Sleepwalking, night terrors, and other parasomnias can be mysterious and perplexing phenomena, often leaving individuals and their loved ones searching for answers. One factor that has been increasingly linked to these sleep disorders is sleep apnea, a condition characterized by interruptions in breathing during sleep. While sleep apnea is typically associated with snoring and daytime fatigue, its connection to parasomnias is not widely known. This article explores the role of sleep apnea in sleepwalking and other parasomnias, delving into the mechanisms at play, the impact on sleep quality, and the potential risks involved. By understanding this link, individuals and healthcare professionals can better manage and treat parasomnias associated with sleep apnea, ultimately improving sleep and overall well-being.
Understanding Sleep Apnea

Sleep apnea is a sleep disorder characterized by frequent pauses in breathing during sleep. It can have various causes, including obesity, genetics, and anatomical factors. This condition affects a significant number of people worldwide, with estimates suggesting that up to 20% of adults may have some form of sleep apnea. The symptoms of sleep apnea can vary, but commonly include loud and chronic snoring, excessive daytime sleepiness, and morning headaches. Left untreated, sleep apnea can have serious health implications, such as an increased risk of cardiovascular disease and stroke. Diagnosis typically involves a sleep study conducted by a healthcare professional. Treatment options range from lifestyle changes, such as weight loss and avoiding alcohol, to the use of continuous positive airway pressure (CPAP) devices that help keep the airway open during sleep. Understanding the complexities of sleep apnea is crucial in recognizing its potential role in sleepwalking and other parasomnias. For more information on sleep apnea causes, symptoms, and treatments, you can refer to this comprehensive guide.
Definition and Causes
Sleep apnea is a sleep disorder that is characterized by recurring pauses in breathing during sleep. These pauses, known as apneas, can last for a few seconds to minutes and can occur multiple times throughout the night. Sleep apnea can be classified into three main types: obstructive sleep apnea (OSA), central sleep apnea (CSA), and complex sleep apnea syndrome (CSAS), which is a combination of both OSA and CSA. In OSA, the most common form of sleep apnea, the airway becomes partially or completely blocked, restricting airflow. This obstruction can be caused by various factors, including an excess of soft tissue in the throat, the tongue collapsing backward, or the throat muscles not adequately supporting the airway.
On the other hand, CSA occurs when the brain fails to send proper signals to the muscles that control breathing. This can be a result of underlying medical conditions such as heart failure, stroke, or brainstem injury. CSAS, as mentioned earlier, is a combination of both obstructive and central sleep apnea.
The causes of sleep apnea can vary, but certain factors increase the risk of developing this condition. These include obesity, excessive alcohol consumption, smoking, nasal congestion, family history of sleep apnea, and age. Sleep apnea is more prevalent in males and individuals over the age of 40. It is important to note that sleep apnea can occur in individuals of any age or gender.
If left untreated, sleep apnea can have serious consequences for a person’s health and well-being. It can contribute to the development of various medical conditions such as high blood pressure, heart disease, diabetes, and even depression. It can also impact overall quality of life, leading to daytime sleepiness, difficulty concentrating, and impaired cognitive function.
For those interested in the connection between sleep apnea and dreaming, it is important to note that sleep apnea primarily affects the non-REM (rapid eye movement) stages of sleep, as apneas cause frequent awakenings and disrupt the natural sleep architecture. However, it is still possible to experience dreams during these stages of sleep. For more information on sleep apnea and its impact on REM sleep and dreaming, refer to this informative article.
Prevalence and Symptoms
The prevalence of sleep apnea is significant, with millions of individuals worldwide affected by this disorder. It is estimated that approximately 20% of adults may have some form of sleep apnea. However, it is important to note that many cases of sleep apnea go undiagnosed, making the actual prevalence potentially higher. Sleep apnea can affect individuals of all ages, genders, and body types, although it is more common in males and individuals who are overweight or obese.
The symptoms of sleep apnea can vary but often include:
1. Loud and chronic snoring: Snoring is a common symptom of sleep apnea, and it is often reported by bed partners or family members. The snoring is typically loud, disruptive, and may be accompanied by gasping or choking sounds as breathing resumes.
2. Excessive daytime sleepiness: Individuals with sleep apnea often experience excessive daytime sleepiness, regardless of the amount of time spent in bed. This can lead to difficulties concentrating, decreased productivity, and an increased risk of accidents or falls.
3. Morning headache: Waking up with a headache is another common symptom of sleep apnea. The headache is often described as dull or throbbing and typically improves throughout the day.
4. Fragmented sleep: Sleep apnea can interrupt the normal sleep cycle, causing frequent awakenings throughout the night. These interruptions can lead to fragmented sleep, leaving individuals feeling unrested and fatigued during the day.
5. Mood disturbances: Sleep apnea has been linked to mood disturbances such as irritability, depression, and anxiety.
6. Nighttime sweating: Some individuals with sleep apnea may experience excessive sweating during sleep, particularly around the head and neck area.
It is important to note that the presence of these symptoms does not necessarily indicate that an individual has sleep apnea. A formal diagnosis can only be made through a sleep study conducted by a healthcare professional. However, recognizing these symptoms and seeking medical attention is crucial in order to receive appropriate treatment and improve overall sleep quality. For more information on sleep apnea and its potential impact on lucid dreaming, you can refer to this informative article.
Diagnosis and Treatment
Diagnosing sleep apnea involves a combination of medical history evaluation, physical examination, and sleep studies. Healthcare professionals will typically start by discussing symptoms and risk factors with the patient. They may inquire about the frequency and intensity of snoring, daytime sleepiness, and other related symptoms. A physical examination may be performed to assess the patient’s overall health and look for any anatomical factors that may contribute to sleep apnea.
One of the most common diagnostic tools for sleep apnea is a sleep study, also known as polysomnography. This study is conducted in a specialized sleep center or at home using portable monitoring devices. It records various parameters during sleep, including brain activity, heart rate, breathing patterns, oxygen levels, and body movements. The data collected during the sleep study helps healthcare professionals determine the presence and severity of sleep apnea.
Once diagnosed, treatment options for sleep apnea focus on improving airflow and ensuring an uninterrupted breathing pattern during sleep. Lifestyle modifications may be recommended, such as weight loss, regular exercise, avoiding alcohol and sedatives, and sleeping on the side instead of the back. These lifestyle changes can sometimes alleviate mild cases of sleep apnea.
For moderate to severe sleep apnea, the gold standard treatment is continuous positive airway pressure (CPAP) therapy. This involves wearing a mask connected to a machine that delivers pressurized air to keep the airway open. The positive air pressure prevents the collapse of the airway, reducing or eliminating episodes of breathing pauses. CPAP therapy is highly effective in managing sleep apnea symptoms, improving sleep quality, and reducing the associated health risks.
In some cases, alternative treatment options may be considered, such as oral appliances that help reposition the jaw and tongue to keep the airway open, or surgical interventions to remove obstructions in the airway. The choice of treatment depends on the severity of the sleep apnea, individual preferences, and the advice of healthcare professionals.
It is important for individuals with sleep apnea to work closely with healthcare professionals to monitor their condition and adjust treatment as needed. Regular follow-up appointments and adherence to recommended treatments can significantly improve sleep quality and overall well-being for those with sleep apnea.
Link between Sleep Apnea and Parasomnias
The link between sleep apnea and parasomnias, such as sleepwalking, has been a topic of increasing interest in the field of sleep medicine. Sleepwalking, also known as somnambulism, is a parasomnia characterized by complex behaviors performed during sleep. While the exact mechanisms linking sleep apnea and sleepwalking are not fully understood, studies have shown a significant association between the two conditions. It is believed that the fragmented sleep caused by sleep apnea may disrupt the normal sleep cycles and increase the likelihood of parasomnias occurring. Additionally, both sleep apnea and sleepwalking have been found to share common risk factors, such as obesity and certain medications. Further research is needed to fully elucidate the relationship between these conditions and develop targeted treatment strategies. Other parasomnias, such as sleep talking, night terrors, and REM sleep behavior disorder, have also been linked to sleep apnea. Recognizing this link is crucial in effectively managing and treating these disruptive sleep disorders.
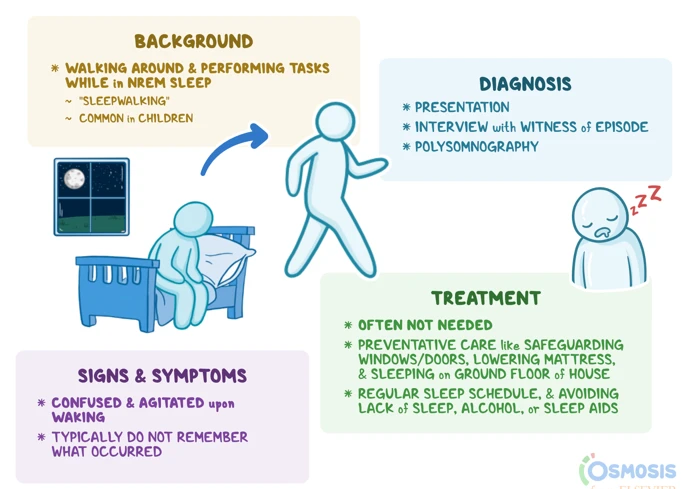
Exploring Sleepwalking
Sleepwalking, also known as somnambulism, is a fascinating and complex parasomnia that occurs during the non-REM stages of sleep. It is characterized by activities ranging from simple behaviors like sitting up in bed or walking around the room to more complex actions like cooking or driving, all while the person is still asleep. The exact cause of sleepwalking is not fully understood, but it is believed to involve a combination of genetic and environmental factors. Sleep deprivation, certain medications, and medical conditions such as sleep apnea can also contribute to the occurrence of sleepwalking episodes. Sleepwalkers often have a blank or staring expression on their faces and may be difficult to awaken or communicate with. It is important to note that while sleepwalking itself is usually harmless, it can lead to potential injuries if the individual interacts with their environment in a dangerous way. The duration of sleepwalking episodes can vary, ranging from a few seconds to half an hour or longer. It typically occurs in the first few hours of sleep, during deep stages of slow-wave sleep. Sleepwalkers may have no memory of their actions upon waking, or they may have fragmented and unclear memories. To reduce the risk of injury during sleepwalking episodes, it is recommended to create a safe sleeping environment by removing objects or obstacles that may be tripping hazards. Additionally, maintaining a consistent sleep schedule and addressing any underlying factors such as sleep apnea can help manage and reduce the occurrence of sleepwalking.
Other Parasomnias Associated with Sleep Apnea
Sleep apnea not only has a correlation with sleepwalking but also with other parasomnias. Here are some of the parasomnias that have been found to be associated with sleep apnea:
1. Night Terrors: Night terrors are intense episodes of fear, panic, and distress during sleep. These episodes often include screaming, thrashing, and a sense of terror, leaving the individual in a state of confusion upon awakening. Research has shown a higher prevalence of night terrors in individuals with sleep apnea, suggesting a potential connection between the two.
2. Sleep Talking: Sleep talking, also known as somniloquy, is a parasomnia characterized by talking or making sounds during sleep. While it is considered a relatively harmless sleep disorder, studies have found an increased prevalence of sleep talking in individuals with sleep apnea. The exact mechanisms underlying this association are not fully understood but may be related to the disrupted sleep patterns caused by sleep apnea.
3. Sleep Bruxism: Sleep bruxism refers to the grinding or clenching of teeth during sleep. It is a common parasomnia that can lead to dental problems, jaw pain, and headaches. Sleep apnea has been found to be more prevalent in individuals with sleep bruxism, suggesting a possible relationship between the two disorders. The mechanisms linking sleep apnea and sleep bruxism are still being studied, but it has been hypothesized that the arousal response triggered by sleep apnea episodes may contribute to the development of sleep bruxism.
4. Nightmares: Nightmares are vivid and disturbing dreams that cause intense fear, anxiety, or sadness. While nightmares can occur in individuals without sleep apnea, there is evidence suggesting that sleep apnea may contribute to an increased frequency and intensity of nightmares. The exact mechanisms underlying this association are not fully understood, but disruptions in sleep architecture and oxygen levels during sleep apnea episodes may play a role.
It is important to note that the associations between sleep apnea and these parasomnias are still being researched and understood. More studies are needed to determine the exact nature of these relationships and how they can be effectively managed and treated. Nevertheless, recognizing these connections can help healthcare professionals in providing comprehensive care for individuals experiencing both sleep apnea and parasomnias.
The Mechanisms at Play
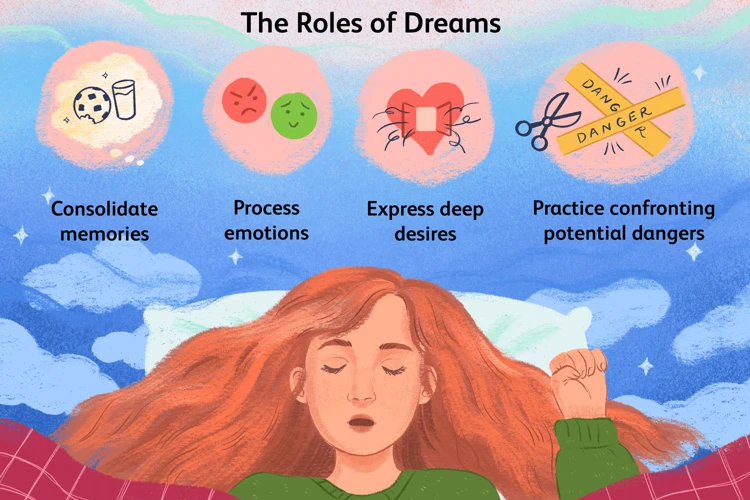
Sleep apnea can play a significant role in the occurrence of parasomnias like sleepwalking. The mechanisms behind this link lie in the disruption of the normal sleep cycle caused by sleep apnea. During sleep, the body goes through different stages, including rapid eye movement (REM) sleep and non-REM sleep. REM sleep is the stage where dreaming predominantly occurs, and it is during this stage that sleepwalking often takes place. Sleep apnea can disrupt the normal progression of sleep stages, leading to fragmented and shallow sleep. This disruption can cause an irregular transition between REM and non-REM sleep, increasing the likelihood of sleepwalking episodes. Additionally, the intermittent pauses in breathing during sleep apnea can lead to brief periods of hypoxia (low oxygen levels) in the brain. These episodes of oxygen deprivation have been linked to triggering parasomnias. The combination of disrupted sleep architecture and intermittent oxygen deprivation creates an environment conducive to the development of sleepwalking and other parasomnias. By addressing sleep apnea and improving sleep quality, the frequency and severity of these sleep disorders can be reduced.
Impact on Sleep Quality and Duration
Sleep apnea can have a significant impact on both sleep quality and duration. When individuals with sleep apnea experience breathing interruptions during the night, their sleep cycles are disrupted. This can lead to fragmented sleep, causing them to wake up multiple times throughout the night, even if they are unaware of it. As a result, the individual may feel excessively tired and fatigued during the day.
One of the key consequences of sleep apnea is a reduction in the amount of deep and REM (rapid eye movement) sleep experienced. Deep sleep is essential for physical restoration and repair, while REM sleep is crucial for cognitive functions and emotional processing. Without adequate amounts of these sleep stages, individuals may wake up feeling unrefreshed and find it challenging to concentrate or focus during the day.
Sleep apnea can also lead to an increase in nighttime awakenings, further disrupting the overall duration of sleep. The constant interruptions in breathing trigger the body to partially wake up to resume normal breathing, often resulting in a cycle of brief awakenings. This can prevent individuals from achieving the recommended amount of sleep needed for optimal functioning and overall health.
Additionally, the recurrent drops in blood oxygen levels that occur with sleep apnea can have serious implications for sleep quality. The fluctuations in oxygen levels can cause a person to wake up gasping for air or experience shallow breathing, leading to a sense of suffocation or choking. This can be alarming and disruptive, contributing to a poor sleep experience.
The combination of fragmented sleep, reduced deep and REM sleep, increased awakenings, and oxygen fluctuations ultimately results in a diminished sleep quality and duration for individuals with sleep apnea. It is crucial to address and effectively manage sleep apnea to improve sleep outcomes and prevent the potential development or aggravation of parasomnias such as sleepwalking.
Understanding the Risks

Sleep apnea, if left untreated, can pose several risks and complications to overall health and well-being. One of the primary risks associated with sleep apnea is the impact it can have on cardiovascular health. The repeated pauses in breathing during sleep can lead to low oxygen levels in the blood, which in turn can increase the risk of hypertension, heart disease, and stroke. Sleep apnea has also been linked to an increased risk of developing type 2 diabetes. The disrupted sleep patterns and oxygen deprivation can disrupt the body’s ability to regulate blood sugar levels, contributing to insulin resistance. Additionally, sleep apnea can have a negative impact on cognitive function. The fragmented sleep caused by the frequent awakenings can lead to daytime sleepiness, difficulty concentrating, and memory problems. These cognitive impairments can affect daily activities and increase the risk of accidents, both at home and in the workplace. Untreated sleep apnea can lead to a decreased quality of life, as individuals may experience reduced energy levels, mood disturbances, and a decreased ability to perform daily tasks. It is important to recognize and address these risks associated with sleep apnea to prevent further complications and improve overall health. Seeking proper diagnosis and treatment from healthcare professionals can help mitigate these risks and enhance the quality of life for individuals with sleep apnea.
Managing and Treating Sleep Apnea-Related Parasomnias
Managing and treating sleep apnea-related parasomnias requires a multifaceted approach. Lifestyle modifications play a crucial role in minimizing the occurrence and severity of parasomnias. These modifications can include maintaining a consistent sleep schedule, creating a relaxing bedtime routine, and avoiding alcohol and caffeine before bed. Weight loss, if applicable, can also be beneficial, as obesity is a common risk factor for both sleep apnea and parasomnias. Additionally, individuals with sleep apnea-related parasomnias may benefit from using continuous positive airway pressure (CPAP) therapy. This involves wearing a mask during sleep that delivers a constant flow of air, keeping the airway open. Other treatment options may include medication to manage specific symptoms or addressing any underlying medical conditions contributing to the parasomnias. Consulting with a healthcare professional is essential to explore the most suitable treatment plan tailored to each individual’s needs.
Lifestyle Modifications
Lifestyle modifications can play a crucial role in managing and treating sleep apnea-related parasomnias. Making certain changes to one’s daily routine and habits can help improve sleep quality and reduce the frequency and severity of parasomnias. One important step is maintaining a healthy weight through regular exercise and a balanced diet. Obesity is a known risk factor for sleep apnea, so shedding excess pounds can alleviate symptoms and decrease the likelihood of parasomnias. Avoiding alcohol, sedatives, and smoking is also essential, as these substances can relax the throat muscles and contribute to airway obstruction during sleep. Establishing a consistent sleep schedule and creating a relaxing bedtime routine can help regulate sleep patterns and promote better overall sleep. Additionally, optimizing the sleep environment by keeping it dark, quiet, and comfortable can enhance sleep quality. A sleep-friendly bedroom can minimize the risk of disruptions that can trigger parasomnia episodes. While lifestyle modifications may not completely eliminate parasomnias associated with sleep apnea, they can significantly improve sleep outcomes and overall well-being.
CPAP Therapy for Sleep Apnea Treatment
CPAP (Continuous Positive Airway Pressure) therapy is one of the most common and effective treatments for sleep apnea. It involves the use of a machine that delivers a constant flow of pressurized air through a mask worn over the nose or mouth during sleep. This pressurized air helps to keep the airway open, preventing the collapse or obstruction that causes sleep apnea episodes. CPAP therapy not only alleviates the symptoms of sleep apnea but also improves overall sleep quality and reduces the associated risks. By providing a steady stream of air, CPAP therapy eliminates pauses in breathing, reduces snoring, and ensures the continuous supply of oxygen to the body and brain.
When initiating CPAP therapy, a sleep specialist will determine the optimal pressure level required for each individual. This pressure level is usually determined during a diagnostic sleep study where various pressures are tested to find the one that effectively clears any obstruction. Finding the right mask is also crucial for successful CPAP therapy. Masks come in different styles, including nasal masks, full-face masks, and nasal pillows, allowing for customization based on individual comfort and breathing preferences.
Using CPAP therapy consistently and properly is key to its effectiveness. It may take some time for individuals to adjust to sleeping with a mask and the sensation of pressurized air. However, the benefits of CPAP therapy, such as improved sleep quality, reduced daytime sleepiness, and decreased risk of associated health issues, make the adjustment worthwhile. Regular follow-up appointments with a sleep specialist are important to monitor progress, make any necessary adjustments, and address any concerns or discomfort.
It is worth noting that while CPAP therapy is highly effective, it may not be suitable for everyone. Some individuals may find the equipment uncomfortable or experience side effects such as nasal congestion, dryness, or skin irritation. In such cases, alternative therapies such as bilevel positive airway pressure (BiPAP) or adaptive servo-ventilation (ASV) may be recommended. Additionally, lifestyle modifications like weight loss, sleeping in certain positions, or avoiding alcohol and sedatives may also complement CPAP therapy in managing sleep apnea.
With advancements in technology, CPAP machines have become more compact, quieter, and user-friendly, making adherence to therapy easier for individuals. Accessories such as heated humidifiers can also help alleviate issues like dryness or nasal congestion. The overall goal of CPAP therapy is to provide a consistent and uninterrupted flow of pressurized air, ensuring a restful night’s sleep and minimizing the disruptive episodes associated with sleep apnea.
Additional Treatment Options
Additional treatment options for sleep apnea-related parasomnias may be considered for individuals who do not respond well to lifestyle modifications or CPAP therapy. These alternative approaches aim to address the underlying causes and symptoms of both sleep apnea and associated parasomnias. Here are some additional treatment options that may be recommended:
1. Oral Appliances: Custom-made oral appliances, such as dental devices or mandibular advancement splints, can help to keep the airway open by repositioning the jaw during sleep. These devices are designed to improve breathing and reduce the frequency and severity of both sleep apnea and parasomnias.
2. Surgery: In some cases, surgical intervention may be necessary to correct anatomical abnormalities that contribute to sleep apnea. Procedures like uvulopalatopharyngoplasty (UPPP), tonsillectomy, or maxillomandibular advancement (MMA) may be recommended to remove excess tissue or reposition the jaw and improve airflow.
3. Positional Therapy: For individuals whose sleep apnea and parasomnias are worsened in certain sleeping positions, positional therapy may be beneficial. This approach aims to encourage sleeping in specific positions that promote better breathing and reduce the occurrence of apneas and associated sleep disturbances.
4. Medications: In some cases, medications may be prescribed to address specific symptoms or underlying conditions that contribute to sleep apnea and parasomnias. For example, if sleepwalking or other parasomnias are directly associated with certain medications, alternative drugs may be recommended.
It is important to note that the effectiveness of these additional treatment options can vary from person to person. Consultation with a healthcare professional who specializes in sleep disorders is crucial to determine the most suitable approach based on individual needs and circumstances.
Conclusion
In conclusion, it is evident that sleep apnea plays a significant role in the development and exacerbation of sleepwalking and other parasomnias. The link between these conditions highlights the interconnectedness of sleep disorders and emphasizes the importance of identifying and addressing underlying factors. By understanding the mechanisms at play and the impact on sleep quality, individuals and healthcare professionals can take appropriate steps to manage and treat sleep apnea-related parasomnias effectively. Lifestyle modifications, such as weight loss and avoiding sleep disruptors, can have a positive impact on both sleep apnea and associated parasomnias. Additionally, the use of CPAP therapy is a proven treatment option for sleep apnea, which can also help alleviate parasomnias. It is crucial for individuals experiencing these sleep disorders to consult with medical professionals for accurate diagnosis and tailored treatment plans. By addressing sleep apnea and its relationship with parasomnias, individuals can experience improved sleep quality, reduced symptoms, and enhanced overall well-being.
Frequently Asked Questions
How common is sleep apnea?
Sleep apnea is prevalent, affecting approximately 20% of adults worldwide.
What are the main causes of sleep apnea?
Sleep apnea can be caused by factors such as obesity, genetics, and anatomical abnormalities in the airway.
What are the symptoms of sleep apnea?
Common symptoms of sleep apnea include loud and chronic snoring, daytime sleepiness, morning headaches, and difficulty concentrating.
Can sleep apnea contribute to weight gain?
Yes, there is evidence to suggest that sleep apnea can contribute to weight gain and obesity due to various factors, such as hormonal imbalances and decreased physical activity.
Is sleep apnea related to other medical conditions?
Yes, sleep apnea has been associated with an increased risk of cardiovascular disease, high blood pressure, stroke, and diabetes.
How is sleep apnea diagnosed?
Sleep apnea is typically diagnosed through a sleep study, which may involve monitoring breathing patterns, brain activity, heart rate, and oxygen levels during sleep.
What are the treatment options for sleep apnea?
Treatment options for sleep apnea include lifestyle modifications such as weight loss, avoiding alcohol and sedatives, using CPAP devices, and in some cases, surgical interventions.
Can sleep apnea lead to sleepwalking?
Yes, there is a link between sleep apnea and sleepwalking, with some studies suggesting that sleep-disordered breathing can trigger parasomnias like sleepwalking.
Are there any risks associated with untreated sleep apnea?
Untreated sleep apnea can pose significant health risks, including an increased risk of heart disease, stroke, and even accidents due to excessive daytime sleepiness.
Can treating sleep apnea improve sleep quality?
Yes, treating sleep apnea can improve sleep quality by ensuring adequate oxygenation and reducing disruptions in breathing during sleep, resulting in more restful and uninterrupted sleep.