Have you ever wondered what happens when your body moves on its own while you’re fast asleep? Sleepwalking is a fascinating phenomenon that has intrigued scientists for years. It’s a mysterious state where people engage in complex behaviors, like walking, talking, and even cooking, all while still asleep. While the exact science behind sleepwalking is not completely understood, researchers have made significant progress in unraveling its complexities. In this article, we will delve deeper into the causes, neurological explanations, risks, and management of sleepwalking. So, grab your pillow and get ready to explore the depths of human slumber.
Understanding Sleepwalking
Sleepwalking is a complex sleep disorder that occurs during the deepest stages of sleep. Sleepwalking, also known as somnambulism, is characterized by performing various activities while unconscious. The exact cause of sleepwalking remains uncertain, but it is believed to be influenced by a combination of genetic factors, medical conditions, and stress and anxiety. While sleepwalking can affect individuals of all ages, it is particularly prevalent in children, with studies suggesting that up to 17% of children between the ages of 4 and 12 experience sleepwalking episodes. Sleepwalking can be a perplexing phenomenon for both individuals experiencing it and their loved ones. Understanding the underlying factors contributing to sleepwalking is essential in order to effectively manage and prevent these episodes. To delve deeper into the causes of sleepwalking, click here.
Definition of Sleepwalking
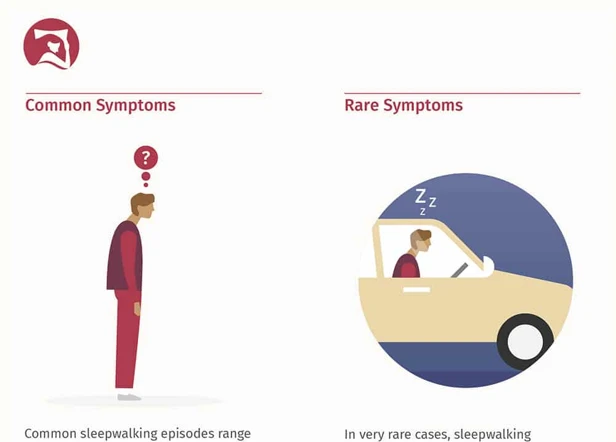
Sleepwalking, also known as somnambulism, is a parasomnia sleep disorder that involves performing complex behaviors while in a state of partial consciousness during deep sleep. Individuals who experience sleepwalking may engage in various activities such as walking, talking, eating, or even driving, all while appearing to be asleep. These episodes typically occur during the first few hours of sleep and can last for a few minutes to half an hour. The person may display a blank expression with glassy eyes, and their movements may be slow and uncoordinated. Although sleepwalkers may appear to be awake, they are not fully aware of their surroundings and often have no recollection of their actions upon awakening. It is important to note that sleepwalking is different from night terrors, which are characterized by episodes of fear, screaming, and intense agitation during sleep. To understand the intricate mechanisms of sleepwalking at a neuroscientific level, researchers have extensively studied the relationship between sleepwalking and the brain. Sleepwalking is a relatively common phenomenon in children, and parents should be aware of the potential signs and management strategies to ensure the safety and well-being of their child.
Prevalence of Sleepwalking
The prevalence of sleepwalking is a significant aspect to consider when examining this sleep disorder. Studies have indicated that sleepwalking is more common during childhood, with a peak occurrence between the ages of 4 and 12. It is estimated that up to 17% of children experience sleepwalking episodes at some point during their development. However, sleepwalking can also affect adults, although the occurrence tends to be less frequent. The prevalence of sleepwalking among adults varies, with estimates ranging from 1% to 5% of the population. It is important to note that these numbers are approximate, as sleepwalking often goes undiagnosed or unreported. Sleepwalking episodes can occur sporadically or in clusters, and they tend to be more prevalent in individuals who have a family history of sleepwalking. These statistics highlight the widespread nature of sleepwalking and emphasize the need for further research and understanding regarding its causes and management.
Causes of Sleepwalking

The causes of sleepwalking can vary and are often multifaceted. One possible factor that contributes to sleepwalking is genetic predisposition. Research suggests that if you have a family history of sleepwalking, you may be more likely to experience it yourself. Certain medical conditions such as sleep apnea, restless leg syndrome, and seizures have also been associated with sleepwalking episodes. Additionally, stress and anxiety can play a role in triggering sleepwalking episodes. People who experience high levels of stress or have anxiety disorders may be more prone to sleepwalking. It’s important to note that the specific causes of sleepwalking can vary from person to person, and further research is still being conducted to fully understand this complex sleep disorder.
Genetic Factors
Genetic factors play a significant role in the occurrence of sleepwalking. Research suggests that there is a genetic predisposition to sleepwalking, meaning that it can run in families. Multiple studies have found that individuals with a family history of sleepwalking are more likely to experience episodes themselves. This suggests that certain genes may be responsible for the development of sleepwalking. One study conducted on twins found a higher concordance rate for sleepwalking in identical twins compared to fraternal twins, further supporting the genetic link. Researchers have also identified specific gene variants that may be associated with an increased risk of sleepwalking. For example, a study published in the journal Sleep analyzed the DNA of sleepwalkers and found a variation in the CHRNA4 gene, which is involved in regulating brain activity during sleep. While more research is needed to fully understand the genetic mechanisms underlying sleepwalking, it is clear that genetics plays a significant role in its occurrence.
Medical Conditions
Medical conditions can play a significant role in the occurrence of sleepwalking episodes. Certain sleep disorders and medical conditions have been found to be associated with an increased likelihood of sleepwalking. One such condition is obstructive sleep apnea, which is characterized by repeated pauses in breathing during sleep. The fragmented and disrupted sleep patterns observed in individuals with sleep apnea can contribute to sleepwalking episodes. Another medical condition linked to sleepwalking is gastroesophageal reflux disease (GERD), which is characterized by the backward flow of stomach acid into the esophagus. The discomfort caused by GERD can disrupt sleep and potentially trigger sleepwalking episodes. Additionally, individuals with migraine headaches may experience sleepwalking as a comorbidity. The exact mechanisms underlying the connection between migraines and sleepwalking are not yet fully understood, but it is believed that disruptions in the sleep-wake cycle and abnormal brain activity may contribute to both conditions. It is essential for individuals experiencing sleepwalking episodes to consult with a healthcare professional to assess and manage any underlying medical conditions that may be contributing to their sleepwalking.
Stress and Anxiety
Stress and anxiety play a significant role in sleepwalking episodes. When individuals experience high levels of stress or anxiety, it can disrupt their sleep patterns and contribute to the occurrence of sleepwalking. Psychological factors such as work-related stress, relationship problems, traumatic events, or unresolved emotional issues can trigger sleepwalking episodes. Stress and anxiety can disrupt the natural sleep cycle, causing individuals to transition between sleep stages in an irregular manner. This disruption can potentially lead to a state of partial arousal, where the individual is neither fully asleep nor awake, making them more susceptible to sleepwalking. Additionally, elevated levels of stress hormones, such as cortisol, can influence the brain’s activity and interfere with the regulation of sleep. It is important to address and manage stress and anxiety through stress reduction techniques such as relaxation exercises, meditation, counseling, or therapy to minimize the frequency and intensity of sleepwalking episodes. By addressing these emotional factors, individuals may find relief from sleepwalking and improve the overall quality of their sleep.
Neurological Explanations
When it comes to understanding the neurological explanations for sleepwalking, scientists have made significant progress in unraveling the mysteries behind this peculiar phenomenon. Brain activity plays a crucial role in sleepwalking episodes. Research suggests that sleepwalkers exhibit abnormal brain patterns during the deepest stages of sleep, known as slow-wave sleep. During these stages, certain parts of the brain responsible for regulating movement, such as the frontal cortex, may remain partially awake while the rest of the brain remains asleep. This mismatch in brain activity results in the execution of complex behaviors during sleep. Additionally, the impact of sleep stages and the interaction between different neurotransmitters further contribute to the occurrence of sleepwalking. To learn more about the intricate relationship between the brain and sleepwalking, visit here.
Role of Brain Activity
The Role of Brain Activity in sleepwalking is a crucial aspect to understand this intriguing phenomenon. Research suggests that sleepwalking may be associated with certain abnormalities in brain activity during sleep. One particular area of interest is the interaction between the different stages of sleep, such as rapid eye movement (REM) sleep and non-rapid eye movement (NREM) sleep. During REM sleep, which is commonly associated with dreaming, the brain is highly active, and the muscles are mostly paralyzed to prevent acting out dreams. In contrast, during NREM sleep, the brain is in a resting state, with less muscle paralysis. It is believed that in sleepwalkers, there may be disruptions in the transition between these different sleep stages, leading to incomplete muscle paralysis during REM sleep and partial awakenings during NREM sleep. These disruptions can result in the individual engaging in physical activities while still asleep. This connection between brain activity, sleep stages, and sleepwalking is an ongoing area of research, and further studies are needed to gain a deeper understanding of the intricate mechanisms at play.
Impact of Sleep Stages
The impact of sleep stages on sleepwalking is a significant area of study. Sleep is divided into several stages, including non-rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep. NREM sleep is further divided into three stages:
- Stage N1: This is the transition stage between wakefulness and sleep. It is a light sleep stage, where the individual can be easily awakened.
- Stage N2: This is a deeper sleep stage characterized by a decrease in body temperature and heart rate. It is still considered light sleep, but the sleeper is less responsive to external stimuli.
- Stage N3: Also known as slow-wave sleep, this is the deepest stage of NREM sleep. It is difficult to wake the sleeper during this stage, and it is when most sleepwalking episodes occur.
During REM sleep, which is the stage associated with vivid dreaming, the body is typically paralyzed to prevent acting out dreams. However, in sleepwalkers, this muscle paralysis may not function properly, leading to the possibility of acting out dreams or engaging in sleepwalking behaviors.
The exact mechanisms by which sleep stages impact sleepwalking are not fully understood, but researchers believe that sleepwalking is more likely to occur during the transition from deep NREM sleep (stage N3) to lighter sleep stages (N2 or wakefulness). This transition period is known as sleep inertia and is thought to influence the occurrence of complex behaviors like sleepwalking.
Understanding the influence of sleep stages on sleepwalking is crucial for managing and preventing episodes. By identifying and addressing disruptions in sleep architecture, such as reducing arousals during the transition from deep sleep to wakefulness, individuals with sleepwalking tendencies can potentially reduce the frequency and intensity of their sleepwalking episodes.
Risks and Complications
Sleepwalking can pose certain risks and complications for individuals who experience episodes. One of the most concerning risks is injury and safety concerns. Sleepwalkers may engage in activities that put them at risk of accidents or falls, especially if they are not in a safe environment. It is not uncommon for sleepwalkers to trip, bump into objects, or even attempt to leave their homes, which can lead to serious injuries. Additionally, sleepwalking can have psychosocial impacts on individuals. The fear of sleepwalking episodes or the embarrassment that may arise from their behaviors can lead to anxiety, stress, and social withdrawal. It is crucial for sleepwalkers to adopt preventive measures and create a sleep-friendly environment to minimize these risks. Taking the necessary precautions can ensure the safety and well-being of sleepwalkers.
Injury and Safety Concerns
When it comes to sleepwalking, safety is a significant concern. Sleepwalkers are often at risk of sustaining injuries due to their unawareness and disorientation during episodes. Some potential hazards include tripping over objects, falling down stairs, or encountering obstacles in the surroundings. To mitigate the risk of injury, it is crucial to create a safe sleep environment for sleepwalkers. This can involve removing clutter, securing doors and windows, and installing safety gates to prevent access to potentially dangerous areas. Placing padding or cushions around sharp corners or edges can provide extra protection in case of accidental bumps or falls. It is also advisable to keep potential hazards out of the sleepwalker’s reach, such as sharp objects or harmful substances. Taking preventive measures and ensuring a safe sleeping environment is essential to minimize the risk of injury and ensure the well-being of individuals experiencing sleepwalking episodes.
Psychosocial Impact
The psychosocial impact of sleepwalking can be significant, affecting individuals’ overall well-being and quality of life. For individuals who frequently experience sleepwalking episodes, it can lead to disturbances in their sleep patterns, resulting in chronic sleep deprivation. This lack of quality sleep can lead to daytime sleepiness, decreased cognitive function, and mood disturbances.
The unpredictable nature of sleepwalking can cause distress and anxiety for the individual and their loved ones. It can create a constant worry about potential injuries or accidents that may occur during sleepwalking episodes. This anxiety can impact relationships and family dynamics, as sleepwalking may require extra precautions and adjustments to the sleep environment to minimize risks.
Additionally, the psychosocial impact of sleepwalking extends beyond the individual experiencing the episodes. It can present challenges in shared living situations, such as roommates or partners who may feel disturbed or concerned by the unusual behaviors and sleep disturbances associated with sleepwalking.
It is crucial for individuals experiencing sleepwalking to seek support from healthcare professionals, therapists, or support groups. These resources can provide guidance on coping strategies and help individuals and their loved ones navigate the psychosocial challenges associated with sleepwalking. By addressing the psychosocial impact, individuals can develop strategies to manage anxiety, improve sleep quality, and cultivate a supportive environment that promotes overall well-being.
Diagnostic Process

The diagnostic process for sleepwalking involves a comprehensive evaluation to identify the underlying causes and rule out any other sleep disorders. A medical evaluation is typically the first step, where the individual’s medical history, sleep patterns, and any potential factors contributing to sleepwalking are assessed. Additionally, sleep studies may be conducted to monitor brain activity, muscle movements, and other physiological changes during sleep. These studies, such as polysomnography and multiple sleep latency tests, provide valuable insights into the sleep architecture and can help diagnose sleep disorders like sleepwalking. The combination of a thorough medical evaluation and detailed sleep studies enables healthcare professionals to accurately diagnose sleepwalking and develop tailored treatment plans.
Medical Evaluation
During the diagnostic process of sleepwalking, a medical evaluation plays a crucial role in identifying any underlying medical conditions or medications that may contribute to the episodes. The medical evaluation typically involves the following steps:
- Medical History: The healthcare provider will ask detailed questions about the individual’s sleep patterns, the frequency and duration of sleepwalking episodes, any associated symptoms, and any relevant medical conditions or medications.
- Physical Examination: A thorough physical examination is performed to check for any signs of underlying medical conditions or neurological abnormalities that could be contributing to sleepwalking.
- Review of Medications: The healthcare provider will review the individual’s current medications to determine if any medications may be triggering or exacerbating sleepwalking episodes. Medications such as sedatives or certain antidepressants can increase the risk of sleepwalking.
- Screening for Sleep Disorders: As sleepwalking can be associated with other sleep disorders, such as sleep apnea or restless leg syndrome, the healthcare provider may recommend further evaluation or refer the individual for a sleep study to rule out other conditions.
- Collaboration with Specialists: In some cases, the healthcare provider may collaborate with specialists, such as neurologists or sleep medicine experts, to further assess and evaluate the individual’s sleepwalking episodes.
The medical evaluation helps in determining any underlying factors contributing to sleepwalking and guides the healthcare provider in developing an appropriate treatment plan. It is important to consult with a healthcare professional for a comprehensive evaluation if you or someone you know experiences sleepwalking episodes.
Sleep Studies
Sleep studies, also known as polysomnography, play a crucial role in diagnosing and understanding sleepwalking. These studies involve monitoring and recording various physiological parameters while an individual is asleep. The goal of sleep studies is to gather information about sleep architecture, brain activity, breathing patterns, and body movements during sleep. In the context of sleepwalking, sleep studies can provide valuable insights into the specific sleep stage during which sleepwalking episodes occur. Researchers have found that sleepwalking tends to happen during the deep stage of non-rapid eye movement (NREM) sleep. During sleep studies, electrodes are attached to the individual’s scalp, face, chest, and legs to measure brain waves, eye movements, muscle activity, heart rate, and respiration. This data helps identify the specific sleep stage when sleepwalking occurs and assists in ruling out other potential sleep disorders that may mimic sleepwalking behaviors. Sleep studies, conducted in specialized sleep laboratories, provide objective data to aid in accurate diagnosis and treatment planning for individuals with sleepwalking episodes.
Prevention and Management
Prevention and management strategies play a crucial role in minimizing the frequency and impact of sleepwalking episodes. Creating a sleep-friendly environment is essential for promoting healthy sleep patterns and reducing the likelihood of sleepwalking. This includes ensuring a comfortable and safe sleep environment, maintaining a regular sleep schedule, and implementing relaxation techniques before bedtime to reduce stress and anxiety. Additionally, implementing stress reduction techniques such as exercise, meditation, and deep breathing exercises can help manage underlying stressors that may contribute to sleepwalking. In some cases, sleep medications may be prescribed by a healthcare professional to regulate sleep and reduce the occurrence of sleepwalking episodes. It is important to consult a healthcare professional for personalized guidance on the prevention and management of sleepwalking.
Creating a Sleep-Friendly Environment
Creating a sleep-friendly environment is crucial for individuals who experience sleepwalking episodes. Here are some effective strategies to promote a healthy and restful sleep environment:
1. Remove Potential Hazards: Clear the bedroom of any sharp objects, furniture with sharp edges, or clutter that can increase the risk of injury during a sleepwalking episode.
2. Secure Doors and Windows: Ensure that all doors and windows are securely locked to prevent sleepwalkers from wandering outside or accessing any potentially dangerous areas.
3. Install Safety Gates: If sleepwalking is more common in children or if it occurs frequently, installing safety gates at the top of staircases can prevent falls and injuries.
4. Improve Lighting: Use nightlights in hallways and bathrooms to provide adequate lighting for sleepwalkers, reducing the risk of accidents.
5. Implement Alarms: Consider installing alarms or bells on doors and windows, which can help alert family members or caregivers when a sleepwalker is on the move.
6. Establish a Consistent Routine: Maintain a regular sleep schedule to promote better overall sleep quality, reducing the likelihood of disruptive sleepwalking episodes.
7. Reduce Noise and Distractions: Keep the sleep environment quiet, calm, and free of distractions that may disrupt sleep and potentially trigger sleepwalking behaviors.
Creating a sleep-friendly environment plays a vital role in mitigating the risks associated with sleepwalking and ensuring the safety of individuals who experience these episodes. By implementing these strategies, sleepwalkers can minimize the chances of injury and enjoy a more peaceful and uninterrupted night’s sleep.
Stress Reduction Techniques
Stress can be a significant contributing factor to sleepwalking episodes. Implementing effective stress reduction techniques can play a crucial role in managing and preventing sleepwalking episodes. Here are some stress reduction techniques that can help promote relaxation and improve sleep quality:
- Regular exercise: Engaging in regular physical activity can reduce stress levels and promote better sleep. Exercise stimulates the production of endorphins, which are natural mood boosters and stress relievers. Aim for at least 30 minutes of moderate-intensity exercise every day.
- Deep breathing exercises: Deep breathing exercises, such as diaphragmatic breathing or belly breathing, can activate the body’s relaxation response and help reduce stress and anxiety. Find a quiet place, inhale deeply through your nose, hold the breath for a few seconds, and exhale slowly through your mouth.
- Meditation: Practicing meditation or mindfulness techniques can calm the mind, reduce stress, and promote better sleep. Find a comfortable position, focus on your breath or a specific mantra, and allow any intrusive thoughts to pass by without judgment.
- Yoga: Yoga combines physical postures, breathing exercises, and meditation. Regular yoga practice can reduce stress and promote a sense of relaxation. Choose gentle or restorative yoga poses that are suitable for your fitness level.
- Aromatherapy: Certain scents, such as lavender, chamomile, or ylang-ylang, are known for their calming effects. Experiment with essential oils or use a diffuser in your bedroom to create a relaxing sleep environment.
By incorporating these stress reduction techniques into your daily routine, you can create a more relaxed and peaceful mindset, minimizing the likelihood of experiencing sleepwalking episodes. Remember, stress management is a personal journey, so explore different techniques and find what works best for you.
Sleep Medications
Sleep medications are sometimes prescribed as a treatment option for individuals with severe and disruptive sleepwalking episodes. These medications work to regulate sleep patterns and promote deeper, more restful sleep. Here are some commonly prescribed sleep medications that can help manage sleepwalking:
- Sedatives: Sedatives, such as benzodiazepines, are commonly used to treat sleep disorders, including sleepwalking. These medications work by calming the central nervous system and inducing a state of relaxation, which can help reduce sleepwalking episodes.
- Antidepressants: Certain antidepressant medications, such as selective serotonin reuptake inhibitors (SSRIs), have been found to be effective in reducing sleepwalking episodes. These medications help regulate serotonin levels in the brain, which can contribute to improved sleep quality and decreased sleepwalking tendencies.
- Anticonvulsants: Anticonvulsant medications, typically used to treat epilepsy, have also shown promise in managing sleepwalking. These medications work by stabilizing brain activity, which can help prevent abnormal movements during sleep.
It’s important to note that sleep medications should only be used under the guidance and supervision of a healthcare professional. They may have potential side effects or interactions with other medications, so it’s crucial to discuss the risks and benefits with a doctor before starting any sleep medication regimen. Sleep medications should be used as a short-term solution to manage sleepwalking, while underlying causes and lifestyle factors are addressed through behavioral interventions and other treatment options.
Treatment Options
When it comes to treating sleepwalking, there are various options available to individuals seeking relief from this peculiar disorder. Two primary treatment approaches include behavioral therapy and the use of medications. Behavioral therapy aims to identify and address underlying causes and triggers through techniques such as hypnosis, relaxation training, and sleep schedule adjustments. This approach focuses on modifying behavior and promoting healthy sleep patterns. On the other hand, medications may be prescribed to help manage sleepwalking episodes, particularly if they are frequent and disruptive. These medications may include benzodiazepines, antidepressants, or even melatonin supplements, depending on the individual’s specific needs and medical history. It is important to consult with a healthcare professional to determine the most suitable treatment plan for addressing sleepwalking.
Behavioral Therapy
Behavioral therapy is a commonly recommended treatment option for individuals experiencing sleepwalking episodes. This form of therapy focuses on modifying behaviors and establishing healthy sleep habits to minimize the occurrence of sleepwalking. The main goal of behavioral therapy is to address any underlying issues or triggers that may contribute to sleepwalking and provide strategies to prevent and manage episodes.
One of the key components of behavioral therapy for sleepwalking is creating a consistent and relaxing bedtime routine. This includes establishing a regular sleep schedule and engaging in relaxing activities before bed, such as reading a book or taking a warm bath. By following a consistent routine, individuals can signal to their body that it is time to wind down and prepare for sleep, reducing the likelihood of sleepwalking.
Another aspect of behavioral therapy is implementing safety measures in the sleep environment. This may involve removing any potential hazards or obstacles that could lead to injury during a sleepwalking episode. It is important to ensure that windows and doors are securely locked and that furniture is arranged in a way that minimizes the risk of tripping or falling.
Behavioral therapy may include the use of relaxation techniques and stress reduction strategies. Techniques such as deep breathing exercises, meditation, and progressive muscle relaxation can help individuals relax and reduce any anxiety or stress that may contribute to sleepwalking. Managing stress levels during the day through healthy coping mechanisms can also help improve overall sleep quality and reduce the likelihood of sleepwalking episodes.
Behavioral therapy for sleepwalking often involves working closely with a qualified therapist or sleep specialist who can provide guidance, support, and personalized strategies. These professionals can help individuals identify their specific triggers, develop coping mechanisms, and monitor progress over time.
It is important to note that behavioral therapy may take time and consistency to see significant improvements. Patience and dedication to implementing recommended strategies are crucial for the success of this form of treatment. If behavioral therapy alone does not effectively manage sleepwalking episodes, a combination of therapy and medication may be considered under the guidance of a healthcare professional.
Medications
When it comes to managing sleepwalking, medications can play a role in reducing the frequency and severity of episodes. However, it’s important to note that medication should only be prescribed by a healthcare professional after a thorough evaluation. Here are some common medications that may be used in the treatment of sleepwalking:
- Sedatives: Sedatives such as benzodiazepines can be prescribed to help promote deeper and more restful sleep, which may reduce the likelihood of sleepwalking episodes.
- Antidepressants: In some cases, certain antidepressant medications may be prescribed to help manage underlying anxiety or stress that could be contributing to sleepwalking.
- Anticonvulsants: Anticonvulsant medications, typically used to manage seizures, may also be effective in reducing the occurrence of sleepwalking episodes.
It’s important to remember that while medications can be helpful, they may also come with potential side effects. Close monitoring and regular follow-up with a healthcare professional are crucial to ensure the most appropriate medication is being used and to assess any possible adverse effects. Medication treatment should always be combined with other management strategies, such as creating a sleep-friendly environment and stress reduction techniques, to maximize the effectiveness of the overall treatment plan.
Coping Strategies for Sleepwalkers
When it comes to coping with sleepwalking, there are several strategies that can help minimize the risks and ensure safety for sleepwalkers. Creating a sleep-friendly environment is crucial, as it involves removing any obstacles or hazards that could potentially harm the sleepwalker during their nocturnal wanderings. This includes keeping the bedroom clutter-free, installing safety gates, and locking windows and doors. Additionally, utilizing stress reduction techniques can be beneficial, such as practicing relaxation exercises or engaging in activities that promote calmness before bedtime. Sleepwalking alarms have also proven to be effective in alerting both the sleepwalker and their caregivers when a sleepwalking episode occurs. Lastly, providing strong caregiver support is essential in ensuring the well-being of sleepwalkers. Informing family members and close friends about the condition can help create a supportive network that can offer assistance and guidance when needed. By implementing these coping strategies, sleepwalkers can navigate their nightly adventures with improved safety and peace of mind.
Safe Sleep Practices
Safe sleep practices are crucial for individuals who experience sleepwalking episodes. By creating a sleep-friendly environment, it is possible to minimize the risks and ensure the safety of sleepwalkers. Here are some safe sleep practices to consider:
- Create a Clutter-Free Bedroom: Remove any obstacles, such as furniture or loose objects, from the sleepwalker’s bedroom to reduce the chances of tripping or injury.
- Secure Windows and Doors: Install locks or alarms on windows and doors to prevent the sleepwalker from wandering outside or accessing potentially dangerous areas.
- Install Safety Gates: If the sleepwalker is prone to leaving their room, consider installing safety gates at the entrance of their bedroom or stairways to prevent falls or accidents.
- Use Padding: Place a soft mat or cushion on the floor near the bed to cushion any falls that may occur during sleepwalking episodes.
- Lock Medications and Household Chemicals: Keep all medications and household chemicals locked away to prevent accidental ingestion or harm during sleepwalking incidents.
- Sleep on Ground Floor: If possible, have the sleepwalker sleep on the ground floor to minimize the risk of falls on stairs or from higher levels.
- Remove Sharp Objects: Keep sharp objects like knives, scissors, or tools out of reach to avoid potential injuries during sleepwalking episodes.
- Use Nightlights: Install nightlights in hallways or the sleepwalker’s bedroom to provide gentle illumination, making it easier for them to navigate safely.
- Consider Bed Alarms: Bed alarms or motion sensors can alert caregivers when the sleepwalker leaves their bed, allowing them to assist and guide them back to safety.
- Regular Exercise: Engage in regular exercise during the day, which can improve overall sleep quality and potentially reduce sleepwalking episodes.
Following these safe sleep practices can significantly reduce the risks associated with sleepwalking and create a secure sleeping environment for the sleepwalker.
Sleepwalking Alarms
Sleepwalking alarms are devices designed to detect and alert individuals when they are sleepwalking. These alarms can be worn as wristbands, anklets, or attached to clothing, and they work by sensing movement and triggering an alarm to wake up the sleepwalker or alert their caregiver. The alarms can be set at various sensitivity levels to detect different levels of movement. When the device detects significant movement, it emits a loud sound, vibration, or both, to awaken the sleepwalker and prevent them from potentially harming themselves or others. Sleepwalking alarms are particularly useful for individuals who sleepwalk frequently or have a history of engaging in complex sleepwalking behaviors. By using sleepwalking alarms, individuals and their caregivers can have peace of mind knowing that they will be alerted if a sleepwalking episode occurs, allowing for quick intervention and safety precautions. It is important to note that sleepwalking alarms should be used in conjunction with other safety measures, such as securing windows and stair gates, to further minimize the risk of injury.
Caregiver Support
When it comes to sleepwalking, caregiver support plays a crucial role in ensuring the safety and well-being of individuals who experience sleepwalking episodes. Here are some important ways caregivers can provide support:
1. Understanding and Education:
– Caregivers should take the time to educate themselves about sleepwalking, including its causes, triggers, and potential risks.
– By understanding the nature of sleepwalking, caregivers can better respond to episodes, ensuring the safety of the sleepwalker and others in the environment.
2. Creating a Safe Environment:
– Caregivers should take proactive measures to create a sleep-friendly environment by reducing potential hazards in the sleepwalker’s surroundings.
– Removing sharp objects, securing windows and doors, and installing safety gates can help prevent injuries during sleepwalking episodes.
3. Nighttime Supervision:
– For individuals who experience frequent or severe sleepwalking episodes, caregivers may consider nighttime supervision to ensure their safety.
– This can involve having a caregiver or family member sleep in the same room or using video monitoring systems to keep an eye on the sleepwalker.
4. Sleep Routine and Stress Reduction:
– Establishing a consistent sleep routine can be beneficial in managing sleepwalking episodes.
– Caregivers can help create a relaxing bedtime routine, incorporating activities that promote relaxation and stress reduction, such as reading or listening to calming music.
5. Communication and Support:
– Open communication between caregivers, sleepwalkers, and healthcare professionals is essential for effective management.
– Caregivers can offer emotional support to sleepwalkers, reassuring them and addressing any concerns they may have about their condition.
Caregiver support is vital in not only ensuring the safety of sleepwalkers but also providing them with the necessary understanding and resources to cope with their condition. By implementing these strategies, caregivers can play a pivotal role in the management and well-being of individuals who experience sleepwalking episodes.
Conclusion
In conclusion, sleepwalking is a complex sleep disorder that continues to puzzle scientists and researchers. While the exact science behind sleepwalking is not completely understood, several factors contribute to its occurrence. Genetic factors, medical conditions, and stress and anxiety are all believed to play a role in sleepwalking. Understanding the neurological explanations behind sleepwalking, such as the role of brain activity and the impact of different sleep stages, has provided valuable insights into this intriguing phenomenon. Sleepwalking can pose risks and complications, including the potential for injuries and psychosocial impact. Diagnosis of sleepwalking involves medical evaluation, as well as sleep studies to gather further information about sleep patterns and behaviors. Prevention and management strategies focus on creating a sleep-friendly environment, stress reduction techniques, and, in some cases, the use of sleep medications. Treatment options for sleepwalking include behavioral therapy and medication. Coping strategies, such as practicing safe sleep practices and the use of sleepwalking alarms, can also be helpful for sleepwalkers. Overall, further research and understanding of sleepwalking are needed to develop more effective approaches to manage and prevent this intriguing sleep disorder.
Frequently Asked Questions
1. Can someone really cook or perform complex tasks while sleepwalking?
Yes, it is possible for individuals to engage in complex behaviors like cooking or even driving while sleepwalking. The brain can orchestrate these activities on autopilot, relying on learned motor skills and muscle memory.
2. Is sleepwalking a dangerous condition?
Sleepwalking can pose certain risks, especially if the sleepwalker encounters hazards or engages in activities that may result in injury. It is important to create a safe sleeping environment and take precautions to minimize potential dangers.
3. Can stress and anxiety trigger sleepwalking episodes?
Yes, stress and anxiety can contribute to the onset of sleepwalking. Heightened emotional states can disrupt normal sleep patterns and increase the likelihood of experiencing sleepwalking episodes.
4. Are there any long-term complications associated with sleepwalking?
While sleepwalking itself may not lead to long-term complications, it can cause sleep disruption and daytime fatigue, impacting overall quality of life. In rare cases, sleepwalking with harmful behavior may require intervention.
5. Can sleepwalking be inherited?
There is evidence to suggest that genetic factors play a role in sleepwalking. Individuals with a family history of sleepwalking have a higher likelihood of experiencing it themselves.
6. Is sleepwalking more common in children or adults?
Sleepwalking is more prevalent in children, with studies indicating that up to 17% of children experience sleepwalking episodes. However, it can also occur in adults, although at a lower frequency.
7. Can medications cause sleepwalking?
Some medications, such as certain sedatives and sleep aids, have been associated with an increased risk of sleepwalking. It is important to consult with a healthcare professional about the potential side effects of medications.
8. How is sleepwalking diagnosed?
Sleepwalking is typically diagnosed through a combination of medical evaluation and sleep studies. These assessments help rule out underlying medical conditions and identify specific patterns of sleep behavior.
9. Can sleepwalking be prevented?
While it may not be possible to prevent sleepwalking entirely, certain measures can minimize the occurrence of episodes. Creating a sleep-friendly environment, managing stress, and maintaining consistent sleep schedules can be helpful in reducing sleepwalking incidents.
10. Are there any treatments available for sleepwalking?
Yes, there are treatments available for sleepwalking. Behavioral therapy, such as implementing relaxation techniques and establishing a consistent bedtime routine, can be effective. In some cases, medication may be prescribed to manage underlying conditions contributing to sleepwalking.