Have you ever wondered what happens to your brain while you’re sleepwalking? Sleepwalking, also known as somnambulism, is a fascinating phenomenon that occurs during certain stages of sleep. It involves a series of complex behaviors that are carried out while an individual is still asleep, leaving them with little to no memory of their nocturnal adventures. It’s a puzzling condition that raises questions about the intricate workings of the brain during sleep and how it can affect our cognitive functioning. In this article, we will dive into the world of sleepwalking and unveil the impact it has on the brain, exploring the stages of sleep, the brain’s role in sleep, abnormal activation patterns, neurotransmitter imbalances, and the influence of sleep disorders. Additionally, we will discuss the cognitive effects of sleepwalking, potential triggers, and strategies for prevention and treatment.
What is Sleepwalking?

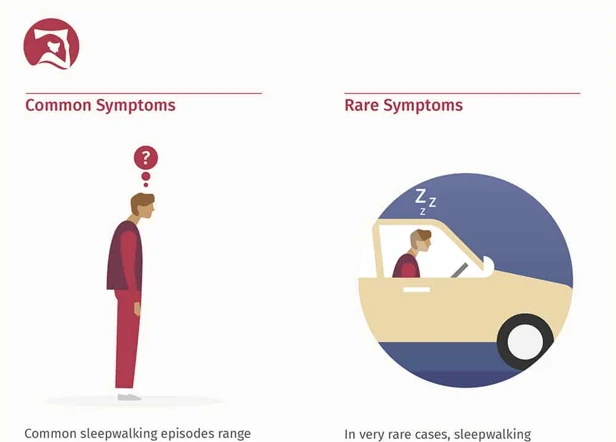
Sleepwalking, also known as somnambulism, is a sleep disorder characterized by complex behaviors and actions that are performed during sleep. It typically occurs during the deeper stages of sleep, particularly during non-rapid eye movement (NREM) sleep. People who experience sleepwalking may engage in a variety of activities, such as walking, talking, eating, or even driving, all while remaining in a sleep state. Sleepwalkers often have little to no memory of their actions once they wake up. While the exact causes of sleepwalking are not fully understood, it is believed to involve a combination of genetic predisposition and environmental factors. To learn more about the causes of sleepwalking, you can read our article Understanding the Causes of Sleepwalking. Sleepwalking can be a perplexing and sometimes even dangerous condition, but advancements in scientific understanding are shedding light on the science behind sleepwalking. If you want to delve deeper into the topic, you may be interested in our article The Science Behind Sleepwalking Explained. Throughout history, there have been fascinating and famous cases of sleepwalking, such as that of the famous explorer Christopher Columbus. To dive into some intriguing sleepwalking stories from the past, check out our article Famous Sleepwalking Cases in History.
The Stages of Sleep
The stages of sleep play a crucial role in understanding sleepwalking and its impact on the brain. Sleep can be divided into two main categories: non-rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep. NREM sleep is further categorized into three stages: N1, N2, and N3.
- N1: This is the stage between wakefulness and sleep. It is a light sleep stage where the muscles start to relax, and the brain produces alpha and theta waves. During this stage, it is easy for individuals to be aroused.
- N2: This is a slightly deeper stage of sleep. The brain produces bursts of rapid brain wave activity called sleep spindles and K-complexes. The body temperature starts to drop, and the heart rate and breathing become regular.
- N3: Also known as deep or slow-wave sleep, N3 is the stage where the body and brain undergo significant restoration. This is the stage where sleepwalking is most likely to occur. The brain produces slow delta waves, and it’s difficult to awaken someone in this stage. Sleepwalking episodes are more common during the first half of the night when NREM sleep is at its peak.
REM sleep, on the other hand, is characterized by rapid eye movements, increased brain activity, and vivid dreaming. REM sleep typically occurs in cycles throughout the night, with each cycle lasting about 90-120 minutes. Interestingly, sleepwalking episodes are rare during REM sleep since the body is in a state of temporary paralysis, known as REM atonia, to prevent individuals from acting out their dreams.
NREM and REM Sleep
When it comes to understanding sleepwalking and its effects on the brain, it’s essential to explore the different stages of sleep, particularly non-rapid eye movement (NREM) and rapid eye movement (REM) sleep. NREM sleep is divided into four distinct stages, each characterized by specific brain wave patterns and physiological changes. During NREM sleep, our brain activity slows down, and our body enters a state of deep relaxation. This is the stage where sleepwalking is most likely to occur. REM sleep is the stage where we experience vivid dreams and increased brain activity, similar to when we are awake. However, sleepwalking mainly occurs during NREM sleep, when our brain is in a state of relative quiet and our body is in a low-arousal state. To better understand the stages of sleep and their impact on sleepwalking, we can use a table to summarize their characteristics:
| Stage | Description |
|---|---|
| NREM Stage 1 | Transition between wakefulness and sleep; light sleep |
| NREM Stage 2 | Deeper sleep; body temperature and heart rate decrease |
| NREM Stage 3 | Deepest sleep; difficult to awaken; crucial for physical restoration and growth |
| NREM Stage 4 | Also known as slow-wave sleep (SWS); essential for memory consolidation and learning |
| REM Sleep | Characterized by rapid eye movements and intense brain activity; vivid dreaming occurs |
As sleepwalking usually occurs during NREM sleep, particularly in the deeper stages, it suggests that certain aspects of this type of sleep may contribute to the manifestation of sleepwalking behaviors. The intricate interplay between NREM and REM sleep and the brain’s activity during these stages hold valuable insights into the mechanisms underlying sleepwalking.
The Role of the Brain in Sleep
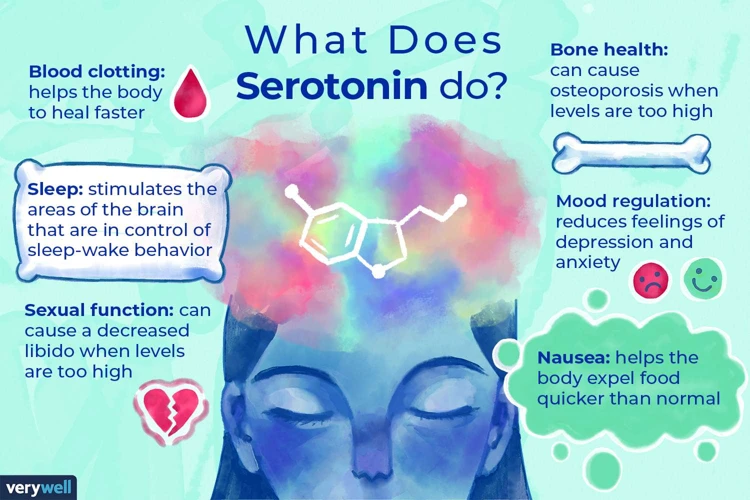
In order to understand how sleepwalking affects the brain, it’s important to first explore the role of the brain in sleep. Sleep is a complex process that involves different stages, each with distinct brain activity patterns. The two main stages of sleep are non-rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep. During NREM sleep, the brain transitions through multiple stages, from light sleep to deep sleep. This is the stage where sleepwalking is most likely to occur. REM sleep, on the other hand, is associated with vivid dreaming and increased brain activity. The brain plays a crucial role in regulating and maintaining these sleep stages. Different areas of the brain are involved in controlling sleep-wake cycles, including the hypothalamus, which produces hormones like melatonin that regulate sleep, and the brainstem, which plays a role in controlling muscle tone during sleep. The brain also produces certain neurotransmitters, such as serotonin and dopamine, that affect sleep and wakefulness. By understanding the intricate workings of the brain during sleep, we can begin to comprehend how sleepwalking disrupts these processes and affects cognitive functioning.
The Brain during Sleepwalking
When it comes to sleepwalking, the brain plays a central role in orchestrating this complex behavior. Research has shown that the brain exhibits abnormal activation patterns during sleepwalking episodes. Electroencephalograms (EEGs), which measure brain activity, have revealed that sleepwalkers display a mix of both wakefulness and deep sleep patterns. This suggests that the brain is caught in a state of imbalance, unable to fully switch between sleep stages. Additionally, there is evidence of neurotransmitter imbalances during sleepwalking. Neurotransmitters such as gamma-aminobutyric acid (GABA) and dopamine, which are involved in regulating sleep and movement, may be disrupted in sleepwalkers. These imbalances could contribute to the motor activity and unusual behaviors exhibited during sleepwalking episodes. Understanding the intricate mechanisms at play in the brain during sleepwalking is still an area of ongoing research, but it sheds light on the complexity of this sleep disorder and its effects on the brain.
Abnormal Activation Patterns
One of the key factors that contribute to sleepwalking is abnormal brain activation patterns during sleep. Research has shown that individuals who sleepwalk exhibit different patterns of brain activity compared to those who do not sleepwalk. Specifically, there is an increased activation in certain areas of the brain during sleep, particularly in the motor cortex and the areas involved in movement control. This abnormal activation can lead to the execution of complex motor behaviors during sleep, such as walking or talking. Additionally, studies using imaging techniques such as functional magnetic resonance imaging (fMRI) have revealed that there is decreased connectivity between different regions of the brain in sleepwalkers. This disrupted connectivity may contribute to the disconnect between the sleepwalker’s actions and their conscious awareness of their surroundings. It’s important to note that the exact mechanisms underlying these abnormal activation patterns are still being investigated, and there is much more to learn about the intricate workings of the brain during sleepwalking.
Neurotransmitter Imbalances
Neurotransmitter imbalances play a significant role in sleepwalking. These imbalances occur when there is a disruption or dysregulation in the levels of certain chemical messengers in the brain. Two key neurotransmitters implicated in sleepwalking are gamma-aminobutyric acid (GABA) and dopamine. GABA is an inhibitory neurotransmitter that helps regulate brain activity and promotes relaxation. Studies have suggested that decreased GABA activity during sleep can contribute to the occurrence of sleepwalking episodes. On the other hand, dopamine is an excitatory neurotransmitter associated with arousal and motor functions. Imbalances in dopamine levels have been linked to increased motor activity during sleep and may contribute to the physical manifestations of sleepwalking.
To give you a clearer understanding, let’s break it down further:
– GABA imbalances: A decrease in GABA levels may result in reduced inhibitory control, leading to overactivation of certain brain regions and subsequent sleepwalking behavior.
– Dopamine imbalances: An increase in dopamine levels can heighten arousal and motor activity during sleep, potentially triggering sleepwalking episodes.
It’s important to note that neurotransmitter imbalances alone may not fully explain the occurrence of sleepwalking, as this condition is likely influenced by a combination of genetic and environmental factors. By gaining insights into these imbalances, researchers hope to develop a better understanding of the mechanisms behind sleepwalking and explore potential treatment options.
Sleep Disorders and Sleepwalking

Sleep disorders can have a significant impact on sleepwalking, as they can disrupt the normal sleep patterns and increase the likelihood of sleepwalking episodes. One common sleep disorder that is closely associated with sleepwalking is insomnia. Insomnia is characterized by difficulty falling asleep or staying asleep, leading to poor sleep quality and insufficient rest. Individuals with insomnia often experience fragmented sleep, which can trigger sleepwalking episodes during the night. To learn more about the relationship between sleepwalking and insomnia, you can refer to our article on Sleepwalking and Insomnia.
Another sleep disorder that can contribute to sleepwalking is sleep apnea. Sleep apnea is a condition where the individual’s breathing is repeatedly interrupted during sleep, causing them to briefly wake up multiple times throughout the night. These awakenings can disrupt the sleep cycle and increase the likelihood of sleepwalking episodes. The connection between sleep apnea and sleepwalking is still being studied, but evidence suggests that the oxygen deprivation and fragmented sleep associated with sleep apnea may trigger sleepwalking behaviors. If you want to explore the relationship between sleep apnea and sleepwalking in more detail, you can read our article on Sleepwalking and Sleep Apnea.
Sleepwalking and Insomnia
Sleepwalking and insomnia are two sleep disorders that can sometimes coexist or be interconnected. Insomnia refers to difficulties falling asleep, staying asleep, or experiencing poor-quality sleep. Sleepwalking, on the other hand, involves engaging in complex behaviors during sleep, typically during the deeper stages of sleep. While insomnia and sleepwalking are distinct disorders, there can be a relationship between the two. Insomnia can increase the likelihood of sleepwalking episodes, as disrupted or inadequate sleep can disrupt the normal sleep-wake cycle and increase the risk of sleepwalking. Conversely, sleepwalking can also contribute to insomnia. Sleepwalkers may experience disturbed sleep patterns due to their nocturnal activities, leading to fragmented and insufficient sleep, which can further exacerbate insomnia symptoms. Understanding the relationship between sleepwalking and insomnia is essential for developing effective treatment strategies that address both conditions simultaneously. If you are interested in exploring more about insomnia and its impact on sleepwalking, check out our comprehensive guide to insomnia, which can be found here.
Sleepwalking and Sleep Apnea
Sleepwalking and sleep apnea are two sleep disorders that can often coexist and have significant impacts on an individual’s sleep quality and overall well-being. Sleep apnea is a condition characterized by pauses in breathing during sleep, leading to disrupted sleep patterns and decreased oxygen levels in the blood. It is believed that the disruptions in sleep caused by sleep apnea can trigger episodes of sleepwalking in susceptible individuals. Research has shown a strong association between sleep apnea and sleepwalking, with studies indicating that up to 13% of individuals with sleep apnea also experience sleepwalking. The exact mechanism behind this relationship is not fully understood, but it is thought to involve abnormalities in the brain’s arousal systems. Sleep apnea can lead to fragmented and poor-quality sleep, which may increase the likelihood of sleepwalking episodes. Additionally, the sleep deprivation and fatigue caused by sleep apnea can further impair cognitive function and increase the risk of accidents during sleepwalking episodes. If you suspect that you or someone you know may have both sleep apnea and sleepwalking, it is important to seek medical evaluation and treatment. Managing sleep apnea through interventions such as continuous positive airway pressure (CPAP) therapy can help improve sleep quality and reduce the frequency of sleepwalking episodes. Understanding the relationship between these two sleep disorders can aid in the development of comprehensive treatment plans that address both conditions simultaneously.
Impact on Cognitive Function
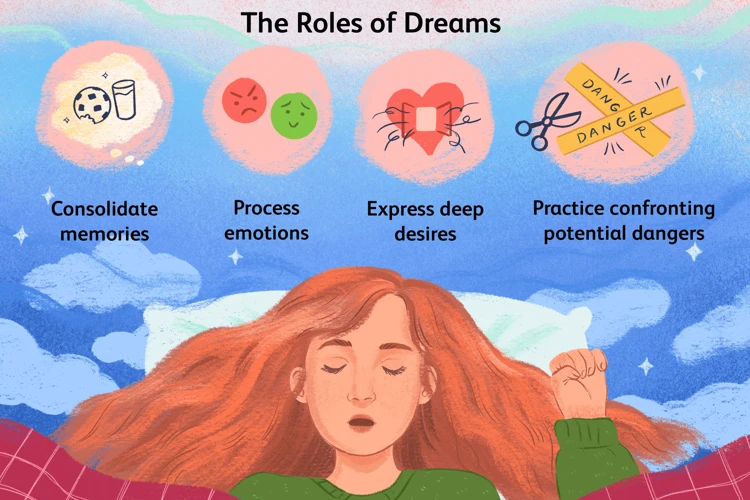
The impact of sleepwalking on cognitive function is a significant aspect of this sleep disorder. Sleepwalking can have various effects on cognitive abilities, including memory consolidation disturbances and impaired decision-making abilities. One of the ways sleepwalking affects cognitive function is through disturbances in memory consolidation. During sleep, our brains process and consolidate memories, transferring them from short-term memory to long-term memory. However, sleepwalking can disrupt this process, leading to fragmented or incomplete memories of events that occurred during the sleepwalking episode. Individuals may wake up with a sense of confusion or disorientation, unable to recall specific details of their sleepwalking experience.
In addition to memory disturbances, sleepwalking can also impair decision-making abilities. As sleepwalkers engage in complex behaviors while still in a sleep state, their decision-making processes are likely to be compromised. Sleepwalkers may engage in actions or behaviors that they would not normally do while awake, leading to potential risks and safety concerns. For instance, they may attempt to cook or use sharp objects without being fully aware of the associated dangers.
It is important to note that the impact on cognitive function can vary among individuals who experience sleepwalking. While some individuals may have minimal cognitive impairment, others may experience more significant disruptions. Factors such as the frequency and duration of sleepwalking episodes may also influence the extent of cognitive effects.
Understanding the impact of sleepwalking on cognitive function is essential for both individuals who sleepwalk and their loved ones. By recognizing the potential cognitive challenges associated with sleepwalking, appropriate precautions and support can be put in place to ensure safety and well-being.
Memory Consolidation Disturbances
Memory consolidation disturbances are one of the ways in which sleepwalking can affect cognitive functioning. During sleep, our brains have the important task of consolidating and storing memories from the day’s experiences. However, in individuals who sleepwalk, this process can be disrupted. Studies have shown that sleepwalkers may have difficulties with memory consolidation, leading to fragmented or incomplete memories of their waking lives. This can result in difficulties with recalling events, learning new information, and forming long-term memories. Additionally, the disrupted sleep patterns associated with sleepwalking can further impair memory consolidation. The exact mechanisms behind these memory disturbances are not fully understood, but researchers believe that abnormalities in the brain’s electrical activity during sleep may play a role. To learn more about the potential causes and impact of sleepwalking on memory consolidation, you can explore scientific studies and articles in the field.
Impaired Decision-making Abilities
One of the cognitive functions that can be affected by sleepwalking is decision-making abilities. When individuals sleepwalk, their brains are essentially operating in a state between sleep and wakefulness, which can lead to impaired decision-making skills. Sleepwalking can cause individuals to make irrational or risky decisions that they would not make when fully awake. This impairment is believed to be due to a disruption in the brain’s executive functions, which are responsible for logical reasoning, judgment, and self-control. Sleepwalking can also affect the brain’s ability to accurately assess risks and consequences, leading to potentially dangerous situations. For example, a sleepwalker may engage in activities like cooking or driving without full awareness or consideration of the associated risks. This impaired decision-making can increase the likelihood of accidents or injuries during sleepwalking episodes. It is crucial for individuals who sleepwalk to take precautions to ensure their safety and the safety of those around them. Creating a sleep-friendly environment, implementing safety measures, and seeking appropriate treatment can help manage impaired decision-making abilities associated with sleepwalking.
Understanding Sleepwalking Triggers

Understanding the triggers of sleepwalking is essential in managing and preventing episodes. Sleepwalking can be caused by a variety of factors, including genetic predisposition and environmental influences. Firstly, genetic predisposition plays a significant role in determining an individual’s susceptibility to sleepwalking. Studies have shown that sleepwalking tends to run in families, suggesting a genetic component to the condition. Additionally, certain environmental factors can act as triggers for sleepwalking. These factors include sleep deprivation, irregular sleep schedules, stress, anxiety, and certain medications. It is important to create a sleep-friendly environment by ensuring a regular sleep schedule, maintaining a relaxing bedtime routine, and minimizing stress levels. By addressing these triggers, sleepwalkers may be able to reduce the frequency and severity of their sleepwalking episodes. To learn more about sleepwalking triggers, you can refer to our informative article that explores this topic in depth.
Genetic Predisposition
Genetic predisposition plays a significant role in sleepwalking, as studies have shown that sleepwalking tends to run in families. It is believed that certain genetic variations can make individuals more susceptible to this sleep disorder. One particular study conducted by researchers at Stanford University identified a gene called CHRNA2 that is associated with an increased risk of sleepwalking. This gene is involved in the regulation of neurotransmitters in the brain, specifically those related to the cholinergic system. Another gene that has been linked to sleepwalking is DEC2, which regulates the body’s circadian rhythm. Individuals with a mutation in this gene may experience disrupted sleep patterns, including sleepwalking episodes. Although genetic predisposition is a significant factor, it does not guarantee that a person will sleepwalk. Environmental factors, such as stress, sleep deprivation, and certain medications, can also trigger sleepwalking episodes in genetically predisposed individuals. To understand the complexities of genetic factors and sleepwalking in more detail, you can refer to relevant scientific research studies and publications.
Environmental Factors
Environmental factors play a significant role in sleepwalking. Certain external circumstances can trigger or exacerbate episodes of sleepwalking. One such factor is insufficient or poor quality sleep. Sleep deprivation can disrupt the normal sleep cycle, increasing the likelihood of sleepwalking episodes. Additionally, environmental disturbances such as noise, light, or extreme temperatures can contribute to sleepwalking. For example, sleeping in a noisy environment can disrupt the deep sleep stages where sleepwalking is more likely to occur. Stress and anxiety are also environmental factors that can influence sleepwalking. High levels of stress can disrupt sleep patterns and increase the frequency of sleepwalking episodes. It is important to create a calm and conducive sleep environment to minimize the risk of sleepwalking. Removing potential hazards in the sleep environment, such as sharp objects or obstacles in the bedroom, can also help prevent injuries during sleepwalking episodes. To learn more about sleepwalking triggers and how to handle them, check out our article Understanding Sleepwalking Triggers.
Prevention and Treatment Strategies
When it comes to sleepwalking, prevention and treatment strategies can play a crucial role in managing and reducing the frequency of sleepwalking episodes. The first step in preventing sleepwalking is to create a safe sleep environment. This includes removing any potential hazards or obstacles that a sleepwalker might encounter during their nocturnal wanderings. For example, securing windows and doors, clearing clutter from the bedroom, and using safety gates can all help create a safer sleep environment. Additionally, establishing a consistent sleep routine and ensuring that the sleepwalker gets enough quality sleep can also be beneficial. In some cases, treating any underlying sleep disorders, such as insomnia or sleep apnea, may help reduce sleepwalking episodes. Cognitive behavioral therapy (CBT) can also be an effective treatment approach for sleepwalking, as it helps address any underlying psychological factors that may contribute to the condition. In certain cases, medication may be prescribed to manage sleepwalking, but it is typically only used in severe or persistent cases. It is important to consult with a healthcare professional or sleep specialist for an accurate diagnosis and personalized treatment plan. By implementing these prevention and treatment strategies, individuals with sleepwalking can significantly improve their quality of sleep and reduce the impact of sleepwalking on their daily lives.
Conclusion
In conclusion, sleepwalking is a complex sleep disorder that involves a variety of behaviors and actions performed while an individual is in a sleep state. While the exact mechanisms behind sleepwalking are still not fully understood, research suggests that abnormal activation patterns and neurotransmitter imbalances in the brain may play a role in its occurrence. Sleepwalking can have a significant impact on cognitive function, including disturbances in memory consolidation and impaired decision-making abilities. Understanding the triggers for sleepwalking, such as genetic predisposition and environmental factors, can help individuals better manage and prevent episodes. Treatment strategies for sleepwalking may involve creating a safe sleep environment, managing underlying sleep disorders, and, in some cases, medication. Despite the challenges presented by sleepwalking, ongoing research and advancements in the field provide hope for better understanding and management of this intriguing phenomenon. Sleepwalking continues to fascinate scientists and individuals alike, highlighting the mysterious nature of our sleep and the intricate workings of the brain.
Frequently Asked Questions
1. What percentage of the population experiences sleepwalking?
Approximately 1-15% of the population experiences sleepwalking at some point in their lives.
2. At what age does sleepwalking typically start?
Sleepwalking often starts in childhood, usually between the ages of 4 and 8.
3. Is sleepwalking dangerous?
Sleepwalking can potentially be dangerous, as sleepwalkers may engage in activities that put themselves or others at risk. It is important to take precautions to ensure safety.
4. Can sleepwalking be triggered by stress?
Yes, stress can be a contributing factor in the occurrence of sleepwalking episodes. Managing stress levels may help reduce the frequency of sleepwalking incidents.
5. Can waking a sleepwalker cause harm?
Waking a sleepwalker is generally considered safe and necessary if they are in a potentially dangerous situation. However, it is important to gently guide them back to bed and ensure they are not startled.
6. Is it true that sleepwalkers’ eyes are open but they are not fully conscious?
Yes, sleepwalkers often have their eyes open, but their consciousness is in a state between sleep and wakefulness. They are not fully aware of their surroundings and may appear confused.
7. Can sleepwalking be inherited?
There is evidence to suggest that sleepwalking may have a genetic component, as it often runs in families. However, other factors, such as environmental triggers, may also play a role.
8. Can alcohol or sleep deprivation trigger sleepwalking?
Yes, both alcohol consumption and sleep deprivation can increase the likelihood of sleepwalking episodes. It is best to avoid these triggers if you are prone to sleepwalking.
9. Can medications cause sleepwalking?
Some medications, such as certain sleep aids, antidepressants, and antipsychotics, have been associated with sleepwalking as a potential side effect. It is important to discuss any concerns with a healthcare professional.
10. Is there a cure for sleepwalking?
While there is no specific cure for sleepwalking, certain strategies, such as improving sleep hygiene, managing stress, and creating a safe sleep environment, can help reduce the frequency and severity of sleepwalking episodes.