, can help reset the body’s internal clock and promote wakefulness during work hours.
– Limiting exposure to bright light, particularly blue light, in the hours leading up to bedtime can help signal the body to prepare for sleep.
5. Healthy Lifestyle Habits:
– Engaging in regular exercise, maintaining a balanced diet, and avoiding excessive caffeine or alcohol consumption can contribute to better sleep quality.
– Establishing a wind-down routine before bedtime, such as reading or taking a warm bath, can help signal to the body that it’s time to relax and prepare for sleep.
6. Medications and Supplements:
– In some cases, doctors may prescribe medications, such as melatonin or prescription sleep aids, to help regulate sleep patterns and manage the symptoms of shift work sleep disorder.
– It’s important to consult with a healthcare professional before starting any medication or supplement regimen.
Remember, the effectiveness of treatment options may vary from person to person, so it’s essential to find a personalized approach that works best for managing shift work sleep disorder.
Delayed Sleep Phase Disorder
Delayed sleep phase disorder (DSPD) is a circadian rhythm sleep disorder characterized by a persistent delay in the timing of sleep, making it difficult for individuals to fall asleep and wake up at desired or socially acceptable times. People with delayed sleep phase disorder often experience a shift in their biological clock, causing them to naturally feel more alert and awake during the late evening and nocturnal hours. The symptoms of delayed sleep phase disorder include going to bed and waking up later than desired, prolonged sleep latency (the time it takes to fall asleep), and difficulty adjusting to an earlier sleep schedule. The causes of delayed sleep phase disorder can vary, but it is commonly associated with an imbalance in the body’s melatonin production, as well as factors such as genetics, lifestyle choices, and exposure to light. Treatment for delayed sleep phase disorder often involves implementing strategies to reset the sleep-wake schedule, such as gradually advancing bedtime and wake-up times, using bright light therapy, and avoiding stimulants close to bedtime. If you want to learn more about sleep disorders and their impact on mental health, you can check out our article on the impact of sleep disorders on mental health.
Symptoms of Delayed Sleep Phase Disorder
Delayed Sleep Phase Disorder (DSPD) is a sleep disorder characterized by a persistent delay in the timing of sleep. People with DSPD often have trouble falling asleep at a conventional bedtime and struggle to wake up at a socially acceptable time in the morning. Here are some common symptoms of Delayed Sleep Phase Disorder:
- Difficulty falling asleep: Individuals with DSPD often find it difficult to fall asleep at night, even when they feel tired. They may toss and turn in bed for hours before finally being able to fall asleep.
- Delayed sleep onset: Instead of feeling sleepy in the evening like most people, individuals with DSPD experience a delayed sleep onset. This can result in them staying awake until the early hours of the morning.
- Excessive daytime sleepiness: Despite going to bed late, individuals with DSPD still need to wake up early for work, school, or other obligations. This leads to a chronic lack of sleep, resulting in excessive daytime sleepiness and feeling groggy throughout the day.
- Irregular sleep-wake pattern: People with DSPD often have an irregular sleep-wake pattern, going to bed and waking up much later than the average person. This misalignment between their internal body clock and the societal norms can cause significant disruptions in their daily lives.
- Difficulty waking up: Due to staying awake until late at night, individuals with DSPD may struggle to wake up in the morning, even with the help of alarms. They often feel groggy and struggle with morning tasks or responsibilities.
If you or someone you know is experiencing these symptoms, it may be worth seeking medical advice or consulting a sleep specialist for an accurate diagnosis and appropriate treatment options.
Causes of Delayed Sleep Phase Disorder
Delayed Sleep Phase Disorder (DSPD) is a sleep disorder characterized by a delayed timing of the sleep-wake cycle. It commonly affects teenagers and young adults. The causes of Delayed Sleep Phase Disorder are not yet fully understood. However, several factors have been identified as potential contributors to the development of this condition.
One of the main causes of Delayed Sleep Phase Disorder is believed to be a disruption in the body’s internal clock, known as the circadian rhythm. The circadian rhythm regulates various biological processes, including sleep-wake cycles. In individuals with DSPD, this internal clock is often set to a later time compared to the standard sleep schedule. This delayed timing makes it difficult for them to fall asleep and wake up at the desired times.
Genetics also play a role in the development of Delayed Sleep Phase Disorder. Studies have shown that there may be genetic variations associated with the regulation of the circadian rhythm. Certain genetic mutations or abnormalities in specific genes involved in the sleep-wake cycle can contribute to the delayed timing of sleep in individuals with DSPD.
Environmental factors can also influence the development of Delayed Sleep Phase Disorder. Irregular sleep schedules, exposure to bright light at night, and excessive use of electronic devices before bedtime can disrupt the circadian rhythm and contribute to a delayed sleep phase.
In some cases, Delayed Sleep Phase Disorder may occur secondary to other medical or psychiatric conditions. Conditions such as depression, anxiety, attention-deficit/hyperactivity disorder (ADHD), and certain neurological disorders have been associated with DSPD. These conditions may exacerbate sleep disturbances and contribute to a delayed sleep phase.
The causes of Delayed Sleep Phase Disorder are multifactorial and can involve disruptions in the circadian rhythm, genetic predisposition, environmental factors, and comorbid medical or psychiatric conditions. Understanding the underlying causes is crucial for developing effective treatment strategies for individuals with DSPD. If you are interested in learning about how sleep disorders can impact mental health, you can check out our article on the impact of sleep disorders on mental health.
Treatment for Delayed Sleep Phase Disorder
Treatment for Delayed Sleep Phase Disorder focuses on shifting the individual’s sleep-wake schedule to a more desired timeframe. Here are a few strategies that can aid in managing this sleep disorder:
1. Light Therapy: Exposure to bright light in the morning can help advance the body’s internal clock and promote earlier sleep onset. Light therapy involves using a lightbox or light visor for a specified duration each day. This simulated natural light can help regulate circadian rhythms and adjust the sleep-wake cycle.
2. Dark Therapy: On the opposite end of the spectrum, minimizing exposure to bright light sources before bedtime can be beneficial. This approach involves wearing blue-blocking glasses, reducing screen time, and creating a dark and relaxing sleep environment to signal to the body that it’s time to sleep.
3. Sleep-Hygiene Practices: Establishing consistent sleep routines and practicing good sleep hygiene can also assist in managing Delayed Sleep Phase Disorder. This includes maintaining a regular sleep schedule, avoiding caffeine and stimulating activities close to bedtime, creating a comfortable sleep environment, and engaging in relaxation techniques before sleep.
4. Melatonin Supplementation: Melatonin is a naturally occurring hormone that regulates sleep-wake cycles. Taking melatonin supplements in the evening, a few hours before the desired bedtime, can help shift the sleep phase earlier. It is essential to consult with a healthcare professional before starting any supplementation.
5. Chronotherapy: In more severe cases, a technique called chronotherapy may be recommended. This approach involves gradually adjusting the sleep schedule by systematically delaying the bedtime by a few hours each day until reaching the desired sleep-wake time. It can be an effective but challenging method and should be done under the guidance of a sleep specialist.
Remember, it is important to consult with a healthcare professional or sleep specialist to determine the most suitable treatment plan for each individual with Delayed Sleep Phase Disorder. They can provide personalized recommendations and guidance based on the specific needs and challenges of the individual’s sleep pattern.
Exploding Head Syndrome
Exploding Head Syndrome is a rare and perplexing sleep disorder that can cause intense and startling auditory hallucinations. Individuals with often report hearing loud noises, such as explosions or thunderclaps, just as they are falling asleep or waking up. These hallucinations can be incredibly vivid and disturbing, causing significant distress and anxiety. While the exact causes of Exploding Head Syndrome are still unknown, researchers speculate that it may be related to abnormal sleep-wake transitions or dysfunction in the auditory pathways of the brain. Treatment for Exploding Head Syndrome typically involves reassurance and education about the benign nature of the condition. In some cases, medications such as calcium channel blockers or tricyclic antidepressants may be prescribed to help alleviate symptoms. It’s important for individuals experiencing Exploding Head Syndrome to seek medical advice and support to better understand and manage this puzzling sleep disorder.
Symptoms of Exploding Head Syndrome
Symptoms of Exploding Head Syndrome can be frightening and bewildering for those who experience them. Exploding Head Syndrome is characterized by sudden and intense noises or sensations that occur in the head as a person is falling asleep or waking up. These sensations can vary from person to person, but they often include the perception of loud noises such as explosions, crashing sounds, or even screams. Some people may also report a feeling of intense pressure or a sensation of an electrical shock throughout the head. These episodes can be accompanied by a rapid heartbeat, sweating, and a sense of panic or fear. It is important to note that although the experiences can be alarming, Exploding Head Syndrome is not associated with any physical harm or underlying medical condition. Most individuals who experience this sleep disorder do not require treatment, as the symptoms often spontaneously resolve over time. However, if the symptoms of Exploding Head Syndrome are causing significant distress or adversely impacting sleep quality, a healthcare professional may recommend certain techniques or therapies to manage the condition.
Causes of Exploding Head Syndrome
The causes of Exploding Head Syndrome are still not fully understood. However, researchers have identified several potential factors that may contribute to the occurrence of this unusual sleep disorder. One theory suggests that abnormalities in the brain’s auditory system may play a role, causing the brain to misinterpret normal sounds as loud explosions. Another possible cause is sleep deprivation or irregular sleep patterns, as these can disrupt the brain’s normal functioning and increase the likelihood of experiencing episodes of Exploding Head Syndrome. Stress and anxiety have also been linked to the occurrence of this syndrome, with high levels of stress potentially triggering the brain’s exaggerated response to sounds during the sleep-wake transition. Additionally, underlying neurological conditions such as migraines, seizures, and Meniere’s disease may increase the risk of developing Exploding Head Syndrome. It’s important to note that more research is needed to fully understand the causes of this condition and to identify effective treatment options. If you want to learn more about other sleep disorders and their impact on mental health, you can check out our guide on the impact of sleep disorders on mental health.
Treatment for Exploding Head Syndrome
Treatment for Exploding Head Syndrome involves a combination of strategies aimed at reducing the frequency and intensity of the episodes. Here are some approaches that may be helpful:
1. Sleep hygiene: Maintaining a consistent sleep schedule, creating a relaxing bedtime routine, and ensuring a quiet and comfortable sleep environment can contribute to better sleep quality and potentially reduce the occurrence of episodes.
2. Stress reduction: Managing stress levels through techniques like relaxation exercises, deep breathing, and mindfulness can help minimize the triggers for Exploding Head Syndrome.
3. Medication adjustment: If the episodes of Exploding Head Syndrome are linked to certain medications, consulting with a healthcare professional to explore potential adjustments or alternatives may be beneficial.
4. Treating underlying conditions: Addressing any underlying conditions that may be contributing to the development of Exploding Head Syndrome, such as anxiety or sleep disorders, can be vital in managing the symptoms.
5. Cognitive-behavioral therapy: Engaging in therapy sessions with a trained therapist can help individuals understand and cope with the episodes, providing tools to lessen the impact and anxiety associated with Exploding Head Syndrome.
It’s important to remember that what works for one person may not work for another, so a personalized approach is often necessary. Seeking guidance from a healthcare professional who specializes in sleep disorders is recommended to develop an effective treatment plan. If you’re interested in learning more about the impact of sleep disorders on mental health, you can check out our comprehensive guide on the impact of sleep disorders on mental health.
Conclusion
In conclusion, understanding the various sleep disorders that can disrupt our nightly routines is crucial for finding effective treatments and regaining restful sleep. Each sleep disorder has its own unique symptoms and causes, making it essential to seek proper diagnosis and professional guidance. Whether you are dealing with the persistent inability to fall asleep (insomnia), sudden and uncontrollable sleep attacks (narcolepsy), or the uncomfortable sensation in your legs that disrupts sleep (restless legs syndrome), there are treatment options available to alleviate the symptoms and improve sleep quality. Proper sleep hygiene practices, lifestyle adjustments, medications, and therapies like cognitive-behavioral therapy for insomnia (CBT-I) or continuous positive airway pressure (CPAP) for sleep apnea can all contribute to better sleep health. It’s important to remember that sleep disorders can have a significant impact on our overall well-being, including our mental health. Therefore, if you are experiencing ongoing sleep issues, it is advisable to consult with a healthcare professional or sleep specialist to address any underlying concerns and develop a personalized treatment plan. By prioritizing good sleep habits and seeking appropriate interventions, you can take significant steps towards enjoying restorative and uninterrupted sleep. For more information on the connection between sleep disorders and mental health, check out our comprehensive guide on the impact of sleep disorders on mental health. Sleep well and wake up refreshed!
Frequently Asked Questions
1. Can insomnia be caused by medical conditions?
Yes, insomnia can be caused by underlying medical conditions such as chronic pain, respiratory disorders, hormonal imbalances, and neurological conditions.
2. Is narcolepsy a genetic disorder?
While the exact cause of narcolepsy is still unknown, research suggests that there may be a genetic predisposition to the disorder.
3. What is the main cause of restless legs syndrome?
The exact cause of restless legs syndrome is not fully understood, but it is believed to be related to abnormalities in the brain’s dopamine levels and iron deficiencies in the body.
4. Can sleep apnea affect children?
Yes, sleep apnea can affect children, particularly those who are overweight or have enlarged tonsils or adenoids.
5. Is REM sleep behavior disorder dangerous?
Yes, REM sleep behavior disorder can be dangerous as it involves acting out vivid dreams during REM sleep, which can lead to injury for the person or their sleep partner.
6. How common are nightmares in adults?
Nightmares are relatively common in adults, with around 4% of adults reporting frequent nightmares.
7. Does sleepwalking only occur in children?
No, sleepwalking can occur in both children and adults, although it is more common in children.
8. What are the risk factors for developing shift work sleep disorder?
Risk factors for developing shift work sleep disorder include working night or rotating shifts, having an irregular work schedule, and working in industries that require extended hours.
9. Can delayed sleep phase disorder be treated?
Yes, delayed sleep phase disorder can be treated through a combination of behavioral interventions, such as adjusting sleep schedules and avoiding stimulating activities before bedtime, and in some cases, medication.
10. Is exploding head syndrome a serious condition?
Exploding head syndrome is not considered a serious condition, but it can be distressing and disruptive to sleep. Treatment may involve managing stress levels and improving sleep hygiene practices.