Sleep Apnea is a common but often undiagnosed sleep disorder that can have serious implications on a person’s health and overall well-being. When individuals suffer from sleep apnea, they experience interruptions in their breathing during sleep, which can lead to a range of symptoms and health complications. It is important to understand the different types of sleep apnea, the signs and symptoms to watch out for, and the available treatment options. In this comprehensive guide, we will explore sleep apnea in detail, including its types, symptoms, and possible solutions. So grab a cup of coffee and prepare to dive into the fascinating world of sleep apnea.
What is Sleep Apnea?
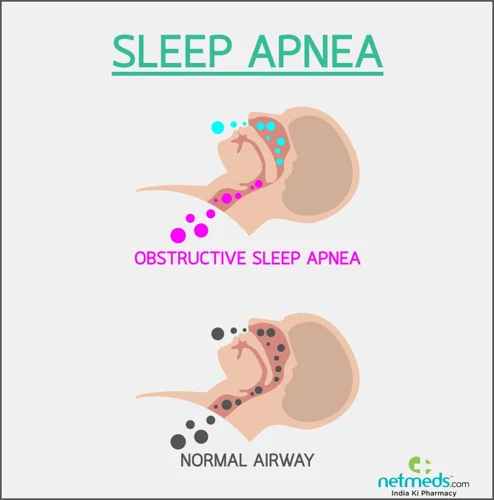
Sleep apnea is a sleep disorder characterized by repeated pauses or interruptions in breathing during sleep. These interruptions, known as apneas, can last for a few seconds to a minute and can occur multiple times throughout the night. The most common type of sleep apnea is obstructive sleep apnea (OSA), which occurs when the throat muscles relax and block the airway. Another type is central sleep apnea (CSA), where the brain fails to send the proper signals to the muscles that control breathing. Complex sleep apnea syndrome (CompSAS) is a combination of both OSA and CSA.
During an apnea episode, the oxygen levels in the blood decrease, and carbon dioxide levels increase, triggering the brain to awaken briefly to restore proper breathing. These awakenings are often so brief that individuals with sleep apnea may not remember them. However, they disrupt the normal sleep cycle, preventing the person from getting adequate restorative sleep.
Sleep apnea can have significant effects on a person’s health and quality of life. The pauses in breathing can cause disruptions in sleep, resulting in excessive daytime sleepiness, difficulty concentrating, and irritability. The repeated drops in oxygen levels can also put strain on the heart and increase the risk of cardiovascular problems.
It is important to differentiate sleep apnea from other sleep disorders, such as narcolepsy or sleep paralysis. While narcolepsy is a neurological disorder characterized by excessive daytime sleepiness and sudden loss of muscle control, sleep paralysis refers to the temporary inability to move or speak while falling asleep or upon waking up.
Understanding sleep apnea is crucial for identifying the symptoms, seeking proper diagnosis, and exploring treatment options. So let’s delve deeper into the different types of sleep apnea and their distinct characteristics. For more information about other sleep disorders, you can read our related articles on narcolepsy, sleep paralysis, and sleepwalking.
Types of Sleep Apnea

There are three main types of sleep apnea: obstructive sleep apnea (OSA), central sleep apnea (CSA), and complex sleep apnea syndrome (CompSAS). Obstructive sleep apnea (OSA) is the most common type and occurs when the throat muscles relax and block the airway during sleep. This results in pauses in breathing and lowered oxygen levels. Central sleep apnea (CSA), on the other hand, is caused by a failure of the brain to send the proper signals to the muscles that control breathing. This leads to a lack of effort to breathe during sleep. Complex sleep apnea syndrome (CompSAS) is a combination of both OSA and CSA, where individuals experience both obstructive blockages and a lack of effort to breathe. It is important to determine the type of sleep apnea a person has in order to provide appropriate treatment and management options.
1. Obstructive Sleep Apnea (OSA)
Obstructive Sleep Apnea (OSA) is the most common type of sleep apnea. It occurs when the muscles in the back of the throat relax, leading to a partial or complete blockage of the airway during sleep. This blockage restricts the flow of air and causes a pause in breathing. Individuals with OSA may experience frequent episodes of these pauses throughout the night, disrupting their sleep cycle and leading to various symptoms.
Causes: OSA can be caused by several factors, including obesity, which increases the amount of soft tissue in the throat that can obstruct the airway. Other risk factors include a large neck circumference, narrowed airway, nasal congestion, or structural abnormalities in the airway.
Symptoms: The signs of OSA often include loud snoring, gasping or choking during sleep, restless sleep, and excessive daytime sleepiness. Individuals with OSA may also wake up with a dry mouth or sore throat. Additionally, they may experience morning headaches, difficulty concentrating, and irritability.
Diagnosis: To diagnose OSA, a healthcare professional may review the individual’s medical history, conduct a physical examination, and recommend a sleep study, also known as a polysomnography. This study monitors various aspects of sleep, including brain activity, heart rate, breathing patterns, and oxygen levels.
Treatment: There are various treatment options available for OSA. Lifestyle changes, such as losing weight, can help reduce symptoms. Continuous Positive Airway Pressure (CPAP) therapy is a common and effective treatment for OSA. It involves wearing a mask over the nose or mouth during sleep, which delivers a continuous flow of air to keep the airway open. Dental devices, such as oral appliances, may also be prescribed to help keep the airway open. In some cases, surgery may be recommended to correct any structural issues in the throat or airway that contribute to OSA.
Management: Along with treatment, certain lifestyle modifications can help manage OSA. Sleeping on the side rather than the back can help keep the airway open. Weight management through a balanced diet and regular exercise can also be beneficial. Avoiding alcohol and sedatives, which can relax the throat muscles and worsen symptoms, is important. Establishing and maintaining a consistent sleep schedule can also contribute to better sleep quality.
Obstructive Sleep Apnea is a serious sleep disorder that requires proper diagnosis and treatment. By understanding the causes, symptoms, diagnosis, treatment options, and management strategies for OSA, individuals can take proactive steps towards improving their sleep quality and overall well-being.
2. Central Sleep Apnea (CSA)
Central Sleep Apnea (CSA) is a less common type of sleep apnea compared to obstructive sleep apnea (OSA). Unlike OSA, which is primarily caused by physical obstructions in the airway, CSA occurs when the brain fails to send proper signals to the muscles responsible for controlling breathing during sleep.
In individuals with CSA, the brain’s respiratory control center does not function correctly, leading to abnormal breathing patterns. The muscles that facilitate breathing do not receive the necessary signals to contract and expand the lungs. As a result, there is a lack of effort to breathe, and no airflow is produced. This pause in breathing can last for several seconds or even minutes.
Central sleep apnea can be caused by various factors, including certain medical conditions that affect the brainstem, such as stroke, congestive heart failure, or neurological disorders like Parkinson’s disease. Medications such as opioids and sedatives can also contribute to the development of CSA.
The symptoms of CSA are similar to those of OSA and may include loud snoring, morning headaches, excessive daytime sleepiness, and difficulty concentrating. However, individuals with CSA may not have the typical signs of upper airway obstruction seen in OSA, such as choking or gasping for air during sleep.
Diagnosing CSA involves a comprehensive sleep study called polysomnography, which measures various physiological factors during sleep, including brain activity, heart rate, oxygen levels, and respiratory effort. This test helps to determine the presence and severity of central sleep apnea.
Treatment options for CSA differ from those for OSA. In some cases, treating the underlying medical condition, such as heart failure or Parkinson’s disease, can alleviate CSA symptoms. Continuous positive airway pressure (CPAP) therapy may also be used to help maintain a consistent airflow during sleep and improve breathing.
In more severe cases, adaptive servo-ventilation (ASV) therapy may be recommended. ASV devices monitor the individual’s breathing patterns and deliver pressure support to assist with inhalation and exhalation, promoting regular breathing throughout the night.
It is important to consult with a healthcare professional if you suspect you may have central sleep apnea. They can provide an accurate diagnosis and recommend appropriate treatment options to help manage the condition and improve your quality of sleep and overall health.
3. Complex Sleep Apnea Syndrome (CompSAS)
Complex Sleep Apnea Syndrome (CompSAS) is a unique form of sleep apnea that combines features of both Obstructive Sleep Apnea (OSA) and Central Sleep Apnea (CSA). Also known as Treatment-Emergent Central Sleep Apnea, CompSAS is typically seen in individuals who initially had OSA and were being treated with Continuous Positive Airway Pressure (CPAP) therapy.
Unlike OSA, where the airway is blocked by relaxed throat muscles, CompSAS involves a mix of both obstructive and central respiratory events. This means that in addition to the physical blockage of the airway, there are also moments when the brain fails to send the proper signals to control breathing.
The exact cause of CompSAS is not fully understood, but studies suggest that the use of CPAP therapy may play a role. CPAP is a common treatment for OSA, where a machine delivers a continuous flow of air through a mask to keep the airway open during sleep. However, in some cases, the use of CPAP can trigger or worsen central sleep apnea, leading to the development of CompSAS.
The symptoms of CompSAS can vary, but often include the hallmark features of both OSA and CSA. These may include loud snoring, excessive daytime sleepiness, morning headaches, and difficulty concentrating. It is important to diagnose and treat CompSAS promptly to prevent further complications and ensure adequate sleep and overall well-being.
Managing CompSAS typically involves a combination of treatment approaches, including adjusting CPAP settings, using adaptive servo-ventilation devices, or trying alternative therapies like bilevel positive airway pressure (BiPAP). Regular monitoring and follow-up with a sleep specialist are essential to fine-tune the treatment according to individual needs.
While CompSAS is less common than OSA and CSA, knowledge and awareness of this condition are crucial. By understanding the symptoms and available treatment options, individuals with CompSAS can work with their healthcare providers to manage their sleep apnea effectively and improve their overall sleep quality and health.
Signs and Symptoms

Recognizing the signs and symptoms of sleep apnea is essential for early detection and proper management of the condition. One of the most common indications of sleep apnea is loud snoring. Individuals with sleep apnea often snore loudly and consistently, sometimes accompanied by gasping or choking sounds. Additionally, frequent pauses in breathing during sleep, known as apneas, are another telltale sign. These pauses can occur multiple times throughout the night and may be observed by a bed partner or family member. Excessive daytime sleepiness is another prominent symptom of sleep apnea, as the interrupted sleep leaves individuals feeling tired and fatigued during the day. Morning headaches, difficulty concentrating, and irritability are also common symptoms. If you suspect you or a loved one may be experiencing these symptoms, it is crucial to consult a healthcare professional for further evaluation and diagnosis.
1. Loud Snoring
– Loud snoring is one of the most common and noticeable symptoms of sleep apnea. It occurs when the airflow is partially blocked during sleep, leading to vibrations in the throat tissues. The snoring sound can be disruptive to both the person with sleep apnea and their sleep partner. It is often described as loud, chronic, and can occur throughout the night or in frequent episodes.
– Snoring is more commonly associated with obstructive sleep apnea (OSA). In OSA, the relaxed throat muscles and tissues partially or completely block the airway, causing the snoring sound as the individual struggles to breathe. It is important to note that not everyone who snores has sleep apnea, but loud and persistent snoring should not be ignored, as it can be a potential sign of an underlying sleep disorder.
– Loud snoring can also be accompanied by other symptoms such as gasping or choking sounds as the person with sleep apnea tries to breathe. These sounds indicate that the airway is completely or almost completely blocked, leading to brief awakenings to restore normal breathing.
– It is essential to consult a healthcare professional if loud snoring is a persistent and bothersome issue. A comprehensive evaluation, including a detailed medical history and sleep study, can help determine if sleep apnea or another sleep disorder is the cause of the snoring. Treatment options can then be explored to manage the underlying sleep apnea and alleviate the disruptive snoring.
By understanding the significance of loud snoring as a potential symptom of sleep apnea, individuals can take the necessary steps to seek evaluation and treatment to improve their sleep quality and overall health.
2. Frequent and Pauses in Breathing
Frequent pauses in breathing, also known as apneas, are a key symptom of sleep apnea. These pauses can occur multiple times throughout the night and can last for a few seconds to a minute. During these episodes, the individual’s airflow is significantly reduced or completely blocked, resulting in a lack of oxygen intake. As a result, the body briefly wakes up to resume normal breathing, often accompanied by choking or gasping sensations.
To illustrate the severity of this symptom, it may be helpful to provide a list outlining the possible consequences:
- Disruption of sleep: The constant interruptions in breathing prevent individuals with sleep apnea from progressing through the various sleep stages properly. Consequently, they experience fragmented and poor-quality sleep, leading to daytime sleepiness and fatigue.
- Impact on cognitive function: The frequent awakenings and inadequate sleep can impair cognitive functions, such as concentration, memory, and problem-solving abilities. This can affect performance at work or school and increase the risk of accidents.
- Affected cardiovascular system: The disruptions in breathing cause changes in blood oxygen levels and increase the heart’s workload. Over time, this can lead to high blood pressure, heart disease, and an increased risk of stroke.
- Decreased quality of life: Sleep apnea can have a significant impact on a person’s overall well-being. The constant fatigue and sleepiness can result in irritability, mood swings, and a decreased enjoyment of daily activities.
- Relationship strain: The loud snoring and intermittent pauses in breathing can disrupt a bed partner’s sleep, leading to frustration and strain in the relationship.
It is imperative to recognize the signs of frequent pauses in breathing as a potential symptom of sleep apnea. Seeking medical attention for proper diagnosis and exploring appropriate treatment options is essential for managing the disorder and improving overall health and well-being.
3. Excessive Daytime Sleepiness
Excessive daytime sleepiness (EDS) is a common symptom experienced by individuals with sleep apnea. It refers to a persistent and overwhelming feeling of drowsiness and the irresistible urge to sleep during the day, even after a full night’s sleep. EDS can significantly impact a person’s quality of life, affecting their productivity, concentration, and overall well-being.
Here are some key points to know about excessive daytime sleepiness in relation to sleep apnea:
1. Impact on daily functioning: Individuals with EDS may find it challenging to stay awake and alert throughout the day, leading to difficulties in performing daily activities, such as work, school, or even driving. The excessive sleepiness can make it hard to concentrate, negatively affecting cognitive abilities and impairing memory.
2. Causes of EDS in sleep apnea: EDS in sleep apnea is primarily caused by disrupted sleep patterns. The frequent awakenings and pauses in breathing during the night prevent individuals from reaching the deep, restorative stages of sleep. As a result, they wake up feeling fatigued and continue to experience daytime sleepiness.
3. Risk factors for EDS: Not everyone with sleep apnea will experience EDS, but certain factors may increase the likelihood of its occurrence. These include obesity, age (middle-aged and older adults are more prone to EDS), sedentary lifestyle, and the severity of sleep apnea.
4. Impact on mental health: EDS can also have a significant impact on mental health. Sleep deprivation caused by untreated sleep apnea can contribute to increased levels of stress, anxiety, and depression. It can also lead to irritability, mood swings, and a decreased overall sense of well-being.
5. Effective management of EDS: Treating the underlying sleep apnea can help alleviate excessive daytime sleepiness. By addressing the interrupted breathing during sleep, individuals can achieve better sleep quality and reduce daytime sleepiness. Treatment options may include lifestyle modifications, continuous positive airway pressure (CPAP) therapy, dental devices, surgery, or expiratory positive airway pressure (EPAP).
If you find yourself experiencing excessive daytime sleepiness along with other symptoms of sleep apnea, it is important to consult with a healthcare professional for proper diagnosis and treatment. A comprehensive evaluation can help determine the best approach to manage EDS and improve your overall sleep quality and daytime functioning.
4. Morning Headaches
Morning headaches are a common symptom associated with sleep apnea. Individuals who suffer from sleep apnea often wake up with headaches that can range from mild discomfort to severe migraines. These headaches typically occur due to the disruption of the normal sleep cycle caused by sleep apnea.
When a person has sleep apnea, their breathing pauses multiple times throughout the night, leading to oxygen deprivation in the brain. This lack of oxygen can cause blood vessels in the brain to expand and trigger headaches. Additionally, the frequent awakenings and disturbances in sleep patterns can result in heightened tension and stress levels, further contributing to morning headaches.
It is important to note that morning headaches caused by sleep apnea differ from normal tension headaches or migraines. They are specifically associated with the sleep apnea condition and are more likely to occur in individuals who experience other symptoms of sleep apnea, such as snoring, fatigue, and pauses in breathing during sleep.
If you consistently wake up with morning headaches, it is essential to consider the possibility of sleep apnea. Seeking a proper diagnosis from a healthcare professional is crucial in order to determine the underlying cause of the headaches and to develop an appropriate treatment plan.
In the next section, we will explore the various diagnostic methods and tests used to identify sleep apnea, including medical history evaluations, physical exams, and sleep studies (polysomnography). Understanding the signs and symptoms of sleep apnea, including morning headaches, can help individuals take the necessary steps towards managing their condition and improving their overall quality of life.
5. Difficulty Concentrating
Difficulty concentrating is a common symptom experienced by individuals with sleep apnea. The interruptions in breathing during sleep can lead to fragmented and poor-quality sleep, resulting in daytime fatigue and cognitive impairment. When the brain does not receive enough restful sleep, it becomes challenging to maintain focus and concentration throughout the day.
Individuals with sleep apnea may find it difficult to concentrate on tasks at work or school, leading to decreased productivity and performance. They may struggle with memory recall and have trouble staying engaged in conversations or activities. This cognitive impairment can have a significant impact on one’s daily life, making it harder to function effectively and efficiently.
The lack of restorative sleep caused by sleep apnea affects the brain’s ability to consolidate memories and process information. Research has shown that untreated sleep apnea is associated with cognitive decline and an increased risk of developing conditions such as dementia and Alzheimer’s disease.
Fortunately, treating sleep apnea can help improve concentration and cognitive function. By addressing the underlying cause of the interrupted sleep, individuals with sleep apnea can experience better sleep quality, leading to enhanced mental clarity and focus. Treatment options such as continuous positive airway pressure (CPAP) therapy, dental devices, and lifestyle modifications can be effective in managing sleep apnea and alleviating the associated cognitive difficulties.
If you’re experiencing difficulty concentrating and suspect that sleep apnea may be the underlying cause, it’s important to consult with a healthcare professional for proper evaluation and diagnosis. Treating sleep apnea not only improves concentration but also contributes to overall health and well-being.
Diagnosis and Testing
Diagnosing sleep apnea involves a comprehensive evaluation of a person’s medical history, physical exams, and specialized sleep studies. Medical professionals will inquire about symptoms and risk factors, such as loud snoring, excessive daytime sleepiness, obesity, and family history of sleep apnea. Physical examinations may include assessing the nasal passages, throat, and neck for any structural abnormalities that could contribute to sleep apnea. Sleep studies, also known as polysomnography, are typically conducted in sleep centers or using home sleep testing devices to monitor various physiological factors during sleep. These studies measure brain waves, heart rate, oxygen levels, and breathing patterns to determine the severity and type of sleep apnea. By accurately diagnosing sleep apnea, healthcare providers can recommend appropriate treatment options to help individuals manage their condition effectively and improve their overall sleep quality.
1. Medical History and Physical Exams
When diagnosing sleep apnea, medical history and physical exams play a crucial role in identifying potential risk factors and symptoms. Here is a breakdown of the steps involved in the medical history and physical examination process:
1. Patient Interview: The healthcare provider will conduct a comprehensive interview with the patient to gather information about their sleep patterns, daytime symptoms, and any existing medical conditions. This interview helps in understanding the patient’s sleep history and identifying potential risk factors for sleep apnea.
2. Family History: The healthcare provider may inquire about the patient’s family history, as sleep apnea can sometimes have a genetic component. Having a close relative with sleep apnea increases the likelihood of developing the condition.
3. Physical Examination: During the physical exam, the healthcare provider will assess various factors that can contribute to sleep apnea. This may include measuring the patient’s body mass index (BMI) to determine if excess weight is a factor. They may also examine the patient’s neck circumference, as a thicker neck can contribute to airway blockages.
4. Upper Airway Evaluation: To assess the airway and identify any structural abnormalities or obstructions, the healthcare provider may perform an examination using tools such as a mirror or a fiberoptic scope. This evaluation helps determine if the airway is narrow or if there are any physical obstructions that could contribute to sleep apnea.
5. Assessment of Associated Symptoms: The healthcare provider will also evaluate symptoms that may indicate sleep apnea, such as high blood pressure, morning headaches, or excessive daytime sleepiness. These symptoms, combined with the patient’s medical history and physical exam findings, help in making an accurate diagnosis.
It is important to note that a medical history and physical exam alone cannot provide a definitive diagnosis of sleep apnea. Further testing, such as sleep studies, is typically required to confirm the presence and severity of the condition. However, the medical history and physical exam serve as crucial initial steps in the diagnostic process, helping healthcare providers determine the need for additional testing and appropriate treatment options for their patients.
2. Sleep Studies (Polysomnography)
Sleep studies, specifically polysomnography (PSG), are an essential diagnostic tool used to evaluate and diagnose sleep apnea. Polysomnography involves the monitoring and recording of various physiological parameters during sleep, including brain activity, eye movements, heart rate, breathing patterns, and oxygen levels.
During a sleep study, the individual spends a night in a sleep laboratory or a specialized unit. The patient is connected to electrodes and sensors that measure brain waves, eye movements, and muscle activity. Additionally, belts are placed around the chest and abdomen to monitor breathing patterns, and sensors are attached to the finger to measure oxygen levels. These recordings allow experts to analyze the sleep architecture and identify any abnormalities or disturbances in breathing patterns.
The data collected during polysomnography is analyzed by sleep specialists who can determine the presence and severity of sleep apnea. The number of apnea and hypopnea events per hour is calculated to establish the apnea-hypopnea index (AHI) or respiratory disturbance index (RDI). This index helps classify the severity of sleep apnea as mild, moderate, or severe.
In some cases, portable home sleep apnea tests may be conducted instead of an in-lab polysomnography study. These tests involve the use of simplified monitoring devices that can be worn at home to collect data while the individual sleeps. Home sleep tests are more convenient and cost-effective but may not provide as comprehensive information as an in-lab study.
Sleep studies, including polysomnography, are vital in diagnosing sleep apnea accurately. They provide valuable insights into the individual’s sleep patterns, breathing abnormalities, and overall sleep quality. Based on the results of a sleep study, healthcare professionals can recommend appropriate treatment options tailored to the severity and specific needs of the patient.
Please note that only qualified healthcare professionals can interpret sleep study results and provide an accurate diagnosis. If you suspect you have sleep apnea, it is essential to consult a sleep specialist for a thorough evaluation.
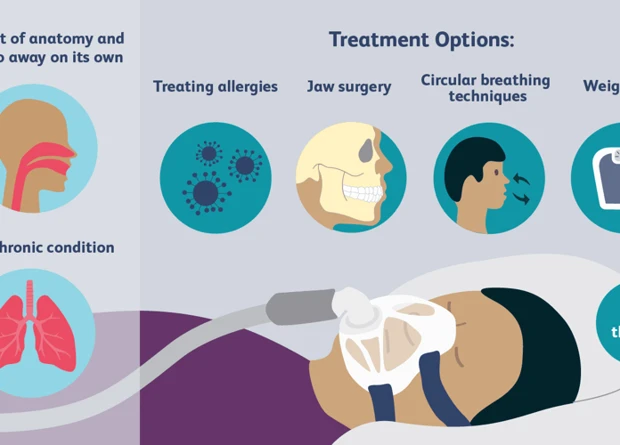
Treatment Options
When it comes to treating sleep apnea, there are several options available to help manage and alleviate the symptoms. These treatment options can range from lifestyle changes to medical interventions, depending on the severity of the condition.
Lifestyle changes: Making certain lifestyle modifications can be beneficial in managing sleep apnea. This includes weight loss, as excess weight can contribute to the development and worsening of the condition. Sleeping on your side instead of your back can also help keep the airway open during sleep.
Continuous Positive Airway Pressure (CPAP): CPAP is a commonly prescribed treatment for sleep apnea. It involves wearing a mask over the nose or mouth during sleep, which delivers a continuous flow of air pressure to keep the airway open. This helps prevent apneas and improves the quality of sleep.
Dental devices: Oral appliances or dental devices can be used to reposition the tongue and jaw, helping to keep the airway open during sleep. These devices are custom-made by a dentist and are designed to be comfortable and effective.
Surgery: In some cases, surgical intervention may be necessary to address structural issues that contribute to sleep apnea. This can involve removing excess tissue from the throat, repositioning the jaw, or correcting nasal abnormalities.
Expiratory Positive Airway Pressure (EPAP): EPAP devices, such as nasal strips or disks, are placed over the nostrils before sleep. They work by creating backpressure during exhalation, helping to keep the airway open.
It is crucial to consult with a healthcare professional to determine the most suitable treatment approach based on individual circumstances and the severity of sleep apnea. Successful management of sleep apnea can improve sleep quality, alleviate symptoms, and reduce the risk of associated health complications.
1. Lifestyle Changes
One of the primary treatment options for managing sleep apnea is making lifestyle changes. These changes can significantly improve symptoms and reduce the frequency of apnea episodes. Here are some lifestyle changes to consider:
1. Weight loss: Obesity is a significant risk factor for sleep apnea. Losing excess weight can help reduce the severity of apnea by relieving pressure on the airway. Incorporating a balanced diet and regular exercise into your routine can aid in weight management.
2. Regular exercise: Engaging in regular physical activity not only promotes weight loss but also improves overall cardiovascular health. Cardio exercises like walking, jogging, or swimming can strengthen the respiratory muscles and help maintain a healthy weight.
3. Quit smoking: Smoking can worsen the symptoms of sleep apnea by causing inflammation and fluid retention in the airway. Quitting smoking or avoiding secondhand smoke can improve both respiratory and overall health.
4. Limit alcohol and sedative use: Alcohol and sedatives relax the muscles, including those in the throat, which can increase the likelihood of airway blockage during sleep. Limiting or avoiding their consumption, especially in the evening, can promote better airflow during sleep.
5. Keep a regular sleep schedule: Establishing a consistent sleep routine helps regulate the body’s internal clock and promotes better sleep quality. Aim for a consistent bedtime and wake-up time, even on weekends, to ensure you get enough restorative sleep.
6. Elevate the head of your bed: Raising the head of your bed by a few inches using pillows or a bed wedge can help keep your airway open and prevent the tongue and soft tissues from obstructing the airflow.
Remember, lifestyle changes may not completely eliminate sleep apnea, but they can significantly improve symptoms and reduce the frequency of apnea episodes. If lifestyle modifications alone are not enough, further treatment options such as continuous positive airway pressure (CPAP) or dental devices may be recommended.
2. Continuous Positive Airway Pressure (CPAP)
Continuous Positive Airway Pressure (CPAP) is one of the most common and effective treatment options for sleep apnea. It involves wearing a mask over the nose or mouth while sleeping, which is connected to a machine that delivers a constant flow of air pressure to keep the airway open.
Here are some key points about CPAP:
– CPAP Machine: The CPAP machine consists of a motor that generates the airflow and a mask that delivers the air pressure to the airway. The machine can be adjusted to provide the appropriate level of pressure needed to keep the airway open during sleep.
– Mask Options: There are different types of masks available to suit individual preferences and needs. The most common types are nasal masks, which cover only the nose, and full-face masks, which cover both the nose and mouth. Some individuals may prefer nasal pillows, which are small inserts that fit into the nostrils.
– Benefits of CPAP: CPAP therapy effectively prevents the collapse of the airway during sleep, ensuring that individuals with sleep apnea can breathe continuously. This helps to eliminate snoring and improve the quality of sleep. By maintaining proper oxygen levels throughout the night, CPAP therapy also reduces the risk of associated health problems, such as cardiovascular issues, daytime fatigue, and cognitive impairment.
– Adjustment Period: While CPAP therapy is highly effective, some individuals may experience an adjustment period when they first start using the machine. It may take time to become comfortable with wearing the mask and using the prescribed pressure. To make the transition easier, it is recommended to start with a lower pressure setting and gradually increase it as needed.
– CPAP Maintenance: Regular maintenance of the CPAP equipment is important to ensure optimal performance and hygiene. This includes cleaning the mask, tubing, and humidifier regularly to prevent the buildup of bacteria or mold. It is also essential to replace parts as needed, such as the mask cushions or filters, to maintain effectiveness and comfort.
– Alternative Treatment Options: In some cases, individuals may find CPAP therapy uncomfortable or have difficulty adjusting to it. In such situations, alternative treatment options can be explored, such as bilevel positive airway pressure (BiPAP) machines, which provide different pressure levels for inhalation and exhalation, or automatic positive airway pressure (APAP) machines, which adjust the pressure automatically based on the individual’s needs.
It is important to note that CPAP therapy should be used consistently and in accordance with the healthcare provider’s recommendations. Regular follow-ups with the healthcare provider are essential to monitor the effectiveness of the treatment and make any necessary adjustments.
CPAP therapy has revolutionized the treatment of sleep apnea and has helped countless individuals achieve better sleep and improved overall health. Talk to your healthcare provider to determine if CPAP therapy is the right option for you.
3. Dental Devices
3. Dental Devices:
Dental devices, also known as oral appliances or mandibular advancement devices, are a non-invasive treatment option for sleep apnea. These devices are custom-made by dentists or orthodontists and are designed to be worn during sleep. They work by repositioning the jaw and tongue to help keep the airway open and prevent breathing obstructions.
There are several types of dental devices available, and the choice depends on the individual’s specific needs and preferences. One common type is a mandibular repositioning device (MRD), which resembles a sports mouthguard. This device helps to move the lower jaw slightly forward to increase the space at the back of the throat and improve airflow.
Another type of dental device is a tongue-retaining device (TRD). This device holds the tongue forward, preventing it from falling back and blocking the airway. It may be a suitable option for individuals with tongue-based obstructions.
Dental devices offer several advantages for individuals with sleep apnea. They are portable, easy to use, and generally well-tolerated. Unlike continuous positive airway pressure (CPAP) machines, dental devices are silent, making them more comfortable for both the user and their sleep partner. They are also convenient for travel and do not require a power source.
However, it is important to note that dental devices are not suitable for everyone with sleep apnea. They are typically recommended for individuals with mild to moderate obstructive sleep apnea or those who are unable to tolerate CPAP therapy. People with severe sleep apnea may require more intensive treatments.
To obtain a dental device, a thorough evaluation by a dentist or orthodontist is necessary. They will examine the individual’s teeth, jaw, and airway to determine the best course of action. The dentist will take impressions of the teeth and create a custom-fit device tailored to the individual’s mouth.
Regular follow-up appointments are crucial to assess the effectiveness of the dental device and make any necessary adjustments. These devices may require periodic replacement due to normal wear and tear.
It is important to highlight that dental devices should be used under the guidance of a qualified healthcare professional. They should only be obtained through reputable providers who specialize in sleep apnea and oral appliance therapy to ensure safety and efficacy.
Dental devices can be an effective treatment option for individuals with mild to moderate obstructive sleep apnea or those who cannot tolerate CPAP therapy. These custom-made devices help to reposition the jaw and tongue, keeping the airway open during sleep. However, it is essential to consult with a healthcare professional to determine the most suitable device and ensure proper fitting and ongoing care.
4. Surgery
Surgery is a treatment option for sleep apnea that is usually considered when other interventions have proven ineffective or if there is a physical abnormality that may be causing the obstruction. Surgical procedures aim to correct the structural issues in the airway that contribute to sleep apnea.
One common surgical procedure for sleep apnea is uvulopalatopharyngoplasty (UPPP). This procedure involves removing excess tissue from the throat, such as the uvula, tonsils, and part of the soft palate, to widen the airway. UPPP can be effective in reducing or eliminating obstructive sleep apnea in some individuals.
Another surgical option is genioglossus advancement (GA). This procedure involves repositioning and advancing the tongue muscle forward to create more space in the back of the throat. By doing so, it helps to prevent the tongue from collapsing and blocking the airway during sleep.
Maxillomandibular advancement (MMA) is a more complex surgical procedure that involves repositioning the upper and lower jaws forward. This helps to expand the space behind the tongue and soft palate, thus reducing the risk of airway obstruction.
In some cases, surgical intervention may also involve removing nasal obstructions, such as polyps or deviated septum, to improve nasal airflow. This can be done through procedures like septoplasty or turbinate reduction.
It is important to note that surgery is not suitable for everyone with sleep apnea. The decision to undergo surgery should be made in consultation with a medical professional, taking into consideration the severity of the sleep apnea, the potential risks and benefits of the procedure, and individual factors.
Surgery for sleep apnea may have risks and complications, including swelling, bleeding, infection, or changes in the voice. It is essential to follow the post-operative instructions provided by the surgeon and attend any necessary follow-up appointments to ensure proper healing and success of the procedure.
While surgery can be an effective treatment option for some individuals with sleep apnea, it is typically considered when other non-invasive methods have not provided satisfactory results. It is always recommended to explore and exhaust other treatment options before considering surgical intervention.
5. Expiratory Positive Airway Pressure (EPAP)
Expiratory Positive Airway Pressure (EPAP) is a treatment option for sleep apnea that can be used as an alternative to Continuous Positive Airway Pressure (CPAP) therapy. It is a non-invasive method that helps to keep the upper airway open during sleep, allowing for uninterrupted breathing.
EPAP works by utilizing small, adhesive valves or disks that are placed over the nostrils. These valves create an increased pressure in the airway when a person exhales, helping to keep the airway from collapsing or being obstructed. This mechanism is known as expiratory positive pressure.
One of the advantages of EPAP is its simplicity and ease of use compared to other treatment options. There is no need for a machine or external device, making it a more convenient choice for individuals who find CPAP machines cumbersome or uncomfortable. EPAP devices are small and portable, allowing for easy travel and use in various sleeping positions.
EPAP is typically recommended for individuals with mild to moderate obstructive sleep apnea or those who have difficulty tolerating CPAP therapy. It can also be used as a temporary alternative for CPAP users who may need to temporarily discontinue CPAP treatment due to travel or other circumstances.
While EPAP can be effective for many individuals, it may not be suitable for everyone. Some individuals may experience nasal congestion or discomfort with the adhesive valves. It is essential to consult with a healthcare professional to determine if EPAP is a suitable treatment option for your specific condition.
Expiratory Positive Airway Pressure (EPAP) is a non-invasive treatment option for sleep apnea that utilizes adhesive valves or disks to maintain an open airway during sleep. It offers a simple and portable alternative to CPAP therapy and can be beneficial for individuals with mild to moderate obstructive sleep apnea. However, it is important to consult with a healthcare professional to determine the most appropriate treatment approach for your specific needs and condition.
Managing Sleep Apnea
Managing sleep apnea involves implementing various strategies to improve the quality of sleep and minimize the symptoms associated with the condition. One effective method is adjusting sleep positioning. Sleeping on the side rather than the back can help keep the airways open and reduce the likelihood of obstruction. Additionally, weight management plays a crucial role in managing sleep apnea, as excess weight can contribute to airway blockage. Engaging in regular exercise not only helps in weight management but also promotes overall respiratory health. It is also important to avoid the consumption of alcohol and sedatives, as they can relax the throat muscles and exacerbate the symptoms of sleep apnea. Lastly, maintaining a consistent sleep schedule ensures adequate rest and proper sleep hygiene. By incorporating these strategies into daily routines, individuals with sleep apnea can effectively manage their condition and improve their sleep quality and overall well-being.
1. Sleep Positioning
Sleep positioning can play a significant role in managing sleep apnea symptoms, particularly for those with mild to moderate cases of obstructive sleep apnea (OSA). By adjusting the sleeping position, individuals can alleviate the obstruction in their airways and improve the flow of oxygen during sleep.
One of the recommended sleep positions for individuals with sleep apnea is sleeping on the side. Side sleeping helps keep the airway open and reduces the chances of the tongue or soft tissues blocking the throat. It is advisable to sleep on the left side as it can prevent acid reflux, which can aggravate sleep apnea symptoms.
In contrast, sleeping on the back, also known as the supine position, can worsen sleep apnea symptoms. This position allows the tongue and soft tissues to fall to the back of the throat, obstructing the airway and leading to disruptions in breathing. To encourage side sleeping, individuals can try using pillows or wedges to provide support and help maintain the proper sleeping position throughout the night.
Additionally, elevating the upper body can be beneficial for individuals with sleep apnea. This can be achieved by sleeping on an adjustable bed or by using extra pillows to prop up the upper body. Elevating the head and chest helps to alleviate the pressure on the airway and promotes better breathing during sleep.
It is important to note that while sleep positioning can be helpful, it may not completely eliminate sleep apnea symptoms or replace other treatment options. It is recommended to consult with a healthcare professional to determine the most appropriate treatment plan for managing sleep apnea. By incorporating sleep positioning techniques and following a comprehensive treatment approach, individuals with sleep apnea can improve the quality of their sleep and overall well-being.
2. Weight Management
Weight management plays a crucial role in managing sleep apnea. Excess weight and obesity are significant risk factors for the development and worsening of sleep apnea. When a person is overweight, excess fat can accumulate in the neck area, which can contribute to the narrowing of the airway during sleep. This narrowing can lead to more frequent occurrences of apneas.
Losing weight can help reduce the severity of sleep apnea and improve symptoms. Even a modest weight loss of around 10% can make a significant difference. It can lead to a decrease in the amount of fat surrounding the airway, allowing for better airflow during sleep.
To achieve weight loss and maintain a healthy weight, a combination of a balanced diet and regular exercise is essential. A diet rich in fruits, vegetables, lean proteins, and whole grains can help in managing weight. It is important to avoid or limit foods high in saturated fats, sugars, and processed carbohydrates. Portion control and mindful eating can also contribute to weight management.
Incorporating regular exercise into daily routine is another vital aspect of weight management. Engaging in moderate aerobic activities such as walking, swimming, or cycling can aid in weight loss and improve overall fitness. Additionally, strength training exercises can help build muscle, which in turn can increase metabolism and assist in weight maintenance.
It is important to note that weight management alone may not completely eliminate sleep apnea, especially if other factors such as structural abnormalities or genetics are involved. However, it can significantly improve symptoms and reduce the overall severity of the condition. It is advisable for individuals with sleep apnea to consult with healthcare professionals or registered dietitians to develop personalized weight management plans.
3. Regular Exercise
Regular exercise is an important component of managing sleep apnea. Engaging in physical activity on a regular basis can help improve overall sleep quality and reduce the severity of sleep apnea symptoms. Exercise can contribute to weight loss and help maintain a healthy body weight, which is especially beneficial for individuals with obstructive sleep apnea (OSA) as excess weight can contribute to airway blockage.
When it comes to exercise, there are a variety of options to choose from. Aerobic exercises such as walking, jogging, swimming, or cycling are great options for improving cardiovascular health and promoting weight loss. Strength training exercises, like weightlifting or resistance band exercises, can help tone muscles and improve muscle function, including the muscles in the throat that control breathing.
Ideally, individuals with sleep apnea should aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week, according to the American Heart Association. It is important to start slowly and gradually increase the intensity and duration of workouts to prevent overexertion and maintain consistency.
In addition to its direct benefits for sleep apnea, exercise also promotes better sleep by reducing stress and anxiety, enhancing mood, and improving overall sleep-wake regulation. However, it is important to avoid exercising too close to bedtime, as the increase in body temperature and heart rate can interfere with falling asleep.
If you haven’t been active for a while or have any health concerns, it is recommended to consult with a healthcare professional before starting an exercise program. They can provide guidance on the most suitable exercises for you and any precautions you may need to take.
So, consider incorporating regular exercise into your daily routine to manage sleep apnea effectively. Not only will it have a positive impact on your sleep, but it will also contribute to your overall well-being. Remember to listen to your body, stay consistent, and enjoy the benefits of an active lifestyle.
4. Avoiding Alcohol and Sedatives
4. Avoiding Alcohol and Sedatives
One important aspect of managing sleep apnea is making lifestyle changes that can promote better sleep. In particular, individuals with sleep apnea should avoid consuming alcohol and sedatives, as they can worsen the symptoms of the condition. Here are some key points to keep in mind:
– Alcohol: Consumption of alcohol before bedtime can relax the muscles in the throat, exacerbating the obstruction of the airway that is already a characteristic of sleep apnea. It can also disrupt the sleep cycle, leading to more frequent interruptions in breathing. It is best to avoid drinking alcohol, especially in the evening or close to bedtime. If you do choose to drink, moderate your alcohol intake and try to have your last drink several hours before going to bed.
– Sedatives: Similarly to alcohol, sedatives such as tranquilizers, sleeping pills, and certain types of medication can relax the airway muscles and interfere with normal breathing patterns. They can also suppress the central nervous system, which can further contribute to respiratory pauses during sleep. If you are taking any medications that have sedative effects, discuss with your healthcare provider to explore alternative options that may be less likely to affect your sleep apnea.
By avoiding alcohol and sedatives, individuals with sleep apnea can reduce the likelihood of experiencing symptoms and improve the quality of their sleep. It is important to note, however, that lifestyle changes should be implemented in conjunction with other recommended treatment options for sleep apnea, such as CPAP therapy or dental devices. Working closely with a healthcare professional can help determine the most appropriate course of action for managing your sleep apnea effectively.
5. Keeping a Sleep Schedule
Keeping a consistent sleep schedule is vital for individuals with sleep apnea to maintain a healthy sleep pattern. Here are some key points to consider when establishing and sticking to a sleep schedule:
1. Set a Regular Bedtime: Determine a specific time to go to bed each night and make an effort to stick to it. This helps regulate your body’s internal clock and promotes better sleep quality.
2. Wake Up at the Same Time: Just as it’s important to establish a regular bedtime, it’s equally important to wake up at the same time every morning. This helps train your body to develop a consistent sleep-wake cycle.
3. Avoid Napping: If possible, try to eliminate or limit daytime napping. Napping can disrupt your sleep schedule and make it more difficult to fall asleep at night. If you must nap, keep it short and before 3 PM.
4. Create a Bedtime Routine: Develop a relaxing routine before bed to signal to your body that it’s time to wind down. This could include activities such as reading a book, taking a warm bath, or practicing relaxation techniques like deep breathing or meditation.
5. Avoid Stimulants: Limit the consumption of stimulants like caffeine and nicotine, especially in the afternoon and evening. These substances can interfere with sleep and make it harder to stick to a consistent sleep schedule.
6. Create a Restful Sleep Environment: Make sure your bedroom is conducive to sleep. Keep the room dark, quiet, and at a comfortable temperature. Consider using earplugs, eye masks, or white noise machines if necessary.
7. Avoid Electronic Devices: The blue light emitted by electronic devices, such as smartphones and tablets, can interfere with your body’s production of melatonin, a hormone that promotes sleep. Avoid using these devices at least an hour before bedtime.
By implementing these strategies and maintaining a consistent sleep schedule, individuals with sleep apnea can improve their sleep quality, reduce daytime sleepiness, and enhance overall well-being. It’s important to remember that everyone’s sleep needs are different, so it may take some trial and error to find the schedule that works best for you.
Conclusion
In conclusion, sleep apnea is a serious sleep disorder that can have significant impacts on an individual’s health and well-being. Understanding the different types of sleep apnea, including obstructive sleep apnea (OSA), central sleep apnea (CSA), and complex sleep apnea syndrome (CompSAS), is crucial for diagnosis and treatment. Recognizing the signs and symptoms, such as loud snoring, frequent pauses in breathing, excessive daytime sleepiness, morning headaches, and difficulty concentrating, can aid in identifying sleep apnea and seeking proper medical attention. Diagnosis often involves medical history evaluations, physical examinations, and sleep studies (polysomnography). Once diagnosed, a range of treatment options is available, including lifestyle changes, continuous positive airway pressure (CPAP) therapy, dental devices, surgery, and expiratory positive airway pressure (EPAP) devices. Managing sleep apnea through sleep positioning, weight management, regular exercise, avoiding alcohol and sedatives, and maintaining a consistent sleep schedule can also improve symptoms and overall sleep quality. Sleep apnea should not be ignored, as it can lead to serious complications, but with proper diagnosis and treatment, individuals can experience significant improvements in their sleep and overall quality of life. So, it’s crucial to address any concerns related to sleep apnea and seek professional guidance for a healthier and more restful future.
Frequently Asked Questions
1. How common is sleep apnea?
Sleep apnea is quite common, affecting approximately 20% of adults worldwide. However, many cases go undiagnosed, so the actual prevalence could be higher.
2. What are the risk factors for developing sleep apnea?
Several factors can increase the risk of developing sleep apnea, including obesity, older age, family history, smoking, alcohol and sedative use, and certain anatomical factors like a thick neck or narrow airway.
3. Can children have sleep apnea?
Yes, children can also be affected by sleep apnea. It is most commonly seen in children who are overweight or have enlarged tonsils or adenoids.
4. How can I know if I have sleep apnea?
If you suspect you may have sleep apnea, it is essential to consult a healthcare professional. They can evaluate your symptoms, take your medical history, and recommend further testing, such as a sleep study, to diagnose sleep apnea.
5. Is sleep apnea treatable?
Yes, sleep apnea is treatable. There are various treatment options available, ranging from lifestyle changes to using specialized devices like continuous positive airway pressure (CPAP) machines.
6. Can untreated sleep apnea lead to other health problems?
Yes, untreated sleep apnea can lead to a variety of health problems, including high blood pressure, heart disease, stroke, diabetes, and an increased risk of accidents due to daytime sleepiness.
7. What lifestyle changes can help manage sleep apnea?
Lifestyle changes can play a significant role in managing sleep apnea. These include maintaining a healthy weight, exercising regularly, avoiding alcohol and sedatives, and establishing a consistent sleep schedule.
8. Is surgery a common treatment for sleep apnea?
Surgery is not the first-line treatment for sleep apnea. It is typically considered when other treatment options have been ineffective or in cases where there is a specific structural abnormality causing the obstruction.
9. Can sleep apnea go away on its own?
While weight loss and certain lifestyle changes may improve the symptoms of sleep apnea, the condition itself usually does not go away on its own. Prompt diagnosis and appropriate treatment are essential for managing sleep apnea effectively.
10. Can using a CPAP machine cure sleep apnea?
A continuous positive airway pressure (CPAP) machine is considered a highly effective treatment for sleep apnea. However, it does not cure the condition. The machine helps keep the airway open during sleep and effectively alleviates the symptoms of sleep apnea as long as it is used regularly.