Are you tired of waking up in strange places with no memory of how you got there? Sleepwalking, a fascinating and often perplexing phenomenon, is a type of sleep disorder that affects individuals during their deep non-REM sleep. It involves complex behaviors, such as walking, talking, and performing activities while asleep. Sleepwalking can have various causes, ranging from genetic factors to sleep deprivation. This article delves into the definition, causes, symptoms, and treatment options for sleepwalking and explores its relationship with other sleep disorders. So, grab a cup of hot tea, relax, and embark on a journey to unravel the mysteries behind sleepwalking and its intriguing connection to the fascinating world of sleep disorders.
Sleepwalking: Definition and Causes

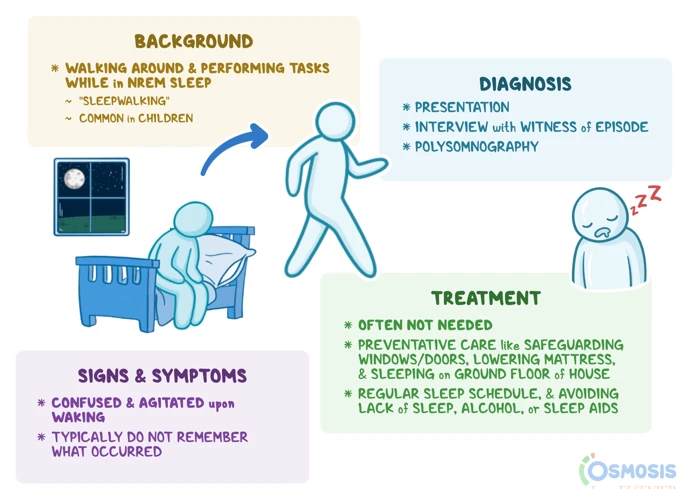
Sleepwalking, also known as somnambulism, is a sleep disorder characterized by complex movements and behaviors performed during deep non-REM sleep. It typically occurs during the first few hours of sleep and involves activities such as sitting up, walking around, or even driving a car. The sleepwalker is not fully aware of their actions and usually has no recollection of the event upon awakening. Sleepwalking can be a perplexing and sometimes alarming experience for both the sleepwalker and those around them. While sleepwalking is most commonly associated with children, it can affect individuals of all ages.
The exact causes of sleepwalking are still not fully understood, but several factors have been identified as potential contributors. Genetic predisposition appears to play a role, as sleepwalking tends to run in families. Stress and anxiety can also trigger sleepwalking episodes, as they disrupt the normal sleep cycle and increase the likelihood of sleep disturbances. Sleep deprivation is another common cause, as it can disrupt the balance between deep sleep and lighter stages of sleep, making sleepwalking more likely. Other factors that may contribute to sleepwalking include fever, certain medications, sleep disorders such as sleep apnea, and environmental factors such as noise or a disruptive sleeping environment.
To further explore the causes and effects of sleepwalking, research has focused on studying the brain during sleepwalking episodes. While there is still much to learn, advancements in neuroimaging techniques have revealed abnormalities in the regions of the brain responsible for motor control and decision-making.
Separating fact from fiction, it is important to debunk some myths surrounding sleepwalking. Contrary to popular belief, waking up a sleepwalker does not cause harm or induce a heart attack. However, it is advisable to guide them gently back to bed to prevent any potential injuries that may occur during their unconscious wanderings.
The causes of sleepwalking are multifactorial, involving a combination of genetic, environmental, and physiological factors. Understanding these underlying causes can pave the way for effective treatment and management strategies for sleepwalkers.
Definition of Sleepwalking
Sleepwalking, also known as somnambulism, is a complex sleep disorder that involves performing activities while in a state of deep non-REM sleep. It is characterized by the sleepwalker engaging in various behaviors, such as walking, talking, eating, or even driving a car, all while remaining asleep. Sleepwalking typically occurs during the first half of the night and is most common in children, although it can persist into adulthood. The sleepwalker may appear to have their eyes open but does not have a clear awareness of their surroundings and is not responsive to external stimuli. Episodes of sleepwalking can last for a few minutes up to half an hour or longer and may end with the person returning to bed on their own or waking up in a confused state. It is important to note that sleepwalking should not be confused with confusional arousals, which are brief episodes of disorientation upon waking up from sleep.
The exact mechanisms underlying sleepwalking are not fully understood, but it is believed to involve an imbalance between the wake and sleep states in the brain during the deeper stages of non-REM sleep. Normally, during deep sleep, the brain inhibits movement to prevent us from acting out our dreams. However, in sleepwalking, this inhibition does not function properly, allowing the individual to engage in complex behaviors while still asleep.
Sleepwalking can be alarming and potentially dangerous, as sleepwalkers may engage in hazardous activities or risk injury. If you or someone you know experiences sleepwalking, it is important to seek treatment options to address the underlying causes and minimize the occurrence of sleepwalking episodes. A medical professional can provide a proper diagnosis and recommend appropriate interventions to promote a better quality of sleep and reduce the incidence of sleepwalking.
Causes of Sleepwalking
Sleepwalking, also known as somnambulism, can be caused by various factors that disrupt the normal sleep patterns and processes. While the exact causes of sleepwalking are not fully understood, several potential contributors have been identified.
Genetic predisposition: Research suggests that there may be a genetic component to sleepwalking. It tends to run in families, suggesting that certain genetic factors may increase the likelihood of sleepwalking episodes. However, the specific genes involved have not been identified yet.
Sleep deprivation: Sleep deprivation or insufficient sleep can disrupt the balance between deep sleep and lighter stages of sleep. This disruption can increase the likelihood of sleepwalking episodes. When the body and brain do not get enough restorative sleep, it can lead to an imbalance in the sleep-wake cycle, making sleepwalking more likely to occur.
Stress and anxiety: High levels of stress and anxiety can also contribute to sleepwalking. These factors disrupt the normal sleep patterns and can lead to sleep disturbances. Sleepwalking may serve as a manifestation of the body’s response to stress, manifesting as complex motor behaviors during sleep.
Medical conditions: Certain medical conditions may also contribute to sleepwalking. For example, individuals with conditions such as sleep apnea, restless legs syndrome (RLS), or gastroesophageal reflux disease (GERD) may be more prone to sleepwalking episodes. These conditions can disrupt sleep and increase the chances of sleepwalking behavior.
Medication and substances: Certain medications and substances can trigger sleepwalking in susceptible individuals. Medications such as sedatives, hypnotics, and antidepressants have been associated with sleepwalking episodes. Additionally, alcohol and sleep-inducing drugs can also increase the risk of sleepwalking.
Environmental factors: Environmental factors can play a role in sleepwalking. Loud noises, disruptions in the sleep environment, and unfamiliar surroundings can increase the likelihood of sleepwalking episodes. Sleepwalking is more common in unfamiliar environments, potentially due to the brain’s heightened arousal response to new surroundings.
While these factors are considered potential causes of sleepwalking, it is important to note that every individual is different, and the triggers for sleepwalking can vary. Identifying and understanding the underlying causes can help guide treatment strategies and management techniques for individuals experiencing sleepwalking episodes.
Common Symptoms of Sleepwalking
Sleepwalking is characterized by a range of physical and behavioral symptoms that occur during deep non-REM sleep. Let’s take a closer look at some of the common symptoms associated with sleepwalking:
Physical Symptoms:
- Walking or moving around: Sleepwalkers often engage in motor activities while asleep, such as walking, wandering aimlessly, or simply sitting up in bed.
- Glassy-eyed appearance: Sleepwalkers may have a vacant or distant look in their eyes, as if they are not fully present.
- Incoherent speech: Sleepwalkers may mumble or talk in their sleep, often speaking nonsensically or in a way that is unrelated to their surroundings or the people present.
- Slow and unresponsive reactions: Sleepwalkers may display slower reflexes and responses to external stimuli.
- Difficulty waking up: Although sleepwalkers may appear to be awake, it can be challenging to rouse them from their sleepwalking state.
Behavioral Symptoms:
- Performing routine activities: Sleepwalkers may engage in routine activities that they typically perform during waking hours, such as getting dressed, eating, or even cooking.
- Agitation or restlessness: Sleepwalkers may exhibit signs of agitation, restlessness, or confusion during an episode.
- Repetitive movements: Some sleepwalkers may repeat certain movements or actions, such as pacing or opening and closing doors repeatedly.
- Unresponsiveness to communication: Sleepwalkers are typically unresponsive to attempts at communication, and their actions and behaviors do not make sense when interacted with.
- No memory of the event: Sleepwalkers usually have no recollection of their sleepwalking episode upon awakening, although they may feel fatigued or disoriented.
It is important to note that symptoms may vary in intensity and frequency among individuals who experience sleepwalking episodes. If you or someone you know exhibits these symptoms regularly, it may be necessary to consult a healthcare professional for further evaluation and guidance.
Physical Symptoms
Physical symptoms are one of the key indicators of sleepwalking. While each individual may experience different physical manifestations, there are common physical symptoms that are often associated with sleepwalking episodes. These symptoms can vary in intensity and duration, and may include:
1. Blank Stares: Sleepwalkers often have a vacant or glassy-eyed look, as if they are not fully present or aware of their surroundings.
2. Slow and Smooth Movements: Sleepwalkers typically exhibit slow, rhythmic movements rather than quick and purposeful actions. Their movements may appear smooth and deliberate, as if they are in a trance-like state.
3. Unresponsiveness: Sleepwalkers are usually unresponsive to attempts at communication or interaction. They may not acknowledge or process external stimuli, such as calling their name or touching them.
4. Open Eyes: Contrary to popular belief, sleepwalkers often have their eyes open during an episode. However, their gaze may be unfocused or distant, reflecting their disengagement from the environment.
5. Automatisms: Sleepwalkers may engage in automatic behaviors, such as dressing or undressing, rearranging objects, or even eating. These activities are typically performed with little consciousness or recollection.
6. Limited Coordination: Sleepwalking can affect motor coordination, making movements appear clumsy or uncoordinated. Sleepwalkers may bump into objects or walls, trip, or stumble while navigating their surroundings.
7. Slow Reaction Time: Sleepwalkers may display delayed responses to external stimuli or commands. They may take longer to process and respond to instructions, showing a reduced level of awareness.
It is important to note that physical symptoms alone may not be enough to diagnose sleepwalking. A comprehensive evaluation by a sleep specialist, including a thorough medical history and possible monitoring during sleep, is necessary for an accurate diagnosis. Understanding the physical symptoms associated with sleepwalking can help individuals and their loved ones recognize and respond to sleepwalking episodes in a safe and supportive manner.
Behavioral Symptoms
During sleepwalking episodes, individuals may exhibit a variety of behavioral symptoms. These symptoms can range from simple and repetitive actions to more complex and purposeful behaviors. Here are some common behavioral symptoms associated with sleepwalking:
- Wandering: Sleepwalkers often get out of bed and wander aimlessly around their surroundings. They may navigate through their house, go outside, or even try to leave the premises.
- Talking: Sleepwalkers may engage in conversations while sleepwalking, although their speech may not be coherent or comprehensible. They may mumble, speak in a monotone voice, or respond to hallucinations.
- Performing Daily Routines: Some sleepwalkers may perform routine activities that they would normally carry out during waking hours. This can include activities such as getting dressed, making a snack, or tidying up their surroundings.
- Aggression: In rare cases, sleepwalkers may display aggressive or violent behaviors while sleepwalking. This can include hitting, pushing, or even attempting to harm themselves or others.
- Disorientation: Sleepwalkers often appear disoriented and have a sense of confusion when waking up from a sleepwalking episode. They may be unaware of their surroundings and have difficulty recalling the event after awakening.
It is important to note that during sleepwalking episodes, individuals may have limited or no memory of their actions upon waking up. They may wake up feeling confused, disoriented, and sometimes embarrassed or ashamed when they discover that they have been sleepwalking.
Understanding these behavioral symptoms can help identify and differentiate sleepwalking from other sleep disorders and nocturnal behaviors. If you or someone you know experiences these symptoms, it is advisable to consult a healthcare professional for a proper diagnosis and guidance on appropriate management strategies.
The Relationship Between Sleepwalking and Other Sleep Disorders
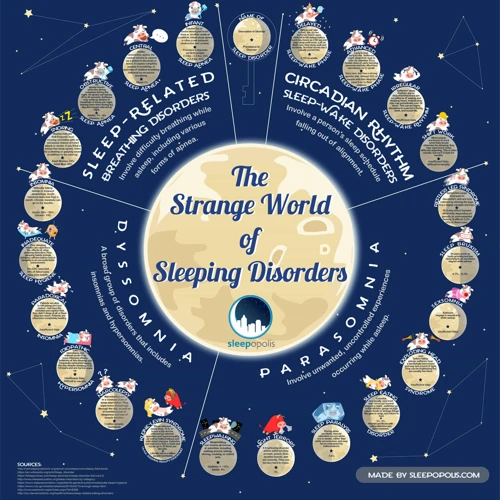
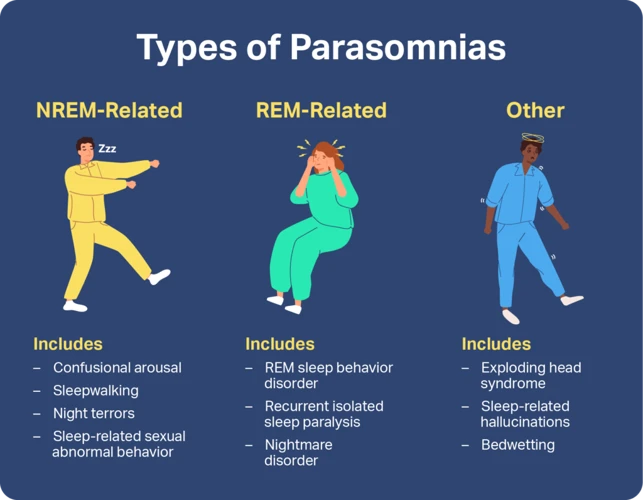
The relationship between sleepwalking and other sleep disorders is a topic of interest in the field of sleep medicine. While sleepwalking is classified as a parasomnia, there are several other sleep disorders that can coexist or have a relationship with sleepwalking. Let’s explore some of these sleep disorders:
1. Night Terrors: Night terrors, also known as sleep terrors, are characterized by sudden and intense episodes of fear or terror during sleep. These episodes typically occur during the first few hours of sleep and are often accompanied by screaming, rapid breathing, and a rapid heart rate. Although sleep terrors and sleepwalking share some similarities, they are distinct disorders. However, it is not uncommon for sleepwalking and sleep terrors to co-occur in individuals.
2. REM Sleep Behavior Disorder (RBD): RBD is a condition where individuals act out their dreams during REM sleep. While most individuals experience temporary muscle paralysis during REM sleep, those with RBD do not have this inhibition, leading to physical movements and even potentially harmful behaviors during sleep. RBD and sleepwalking may have overlapping characteristics, but they are considered separate sleep disorders.
3. Insomnia: Insomnia refers to difficulty falling asleep or staying asleep, which can lead to inadequate sleep quantity or quality. While insomnia and sleepwalking may not seem directly related, disrupted sleep patterns and poor sleep quality can increase the likelihood of sleepwalking episodes. Additionally, anxiety and stress associated with insomnia may also contribute to sleepwalking.
It is important to note that the relationship between sleepwalking and other sleep disorders can vary from person to person. Some individuals may experience multiple sleep disorders concurrently, while others may only have one specific sleep disorder. Understanding these relationships can help healthcare professionals accurately diagnose and treat individuals with sleep disorders.
Sources:
– American Academy of Sleep Medicine. (2014). ICSD-3: International Classification of Sleep Disorders, Third Edition.
– Mahowald, M. W., & Schenck, C. H. (2005). Insights from studying human sleep disorders. Nature, 437(7063), 1279-1285.
Night Terrors
Night terrors, also known as sleep terrors, are a type of sleep disorder that differs from sleepwalking but can occur simultaneously. Night terrors primarily affect children, although they can occur in adults as well. Unlike sleepwalking, which involves physical movement, night terrors are intense episodes of fear or terror during sleep, often accompanied by screaming, thrashing, or intense sweating. These episodes typically occur during the transition from deep non-REM sleep to lighter REM sleep stages.
It is important to note that night terrors are different from nightmares. Nightmares occur during REM sleep and are often vivid dreams that can be recalled upon waking. In contrast, individuals who experience night terrors usually have little to no memory of the episode upon awakening.
The exact cause of night terrors is not well understood, but they may be triggered by various factors. Intense stress, sleep deprivation, fever, and certain medications can contribute to the occurrence of night terrors. Additionally, underlying sleep disorders such as sleep apnea or restless leg syndrome have been associated with an increased likelihood of experiencing night terrors.
The relationship between sleepwalking and night terrors is a complex one. While they are distinct sleep disorders, they can sometimes coexist in the same individual. In some cases, night terrors can even trigger sleepwalking episodes. Both sleepwalking and night terrors share similarities in terms of their potential causes and triggers, such as sleep deprivation and stress.
If night terrors or sleepwalking become frequent or significantly impact one’s daily life, it is important to seek medical evaluation and guidance. A healthcare professional can help determine the underlying causes and develop a personalized treatment plan to manage these sleep disorders effectively.
To learn more about the treatment options for sleepwalking, night terrors, and other related sleep disorders, continue reading our article on treatment options for sleepwalking and associated sleep disorders.
REM Sleep Behavior Disorder
REMP Sleep Behavior Disorder (RBD) is a sleep disorder characterized by vivid, intense, and often violent dream-enactment behaviors. Unlike sleepwalking, RBD occurs during the rapid eye movement (REM) stage of sleep when dreaming is most vivid. During REM sleep, the body typically experiences muscle atonia, which is a temporary paralysis to prevent individuals from physically acting out their dreams. However, in individuals with RBD, this muscle paralysis is absent or incomplete, allowing them to physically act out their dreams.
People with RBD may engage in a range of behaviors during sleep, including talking, shouting, punching, kicking, and even leaping out of bed. These actions can be potentially harmful, not only to the individual experiencing RBD but also to their bed partner. RBD is often associated with neurological conditions such as Parkinson’s disease and other disorders affecting the brainstem. It is believed to result from abnormalities in the brain structures responsible for regulating REM sleep.
Diagnosing RBD generally involves undergoing a sleep study called polysomnography, which monitors brain activity, eye movement, muscle tone, and other physiological parameters during sleep. Treatment options for RBD focus on managing the symptoms and ensuring the safety of the individual and their bed partner.
Medications such as clonazepam, melatonin, or other sedatives may be prescribed to reduce the frequency and intensity of RBD episodes. Making modifications to the sleep environment can also help prevent injuries. For example, using soft padding around the bed or removing sharp objects from the bedroom can minimize the risk of harm during episodes. It is essential to create a safe sleeping environment for individuals with RBD.
Additionally, counseling and therapy may be beneficial, as they can provide emotional support and help individuals cope with any psychological distress associated with RBD. Techniques such as cognitive-behavioral therapy can be useful in managing the disorder. This form of therapy focuses on identifying triggers and developing strategies to modify thoughts and behaviors during sleep.
RBD is a distinct sleep disorder that occurs during the REM stage of sleep and involves vivid dream enactment behaviors. It is essential to properly diagnose and manage RBD to ensure the safety and well-being of individuals experiencing this disorder. With the right combination of medication, environmental modifications, and therapies, individuals with RBD can find relief and minimize the disruptive effects of this condition on their sleep and daily lives.
Insomnia
Insomnia is a sleep disorder characterized by difficulty falling asleep, staying asleep, or both. It can be either acute, lasting for a short period of time, or chronic, persisting for weeks, months, or even years. Insomnia can have a significant impact on an individual’s overall well-being, leading to daytime fatigue, irritability, and difficulty concentrating.
There are several potential causes of insomnia, and it can often be linked to other sleep disorders, including sleepwalking. Here are some common factors associated with insomnia:
1. Stress and Anxiety: Psychological factors such as excessive worrying, racing thoughts, or emotional distress can contribute to insomnia. The mind is unable to relax, making it difficult to fall asleep.
2. Medical Conditions: Certain medical conditions, such as chronic pain, respiratory disorders, hormonal imbalances, and gastrointestinal problems, can disrupt sleep and lead to insomnia.
3. Medications: Certain medications, including some antidepressants, stimulants, and corticosteroids, can interfere with sleep patterns and trigger insomnia as a side effect.
4. Environmental Factors: Noise, light, temperature, and an uncomfortable sleeping environment can all contribute to difficulty falling or staying asleep.
5. Irregular Sleep Schedule: Inconsistent sleep patterns, such as frequent napping or irregular sleep and wake times, can disrupt the body’s natural sleep-wake cycle and lead to insomnia.
To manage insomnia and its potential impact on sleepwalking, it’s essential to address the underlying causes and develop healthy sleep habits. Here are some strategies that can promote better sleep:
– Establish a Regular Sleep Routine: Set a consistent sleep schedule, going to bed and waking up at the same time each day, even on weekends.
– Create a Calm and Comfortable Sleep Environment: Ensure that the bedroom is quiet, dark, and at a comfortable temperature. Consider using earplugs, eye masks, or white noise machines if necessary.
– Practice Relaxation Techniques: Engage in relaxation techniques before bed, such as deep breathing exercises, meditation, or taking a warm bath, to help calm the mind and prepare for sleep.
– Avoid Stimulants: Limit the consumption of caffeine, nicotine, and alcohol, as they can interfere with sleep quality and contribute to insomnia.
– Manage Stress: Find healthy ways to cope with stress and anxiety, such as through exercise, journaling, or talking to a therapist.
If insomnia persists or significantly impacts daily functioning, it is important to consult with a healthcare professional for a comprehensive evaluation and potential treatment options. By addressing insomnia, individuals may also find improvements in their sleepwalking episodes, creating the opportunity for restful and uninterrupted nights.
Treatment Options for Sleepwalking and Associated Sleep Disorders
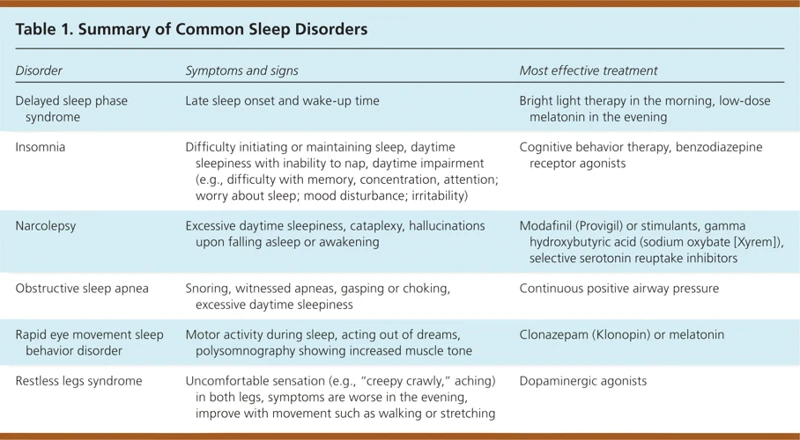
Treatment options for sleepwalking and associated sleep disorders aim to reduce the frequency and intensity of sleepwalking episodes, improve sleep quality, and minimize any potential risks or injuries during these events. While there is no one-size-fits-all approach, several strategies have shown promise in managing sleepwalking and the underlying sleep disorders.
Better sleep hygiene practices can be beneficial for individuals with sleepwalking and associated sleep disorders. This includes establishing a consistent sleep schedule, ensuring a comfortable sleep environment, and practicing relaxation techniques before bed. Avoiding stimulating activities, caffeine, and heavy meals close to bedtime can also contribute to better sleep quality and reduce the likelihood of sleepwalking episodes.
Medication may be prescribed in some cases to help manage sleepwalking. The specific medications used can vary depending on the individual’s symptoms and underlying conditions. Doctors may prescribe sedatives, such as benzodiazepines, to promote deeper sleep and reduce the occurrence of sleepwalking. However, it’s important to note that medication should be used under the guidance of a healthcare professional and its potential benefits should be weighed against any potential side effects.
Therapies and counseling can play a crucial role in managing sleepwalking and associated sleep disorders. Cognitive-behavioral therapy (CBT) can help identify and address any underlying triggers or psychological factors contributing to sleep disturbances. CBT techniques, such as relaxation exercises and stress management strategies, can promote healthier sleep patterns and reduce the frequency of sleepwalking episodes. In some cases, therapy may also involve addressing any trauma or emotional issues that may be disrupting sleep.
For individuals with comorbid sleep disorders, such as insomnia or sleep apnea, effectively treating the underlying condition can help alleviate sleepwalking episodes. This may involve using continuous positive airway pressure (CPAP) therapy for sleep apnea or exploring treatment options for insomnia, such as sleep hygiene practices or cognitive-behavioral therapy for insomnia (CBT-I).
It’s crucial to consult with a healthcare professional to determine the most appropriate treatment approach for sleepwalking and associated sleep disorders. They can assess the individual’s specific symptoms, medical history, and any underlying conditions to develop a personalized treatment plan that addresses their unique needs and goals. Effective treatment can significantly improve sleep quality and overall well-being for those affected by sleepwalking and associated sleep disorders.
Better Sleep Hygiene Practices
Better sleep hygiene practices play a crucial role in managing sleepwalking and improving overall sleep quality. By adopting healthy sleep habits, individuals can reduce the frequency and severity of sleepwalking episodes. Here are some tips to enhance sleep hygiene:
1. Maintain a Consistent Sleep Schedule: Establish a regular sleep routine by going to bed and waking up at the same time each day, including weekends. This helps regulate the body’s internal clock and promotes better sleep.
2. Create a Relaxing Bedtime Routine: Engage in calming activities before bed, such as reading a book, taking a warm bath, or practicing relaxation techniques like deep breathing or meditation. These rituals signal to the body that it’s time to unwind and prepare for sleep.
3. Create a Comfortable Sleep Environment: Make sure your bedroom is dark, quiet, and cool. Invest in a comfortable mattress and pillows that support a good sleeping posture. Use earplugs, white noise machines, or sleep masks if necessary to block out any disruptions.
4. Avoid Stimulants: Limit the consumption of caffeine, nicotine, and alcohol, especially in the evening. These substances can interfere with sleep patterns and exacerbate sleepwalking episodes.
5. Exercise Regularly: Engage in regular physical activity during the day, but avoid intense exercise close to bedtime. Regular exercise helps regulate sleep patterns and promotes overall well-being.
6. Create a Wind-Down Period: Allow yourself some time to wind down and relax before bed. Avoid engaging in stimulating activities or using electronic devices with blue light, as they can interfere with the body’s natural sleep-wake cycle.
7. Keep a Sleep Diary: Track your sleep patterns and any possible triggers for sleepwalking episodes. This can help identify patterns or factors that may contribute to the condition and guide treatment options.
By incorporating these sleep hygiene practices into your daily routine, you can create an optimal sleep environment and potentially reduce the occurrence of sleepwalking episodes. It is important to remember that consistent and personalized approaches may be needed, and consulting with a healthcare professional or sleep specialist can provide further guidance and support in managing sleepwalking.
Medication
can be an option for treating sleepwalking, especially if the episodes are frequent or cause significant disruption to daily life. However, it is important to note that medication is not always necessary or recommended for everyone with sleepwalking. The decision to use medication should be made in consultation with a healthcare professional who specializes in sleep disorders.
One commonly prescribed group of medications for sleepwalking is benzodiazepines. These medications, such as diazepam or clonazepam, work by suppressing the central nervous system, reducing brain activity, and promoting a more relaxed state. They can help decrease the frequency and intensity of sleepwalking episodes. However, benzodiazepines should be used with caution as they can be habit-forming and may cause side effects such as drowsiness, dizziness, and imbalance.
Another medication option is selective serotonin reuptake inhibitors (SSRIs). These medications, commonly used for treating depression and anxiety, have been found to be effective in reducing sleepwalking episodes in some individuals. SSRIs work by increasing the levels of serotonin in the brain, which helps regulate sleep patterns. However, they may also have side effects, such as nausea, headaches, and sexual dysfunction.
For individuals with underlying sleep disorders that contribute to sleepwalking, addressing the underlying condition may be the key to reducing episodes. For example, if sleep apnea is causing fragmented sleep and triggering sleepwalking, treating the sleep apnea with continuous positive airway pressure (CPAP) therapy may effectively reduce sleepwalking episodes.
It is important to stress that medication should always be used under the guidance and supervision of a healthcare professional. They can best assess the individual’s specific needs, evaluate the potential risks and benefits of medication, and determine the most appropriate course of treatment.
In addition to medication, various therapies and counseling techniques can also be beneficial for individuals with sleepwalking. These approaches may include cognitive-behavioral therapy (CBT), relaxation techniques, and sleep hygiene education. The combination of medication and therapy can provide comprehensive and individualized care for managing sleepwalking and improving overall sleep quality.
Therapies and Counseling
Therapies and counseling can be valuable approaches in managing sleepwalking and associated sleep disorders. When sleepwalking becomes frequent or poses a risk to the individual or others, seeking professional help is essential. Here are some therapeutic options to consider:
1. Cognitive Behavioral Therapy (CBT): This type of therapy focuses on identifying and modifying negative thought patterns and behaviors that may contribute to sleepwalking. CBT for sleepwalking may include techniques such as relaxation exercises, stress reduction strategies, and improving sleep hygiene practices.
2. Hypnosis: Hypnotherapy can be used to access the subconscious mind and introduce positive suggestions to prevent or reduce sleepwalking episodes. During hypnosis sessions, a trained therapist can help individuals explore the underlying causes of their sleepwalking and work on altering behavior patterns.
3. Biofeedback: Biofeedback techniques can provide individuals with real-time information about their physiological responses during sleep. This information helps individuals become more aware of the early signs of sleepwalking, allowing them to implement techniques to prevent or interrupt episodes when they occur.
4. Family Therapy: Sleepwalking affects not only the individual experiencing it but also their family members or roommates. Family therapy can help educate loved ones about sleepwalking and provide support, reducing anxiety and creating a more understanding and safe environment.
It’s important to remember that therapies and counseling should be tailored to an individual’s specific needs and preferences. Seeking guidance from a sleep specialist or mental health professional is crucial to determine the most appropriate therapeutic approach.
In addition to therapy, implementing lifestyle changes and maintaining good sleep hygiene practices can be beneficial in managing sleepwalking. This may include maintaining a regular sleep schedule, creating a conducive sleep environment, and avoiding known triggers or factors that disrupt sleep.
By combining therapies, counseling, and lifestyle modifications, individuals with sleepwalking and associated sleep disorders can improve their overall sleep quality and reduce the frequency and intensity of sleepwalking episodes. It’s crucial to work closely with healthcare professionals to find the most effective management plan based on individual circumstances and needs.
Preventing Sleepwalking Episodes
Taking steps to prevent sleepwalking episodes can help reduce the frequency and intensity of these events. By creating a safe sleeping environment and implementing stress reduction techniques, individuals can improve their quality of sleep and minimize the occurrence of sleepwalking.
Creating a Safe Sleeping Environment:
– Remove any potential hazards or obstacles from the sleepwalker’s bedroom, such as sharp objects, furniture with sharp edges, or cluttered pathways that could lead to injuries.
– Install safety gates at the top of stairs or other areas where the sleepwalker may be at risk of falling.
– Close and lock windows and doors to prevent the sleepwalker from wandering outside or accessing dangerous areas.
– Use alarms or motion sensor devices that can alert family members or caregivers if the sleepwalker leaves their bed or room during the night.
Stress Reduction Techniques:
– Establish a consistent bedtime routine that promotes relaxation and helps calm the mind before sleep. This can include activities such as taking a warm bath, practicing deep breathing exercises, or engaging in gentle stretching.
– Create a soothing sleep environment by keeping the bedroom dark, quiet, and at a comfortable temperature.
– Avoid stimulating activities or substances close to bedtime, such as caffeine, heavy meals, or electronic devices, as these can interfere with sleep quality.
– Practice stress management techniques during the day, such as regular exercise, meditation, or talking to a therapist or counselor if stress or anxiety is a contributing factor to sleepwalking episodes.
It’s important to note that while these prevention strategies can be helpful, they may not eliminate sleepwalking entirely, especially if there are underlying medical or psychological conditions involved. Consulting with a sleep specialist or healthcare provider is recommended for individuals who experience frequent or disruptive sleepwalking episodes. They can provide further guidance and tailor a treatment plan based on individual needs.
Creating a Safe Sleeping Environment
Creating a safe sleeping environment is crucial for individuals who experience sleepwalking episodes. By implementing certain measures, the risk of injuries or accidents can be significantly reduced. Here are some tips for creating a safe sleeping environment:
1. Remove obstacles: Clear the sleeping area of any potential hazards or obstacles that could cause a sleepwalker to trip or fall. This includes furniture with sharp corners, toys, clutter, or any items that may obstruct their path.
2. Secure windows and doors: Make sure all windows and doors are securely locked to prevent a sleepwalker from wandering outside and encountering potential dangers.
3. Install safety gates: If sleepwalking is a recurring issue, consider installing safety gates at the top and bottom of staircases to prevent falls.
4. Use nightlights: Keep the sleepwalker’s path well-lit during the night. Nightlights can help them navigate their surroundings safely, reducing the risk of accidents.
5. Avoid sleep on elevated surfaces: If possible, it’s best to discourage sleepwalkers from sleeping on elevated surfaces such as bunk beds or high-lofted beds. This can prevent falls during sleepwalking episodes.
6. Lock dangerous items: Keep potentially harmful items, such as sharp objects, medications, or cleaning supplies, securely locked away to ensure the sleepwalker’s safety.
7. Consider motion sensors: Motion-activated alarms or sensors placed near doors or windows can alert family members when a sleepwalker is on the move, allowing them to intervene and guide the sleepwalker back to bed.
In addition to these specific measures, it is also important to communicate with family members: Inform everyone in the household about the sleepwalker’s condition and provide instructions on how to respond if a sleepwalking episode occurs. This can ensure a quick and supportive response to keep the sleepwalker safe.
By taking these precautions and creating a safe sleeping environment, the risk of accidents and injuries associated with sleepwalking can be minimized, allowing both the sleepwalker and their loved ones to have peace of mind.
Stress Reduction Techniques
Managing stress is crucial for individuals who experience sleepwalking episodes. Implementing stress reduction techniques can help reduce the frequency and severity of sleepwalking episodes. Mindfulness meditation is one effective technique that promotes relaxation and calmness. By focusing on the present moment and practicing deep breathing exercises, individuals can reduce stress levels and improve overall sleep quality.
Another effective stress reduction technique is progressive muscle relaxation. This practice involves tensing and then relaxing different muscle groups throughout the body, releasing built-up tension and promoting a sense of relaxation. Engaging in regular physical exercise is also beneficial for stress reduction, as it helps release endorphins and reduces anxiety.
Creating a consistent sleep schedule is essential for stress reduction and better sleep. Going to bed and waking up at the same time every day can help regulate the sleep-wake cycle and promote more restful sleep. Avoiding caffeine, alcohol, and nicotine close to bedtime is important, as these substances can interfere with sleep quality and increase stress levels.
Incorporating relaxation techniques before bedtime can also be helpful. This can include activities such as taking a warm bath, practicing yoga or stretching exercises, reading a book, or listening to calming music. It is important to create a calming and soothing environment in the bedroom to promote relaxation and minimize stress.
Finally, seeking professional help from a therapist or counselor can provide individuals with effective coping mechanisms to manage stress and anxiety. Cognitive-behavioral therapy (CBT) is often used to address stress-related issues and can help individuals develop healthier ways of coping with stress and reduce the likelihood of sleepwalking episodes.
Implementing stress reduction techniques can significantly improve overall sleep quality and reduce the frequency of sleepwalking episodes. However, it is important to remember that each individual may respond differently to various techniques, so it may be necessary to try different strategies to find what works best for each person. Taking steps to reduce stress and promote relaxation can contribute to better sleep and a reduction in sleepwalking episodes.
Conclusion
In conclusion, sleepwalking is a fascinating and complex sleep disorder that involves performing behaviors and activities during deep non-REM sleep. It can be a bewildering experience for both the sleepwalker and those around them. While the exact causes of sleepwalking are not fully understood, various factors such as genetic predisposition, stress, sleep deprivation, and environmental factors contribute to its occurrence.
Sleepwalking is not just an isolated phenomenon but is also related to other sleep disorders. It shares similarities with night terrors, as both involve partial arousal from deep sleep and can result in complex behaviors. Additionally, a similar phenomenon called REM Sleep Behavior Disorder (RBD) involves acting out dreams during REM sleep, and there may be an overlap between sleepwalking and RBD. Sleepwalking can also be associated with insomnia, as sleep disturbances can trigger sleepwalking episodes.
Fortunately, there are treatment options available for sleepwalking and associated sleep disorders. Improving sleep hygiene practices such as maintaining a regular sleep schedule, creating a relaxing bedtime routine, and ensuring a comfortable sleep environment can help reduce the frequency of sleepwalking episodes. In some cases, medications may be prescribed that can help regulate sleep patterns. Therapies such as cognitive-behavioral therapy (CBT) and counseling can also assist in managing sleepwalking and addressing any underlying psychological factors.
To prevent sleepwalking episodes, it is crucial to create a safe sleeping environment by removing any obstacles or hazards that could potentially cause injury. Implementing stress reduction techniques such as relaxation exercises, meditation, or therapy can also aid in minimizing sleep disturbances and reducing the likelihood of sleepwalking.
In conclusion, while sleepwalking remains a fascinating and somewhat enigmatic sleep disorder, understanding its definition, causes, symptoms, and relationship with other sleep disorders can provide valuable insights into its nature and treatment options. By employing appropriate interventions and strategies, individuals who experience sleepwalking can take steps towards better sleep and improved overall well-being.
Frequently Asked Questions
FAQ 1: Can sleepwalking be dangerous?
Yes, sleepwalking can potentially be dangerous. Sleepwalkers can unknowingly engage in activities that may lead to physical injury, such as falling down stairs or accidentally harming themselves or others in their path.
FAQ 2: Is sleepwalking a common sleep disorder?
Yes, sleepwalking is relatively common, especially in children. It is estimated to affect around 10-15% of children and about 2-4% of adults.
FAQ 3: Can sleepwalking be hereditary?
Yes, there is evidence to suggest that sleepwalking can have a genetic component. If one or both parents have a history of sleepwalking, their children are more likely to experience it as well.
FAQ 4: Can stress trigger sleepwalking episodes?
Yes, stress and anxiety can be triggers for sleepwalking. Emotional distress and feelings of anxiety can disrupt normal sleep patterns and increase the likelihood of sleepwalking episodes.
FAQ 5: Should I wake up a sleepwalker?
It is generally recommended not to wake up a sleepwalker abruptly. Instead, gently guide them back to bed to minimize the risk of disorientation or confusion.
FAQ 6: Can medications cause sleepwalking?
Yes, certain medications, such as sedatives, hypnotics, and some antidepressants, have been associated with an increased risk of sleepwalking. It is important to discuss any concerns with a healthcare professional if you suspect your medication may be contributing to sleepwalking episodes.
FAQ 7: Can sleepwalking occur during naps?
Yes, sleepwalking can occur during both nighttime sleep and daytime naps, as long as the individual reaches the deep non-REM sleep stages where sleepwalking is more likely to happen.
FAQ 8: Can sleepwalking be a symptom of another sleep disorder?
Yes, sleepwalking can be associated with other sleep disorders, such as sleep apnea, restless leg syndrome, or insomnia. Treating the underlying sleep disorder may help reduce sleepwalking episodes.
FAQ 9: Can alcohol and drug use contribute to sleepwalking?
Yes, alcohol and certain drugs can increase the likelihood of sleepwalking. They can disrupt normal sleep patterns and interfere with the brain’s ability to regulate sleep stages effectively.
FAQ 10: Can sleepwalking be treated effectively?
Yes, sleepwalking can often be managed and controlled through various treatment strategies, including improving sleep hygiene, medication, and therapy. It is best to consult with a healthcare professional to determine the most suitable treatment approach.