Are you or your child experiencing trouble with both sleep and bedwetting? Have you ever wondered if there could be a connection between these two issues? Break free from the endless cycle of uncertainty and explore the potential link between sleep disorders and bedwetting. In this article, we will delve into the science behind sleep disorders, gain a deeper understanding of bedwetting, and investigate the possible correlation between the two. Join us on this journey as we uncover the impact that sleep disorders can have on bedwetting and how bedwetting may contribute to sleep disturbances. Additionally, we will explore treatment and management options to help you or your loved ones find relief. Let’s discover the connection together.
Sleep Disorders and Bedwetting: Explained

Sleep Disorders and Bedwetting: Explained
Sleep disorders and bedwetting are two separate issues that can often coincide, causing significant disruptions in one’s sleep patterns and quality of life. Sleep disorders refer to a range of conditions that affect the ability to fall asleep, stay asleep, or achieve sufficient deep sleep. These disorders can manifest in various ways, such as insomnia, sleep apnea, restless leg syndrome, or narcolepsy.
Bedwetting, medically known as nocturnal enuresis, is the involuntary release of urine during sleep, often experienced by children but can also affect adults. This condition can lead to embarrassment, emotional distress, and disrupted sleep for both the individual and their family members.
While sleep disorders and bedwetting may seem unrelated, there is evidence to suggest a potential connection between the two. Sleep disorders can disrupt the normal sleep architecture, leading to fragmented or disrupted sleep patterns. This can make it difficult for individuals to wake up when their bladder is full, potentially contributing to bedwetting episodes.
Certain sleep disorders, such as sleep apnea, can cause increased pressure on the bladder during sleep, making accidents more likely to occur. Additionally, some studies suggest a possible link between the hormones involved in regulating sleep and those involved in controlling bladder function.
In the next sections, we will delve deeper into the science behind sleep disorders, explore the causes of bedwetting in both children and adults, and examine the potential impact that sleep disorders can have on bedwetting. Understanding this connection is crucial for developing effective treatment and management strategies. So, let’s continue our exploration to uncover the intricate relationship between sleep disorders and bedwetting.
The Science Behind Sleep Disorders
The Science Behind Sleep Disorders
Sleep disorders are a complex interplay of various factors that can disrupt the normal sleep-wake cycle. One commonly known sleep disorder is insomnia, characterized by difficulty falling asleep or staying asleep. Insomnia can be caused by factors such as stress, anxiety, or certain medical conditions. Another sleep disorder is sleep apnea, which occurs when the upper airway becomes partially or completely blocked during sleep, leading to pauses in breathing. Restless leg syndrome is another condition that causes uncomfortable sensations in the legs, often leading to an irresistible urge to move them, thereby interrupting sleep. Narcolepsy is a neurological disorder characterized by excessive daytime sleepiness and sudden sleep attacks. These sleep disorders can have detrimental effects on an individual’s physical and mental well-being, leading to daytime fatigue, poor concentration, mood disturbances, and a compromised quality of life. Understanding the science behind sleep disorders is essential to develop effective treatment strategies and promote restful sleep.
Common Sleep Disorders
Common Sleep Disorders
Sleep disorders encompass a wide range of conditions that can disrupt the normal sleep-wake cycle and affect overall sleep quality. Understanding these disorders is essential in recognizing their potential impact on bedwetting. Here are some of the most common sleep disorders:
1. Insomnia: Insomnia is characterized by difficulty falling asleep, staying asleep, or experiencing non-restorative sleep. It can be caused by various factors such as stress, anxiety, medications, or underlying medical conditions. Individuals with insomnia may find it challenging to achieve a deep sleep, which can potentially contribute to bedwetting.
2. Sleep Apnea: Sleep apnea is a disorder in which breathing repeatedly stops and starts during sleep. This interruption in breathing can lead to fragmented sleep and decreased oxygen flow to the body, resulting in daytime fatigue and increased pressure on the bladder. Sleep apnea can be associated with an increased risk of bedwetting episodes.
3. Restless Leg Syndrome (RLS): RLS is characterized by an irresistible urge to move the legs, often accompanied by uncomfortable sensations. These sensations are typically worse at night, leading to difficulty falling asleep or staying asleep. RLS can disrupt sleep patterns, potentially making it harder to wake up when the bladder is full.
4. Narcolepsy: Narcolepsy is a neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. Individuals with narcolepsy may experience excessive daytime sleepiness and sudden sleep attacks during the day. These unpredictable sleep episodes can disrupt nighttime sleep patterns and increase the likelihood of bedwetting.
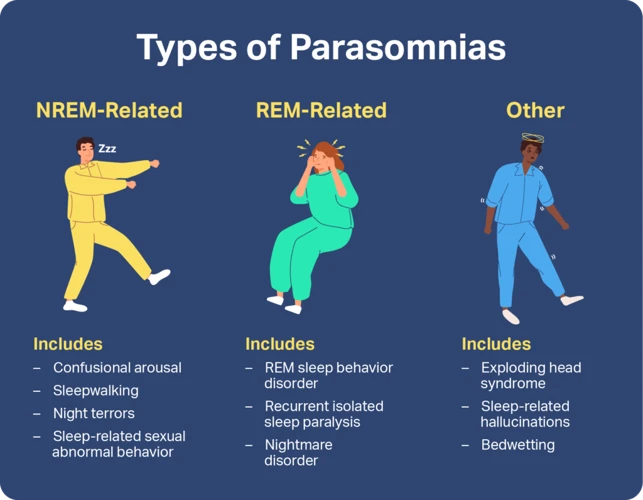
5. Parasomnias: Parasomnias are a group of sleep disorders that involve abnormal behaviors or movements during sleep. Examples include sleepwalking, night terrors, and sleep-related eating disorder. While not directly linked to bedwetting, parasomnias can disrupt sleep continuity and potentially contribute to the occurrence of bedwetting episodes.
It’s important to note that these are just a few examples of common sleep disorders and their potential connection to bedwetting. Proper diagnosis and treatment by healthcare professionals are crucial in addressing underlying sleep disorders and developing effective strategies to manage bedwetting. To learn more about how to address bedwetting, you can read our helpful guide by clicking this link: How to Address Bedwetting.
Effects of Sleep Disorders on the Body
Effects of Sleep Disorders on the Body
Sleep disorders can have a profound impact on various aspects of the body’s functioning. Here are some of the effects that sleep disorders can have:
1. Cognitive Function: Lack of quality sleep due to sleep disorders can impair cognitive function. This includes difficulties with concentration, memory, problem-solving, and decision-making. These cognitive impairments can affect daily activities, work performance, and academic success.
2. Emotional Well-being: Sleep disorders can contribute to mood disturbances, including increased irritability, mood swings, and a higher risk of developing anxiety and depression. Lack of sleep can also exacerbate existing mental health conditions.
3. Physical Health: Chronic sleep disorders have been linked to numerous physical health problems. These include increased risk of obesity, diabetes, cardiovascular diseases, hypertension, and weakened immune system functioning. Sleep deprivation can lead to higher levels of inflammation in the body, which is associated with various health issues.
4. Hormonal Imbalances: Sleep disorders can disrupt the delicate balance of hormones in the body. This can result in decreased production of growth hormones, increased levels of stress hormones like cortisol, and alterations in appetite-regulating hormones such as ghrelin and leptin. These hormonal imbalances can potentially lead to weight gain, reduced muscle mass, and increased appetite.
5. Decreased Libido: Sleep disorders can also contribute to a decreased sex drive and sexual dysfunction. Fatigue, low energy levels, and hormonal imbalances resulting from sleep disorders can all affect sexual health and function.
It’s important to recognize the wide-ranging impact that sleep disorders can have on the body. Seeking proper diagnosis and treatment is crucial not only for improving sleep but also for promoting overall health and well-being. In the next sections, we will further explore the possible connection between sleep disorders and bedwetting, shedding light on how these two issues may intersect.
Understanding Bedwetting

Bedwetting, also known as nocturnal enuresis, is a common yet often misunderstood condition that can affect both children and adults. It occurs when an individual involuntarily releases urine during sleep, leading to wet sheets and a sense of embarrassment or frustration. In children, bedwetting is commonly attributed to factors such as a delay in bladder maturity, genetics, or a hormone imbalance. For adults, underlying medical conditions, stress, or lifestyle factors may contribute to nocturnal enuresis. It’s important to note that bedwetting is not typically caused by laziness, disobedience, or psychological issues. Understanding the causes and triggers of bedwetting is crucial for effective management and treatment. Strategies such as reminding children to use the bathroom before bed, limiting fluid intake before bedtime, or exploring natural remedies or therapies may help address bedwetting in children. For adults, addressing any underlying medical conditions, reducing stress levels, and implementing lifestyle modifications could be beneficial. By gaining a deeper understanding of bedwetting, we can provide support and guidance to individuals and their families who may be facing this challenge.
Causes of Bedwetting in Children
Causes of Bedwetting in Children
Bedwetting, or nocturnal enuresis, is a common issue among children, and there are several factors that can contribute to this condition. Understanding these causes can help parents and caregivers better manage bedwetting and provide appropriate support for their child.
1. Delayed development: In some children, the bladder and nervous system may take longer to develop, leading to difficulty in controlling the bladder during sleep. As they age and their body matures, bedwetting typically resolves on its own.
2. Genetics: Bedwetting has been found to run in families, suggesting a genetic component. If one or both parents had a history of bedwetting, there is an increased likelihood that their child may also experience it.
3. Hormonal imbalance: The production of an antidiuretic hormone, which helps reduce urine production at night, may be insufficient in some children who wet the bed. This can result in a higher volume of urine during sleep and contribute to bedwetting.
4. Overactive bladder: Some children may have an overactive bladder, which means the bladder muscles contract involuntarily, leading to sudden urges to urinate and potential bedwetting.
5. Urinary tract infections (UTIs): UTIs can cause irritation and inflammation in the urinary tract, increasing the frequency and urgency to urinate. Bedwetting can be a symptom of an underlying UTI.
6. Psychological factors: Emotional stress, anxiety, or a significant life event, such as starting school or dealing with family changes, can contribute to bedwetting in some children.
It’s important to note that certain foods and beverages, such as caffeine and citrus fruits, can irritate the bladder and increase urine production, potentially exacerbating bedwetting episodes. By identifying and avoiding these triggers, parents can help manage the condition more effectively.
Understanding the underlying causes of bedwetting in children is crucial in determining the appropriate course of action. In the next section, we will explore bedwetting in adults, its causes, and implications.
Bedwetting in Adults: Causes and Implications
Bedwetting in Adults: Causes and Implications
While bedwetting is commonly associated with children, it is important to acknowledge that it can also affect adults. Adult bedwetting, also known as adult enuresis, can be distressing and have significant implications on an individual’s quality of life. Understanding the causes behind adult bedwetting is crucial for proper management and treatment.
1. Underlying Medical Conditions: Adult bedwetting can be a symptom of an underlying medical condition. Conditions such as urinary tract infections, bladder dysfunction, diabetes, or neurological disorders can contribute to bedwetting. Treating the underlying condition is essential in managing adult bedwetting.
2. Medications: Certain medications can interfere with bladder control and contribute to adult bedwetting. Medications used to treat high blood pressure, psychiatric disorders, or diuretics can increase urine production or affect nerve signals, resulting in bedwetting. Consulting with a healthcare professional can help identify if medication is the cause and explore alternative options if necessary.
3. Hormonal Imbalance: Hormonal imbalances, such as a decrease in antidiuretic hormone (ADH) production, can disrupt the body’s ability to control urine production. ADH helps the kidneys concentrate urine during sleep, but a deficiency can lead to increased urine production and bedwetting. Hormonal therapy may be recommended to address this imbalance.
4. Stress and Emotional Factors: Psychological stress, anxiety, or emotional trauma can contribute to adult bedwetting. These factors can impact the brain-bladder connection, leading to involuntary urination during sleep. Therapy, stress management techniques, and counseling may be beneficial in addressing the underlying emotional factors.
5. Alcohol and Fluid Intake: Consuming alcohol or excessive fluids close to bedtime can increase urine production and contribute to adult bedwetting. Limiting alcohol consumption and managing fluid intake, especially in the evening, may help reduce the frequency of bedwetting episodes.
It is important for individuals experiencing adult bedwetting to consult with a healthcare professional to determine the underlying cause. Identifying the root cause will guide appropriate treatment strategies, which may include medication, lifestyle modifications, pelvic floor exercises, or behavioral therapies. By addressing the underlying causes, individuals can effectively manage adult bedwetting and minimize its impact on their daily lives. For more information on managing bedwetting, you can refer to our article on foods and bedwetting.
The Potential Link: Sleep Disorders and Bedwetting
The Potential Link: Sleep Disorders and Bedwetting
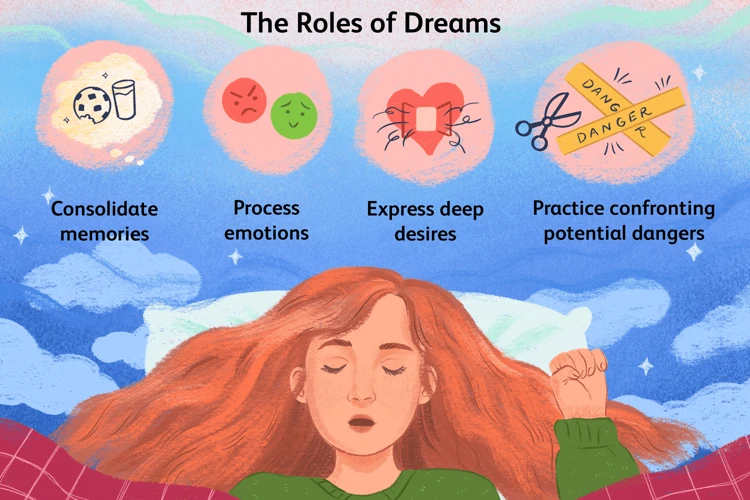
The potential link between sleep disorders and bedwetting is complex and multifaceted. On one hand, sleep disorders can disrupt the normal sleep architecture, leading to fragmented sleep and making it difficult for individuals to wake up when their bladder is full during the night. This can contribute to bedwetting episodes, especially in children who may have a harder time waking up to use the restroom. On the other hand, bedwetting itself can also contribute to sleep disturbances. The embarrassment and anxiety caused by bedwetting can lead to poor sleep quality and even impact dreams and sleep-related experiences. In fact, studies have shown a correlation between bedwetting and vivid dreams, suggesting a potential psychological component to the connection between bedwetting and sleep disorders. Understanding this potential link is crucial for developing appropriate treatment strategies that address both the underlying sleep disorder and the bedwetting issue. By targeting both aspects, individuals can have a better chance of achieving restful sleep and reducing the occurrence of bedwetting.
The Impact of Sleep Disorders on Bedwetting
The Impact of Sleep Disorders on Bedwetting
Sleep disorders can significantly impact bedwetting, exacerbating the frequency and severity of nocturnal enuresis. One of the main ways sleep disorders contribute to bedwetting is through disrupted sleep patterns. When individuals with sleep disorders experience fragmented or shallow sleep, they may have difficulty waking up when their bladder is full. This can result in a higher likelihood of bedwetting episodes throughout the night.
Sleep disorders, such as sleep apnea, can also create physiological changes that directly impact bladder control. Sleep apnea causes interruptions in breathing during sleep, leading to oxygen deprivation and increased pressure on the bladder. This increased pressure can make it more difficult to maintain bladder control during the night, increasing the chances of bedwetting occurrences.
Certain sleep disorders can disrupt the hormone balance in the body, which plays a crucial role in regulating both sleep and bladder function. For example, conditions like insomnia or restless leg syndrome can lead to imbalances in hormones such as melatonin and cortisol. These hormonal imbalances can affect the coordination between the brain and the bladder, potentially leading to nighttime accidents.
It is important to note that the specific impact of sleep disorders on bedwetting may vary from person to person. Some individuals may experience a more profound connection between their sleep disorder and nocturnal enuresis, while others may not see as significant an impact.
Understanding the impact of sleep disorders on bedwetting is essential for developing effective treatment strategies. By addressing the underlying sleep disorder, individuals may experience improvements in their overall sleep quality and potentially see a reduction in bedwetting incidents. In the next section, we will explore how bedwetting itself can contribute to the development or exacerbation of sleep disorders.
How Bedwetting May Contribute to Sleep Disorders
How Bedwetting May Contribute to Sleep Disorders
Bedwetting itself can be a symptom of an underlying sleep disorder, but it can also potentially contribute to the development or worsening of sleep disturbances. Here are some ways in which bedwetting may impact sleep disorders:
1. Sleep Fragmentation: Bedwetting episodes can disrupt sleep by forcing the individual to wake up to change their clothes or bedding. These awakenings can fragment sleep and prevent the person from reaching deep, restorative sleep stages. As a result, they may experience excessive daytime sleepiness, fatigue, and decreased cognitive function.
2. Anxiety and Stress: Living with bedwetting can lead to significant levels of anxiety and stress, particularly in children and young adults. The fear of potential accidents during sleep can create anticipation and worry, making it difficult to fall asleep and maintain a relaxed state of mind. Heightened stress levels can exacerbate existing sleep disorders or contribute to the development of new ones.
3. Sleep-related Disorders: Bedwetting can be associated with certain sleep-related disorders, such as sleepwalking or night terrors. These conditions can further disrupt sleep architecture and increase the risk of accidents during the night. In some cases, bedwetting may occur during vivid or distressing dreams, impacting both sleep quality and the individual’s emotional well-being.
4. Impact on Bed Partner’s Sleep: Bedwetting can also affect the sleep quality of a bed partner, especially in the case of couples sharing a bed. Frequent awakenings and disturbances caused by bedwetting can disrupt the partner’s sleep as well, leading to their own sleep disorders or exacerbating existing ones.
It’s important to recognize the potential bidirectional relationship between bedwetting and sleep disorders. Addressing bedwetting through appropriate interventions, such as alarm systems, bladder training exercises, and lifestyle changes, can not only help manage the condition but also improve sleep quality and potentially alleviate associated sleep disorders. Understanding the intricate connection between bedwetting and sleep disorders allows for a comprehensive approach to treatment and management. To learn more about the impact of dreams on bedwetting, you can read our previous article on “How Dreams May Influence Bedwetting”.
Treatment and Management
Addressing sleep disorders and managing bedwetting can greatly improve the quality of life for individuals dealing with both issues. Treatment options for sleep disorders may include lifestyle changes, such as establishing a consistent sleep schedule, creating a relaxing bedtime routine, and avoiding stimulants like caffeine or electronic devices before bed. In some cases, medical interventions like Continuous Positive Airway Pressure (CPAP) machines or dental devices may be recommended. When it comes to managing bedwetting, it’s important to create a supportive and understanding environment, especially for children. Strategies may include limiting fluid intake before bedtime, using bedwetting alarms to awaken the individual when they start to urinate, and encouraging regular bathroom visits throughout the day. For adults, various treatment approaches, including medication, pelvic floor exercises, and behavioral therapies, can be explored. Seeking medical advice and guidance is essential to determine the most effective treatment plan tailored to individual needs.
Addressing Sleep Disorders
Addressing Sleep Disorders
When it comes to addressing sleep disorders, it is important to seek professional guidance and diagnosis from a healthcare provider specializing in sleep medicine. This will ensure an accurate assessment of the specific sleep disorder at hand. Treatment options for sleep disorders can vary depending on the underlying cause and severity of the condition.
For sleep disorders like insomnia, non-medical interventions and lifestyle changes may be recommended. These can include improving sleep hygiene, such as maintaining a consistent sleep schedule, creating a conducive sleep environment, and practicing relaxation techniques before bedtime. Cognitive-behavioral therapy for insomnia (CBT-I) is also an effective approach that helps modify behaviors and thoughts related to sleep.
In cases of sleep apnea, where breathing pauses intermittently during sleep, continuous positive airway pressure (CPAP) therapy is often the primary treatment. This involves wearing a mask connected to a machine that delivers a steady flow of air pressure to keep the airways open. Other treatment options may include oral appliances, positional therapy, and, in severe cases, surgery.
For sleep disorders caused by underlying medical conditions, addressing and managing the underlying condition may help improve sleep quality. This can involve medication, therapy, or lifestyle modifications to alleviate symptoms and minimize sleep disruption.
It is crucial to remember that each sleep disorder requires a personalized approach to treatment. What works for one person may not work for another. Consulting with a healthcare professional will ensure the most appropriate and effective treatment plan is implemented. Don’t let sleep disorders continue to impact your overall well-being. Seek the help you need and take steps towards a better, more restful night’s sleep.
Managing Bedwetting in Children and Adults
Managing Bedwetting in Children and Adults
When it comes to managing bedwetting in both children and adults, understanding the underlying causes is crucial to developing effective strategies. Here are some approaches to consider:
1. Establish a Routine: Creating a consistent bedtime routine can help regulate sleep patterns and bladder function. Encourage regular bathroom visits before bedtime to empty the bladder.
2. Limit Fluid Intake: Limiting fluids, especially caffeine and sugary beverages, in the evening can reduce the likelihood of bedwetting episodes. However, it is essential to ensure adequate hydration throughout the day.
3. Bedwetting Alarms: Bedwetting alarms can be effective in training the brain to recognize the sensation of a full bladder and wake up in response. These alarms usually consist of a moisture sensor and an audible or vibrating alarm. When moisture is detected, the alarm goes off, prompting the individual to wake up and use the bathroom.
4. Positive Reinforcement: Encourage and praise children or adults for dry nights. This positive reinforcement can boost their confidence and motivation to overcome bedwetting.
5. Bladder Training: Bladder training exercises involve gradually increasing the time between bathroom visits during the day to help increase the bladder’s holding capacity.
6. Medications: In certain cases, a doctor may prescribe medication to help manage bedwetting. These medications work by either reducing urine production or increasing the bladder’s capacity.
7. Emotional Support: Bedwetting can be emotionally distressing, especially for children. Providing emotional support, reassurance, and understanding can go a long way in helping them cope with the condition.
It is important to note that treatment approaches may vary depending on the individual’s age, medical history, and the severity of bedwetting. Consulting with a healthcare professional is essential for proper evaluation and guidance.
Remember, managing bedwetting requires patience and persistence. By implementing these strategies and seeking appropriate medical advice, both children and adults can take proactive steps towards overcoming bedwetting and achieving restful nights of sleep.
Conclusion
Conclusion
In conclusion, the connection between sleep disorders and bedwetting is a complex and multifaceted issue. While research is still ongoing, there is evidence to suggest that sleep disorders can contribute to bedwetting and vice versa. Understanding this relationship is crucial for effective treatment and management.
For individuals experiencing both sleep disorders and bedwetting, it is important to seek medical evaluation and diagnosis. Addressing sleep disorders through various treatment options, such as medication, therapy, or lifestyle changes, can help improve sleep quality and potentially reduce bedwetting episodes.
Managing bedwetting in both children and adults involves implementing strategies such as limiting fluid intake before bedtime, establishing a regular toilet routine, and using protective bedding or waterproof mattress covers. It is essential to provide emotional support and understanding for individuals dealing with bedwetting, as it can often lead to feelings of shame or embarrassment.
If you or your child is struggling with sleep disorders and bedwetting, remember that you are not alone. Consulting with healthcare professionals, such as doctors, pediatricians, or sleep specialists, can provide valuable guidance and support.
By addressing both sleep disorders and bedwetting, individuals can experience improved sleep quality, enhanced overall well-being, and a better quality of life. So, take the first step towards finding relief and consult with a medical professional to develop a personalized treatment and management plan.
Remember, sleep disorders and bedwetting can be managed and overcome. With the right approach and support, individuals can achieve restful nights and wake up to a brighter, drier future.
Frequently Asked Questions
1. Can sleep disorders cause bedwetting in children?
Yes, certain sleep disorders can disrupt the normal sleep patterns and bladder control in children, potentially leading to bedwetting.
2. Are bedwetting and sleep apnea related?
There is evidence to suggest a possible link between sleep apnea and bedwetting, as the increased pressure on the bladder during sleep can contribute to nocturnal enuresis.
3. Can bedwetting be a symptom of restless leg syndrome?
While it is not a direct symptom of restless leg syndrome, the disrupted sleep patterns and involuntary movements associated with this condition can potentially contribute to bedwetting episodes.
4. Are there any hormonal factors involved in bedwetting?
Yes, the hormones involved in regulating sleep and those involved in controlling bladder function can interact, potentially influencing the prevalence of bedwetting in individuals.
5. Is bedwetting in adults a common phenomenon?
Nocturnal enuresis in adults, although less frequent than in children, is more common than many people realize and can have various underlying causes.
6. Can psychological factors contribute to bedwetting?
Yes, psychological factors such as stress, anxiety, and emotional disturbances can play a role in bedwetting for both children and adults.
7. Is bedwetting only a nighttime occurrence?
In most cases, bedwetting occurs during sleep, specifically at night. However, some individuals may also experience bedwetting during daytime naps.
8. Is bedwetting a hereditary condition?
There seems to be a hereditary component to bedwetting, as it often runs in families. If one or both parents experienced bedwetting as children, their children are more likely to have the condition as well.
9. Can certain medications contribute to bedwetting?
Yes, some medications, such as certain antidepressants or diuretics, can affect bladder control and potentially contribute to bedwetting episodes.
10. Can bedwetting be treated successfully?
Absolutely! Both sleep disorders and bedwetting can be effectively managed and treated through various approaches, including lifestyle changes, behavioral therapies, medication, and addressing any underlying medical conditions.








