Nightmares and PTSD: Unraveling the Intricate Connection
As humans, we rely on sleep to rejuvenate our bodies and minds, but for individuals suffering from Post-Traumatic Stress Disorder (PTSD), sleep can bring forth a different kind of torment. Nightmares, vivid and disturbing dreams that occur during rapid eye movement (REM) sleep, often haunt those with PTSD, intensifying their already crippling symptoms. The relationship between nightmares and PTSD is intricate, with nightmares both being a symptom and a contributing factor to the disorder. This article delves into the role of nightmares in PTSD, exploring their psychological impact, the underlying neural mechanisms, treatment approaches, and self-help strategies aimed at managing these distressing nocturnal experiences. With a better understanding of this complex interplay, we can shed light on the pathways towards improving the quality of life for individuals battling with PTSD and chronic nightmares.
The Relationship Between Nightmares and PTSD
The relationship between nightmares and PTSD is undeniably intricate. Nightmares are not only a hallmark symptom of PTSD but also play a significant role in the development and maintenance of the disorder. Individuals with PTSD often experience nightmares that vividly reenact the traumatic event they have endured. These distressing dream sequences can intensify the emotional and physiological distress individuals with PTSD already experience during waking hours. Additionally, nightmares can trigger flashbacks and intrusive memories, leading to a perpetual cycle of re-traumatization. The frequency and severity of nightmares are closely associated with the severity and duration of PTSD symptoms, further exacerbating the overall psychological distress. Understanding the connection between nightmares and PTSD is crucial in developing effective treatment interventions that target both symptom clusters. Through the exploration of the intricate relationship between nightmares and PTSD, we can gain insight into the shared neurobiological mechanisms and therapeutic strategies that can alleviate the debilitating impact of nightmares on individuals’ well-being. To learn more about overcoming nightmares, you can read our in-depth article on how to overcome nightmares.
The Psychological Impact of Nightmares in PTSD
Nightmares in individuals with PTSD have a profound psychological impact, further exacerbating the already distressing symptoms of the disorder. One of the psychological effects of nightmares in PTSD is nightmare re-experiencing, where the traumatic event is vividly relived during sleep, leading to intense fear, distress, and a disrupted sense of personal safety. These nightmares can re-traumatize individuals, causing them to feel helpless, overwhelmed, and emotionally dysregulated. Emotional dysregulation is another significant psychological impact of nightmares in PTSD. The intense emotions evoked during nightmares can spill over into waking life, leading to difficulties in managing and regulating emotions effectively. Sleep disturbances caused by nightmares, including disruptions in sleep continuity and quality, can also contribute to mood disturbances, daytime fatigue, and impaired cognitive functioning in individuals with PTSD. Understanding the psychological impact of nightmares is crucial for developing targeted interventions aimed at alleviating distress and improving overall psychological well-being. To explore more about the interplay between nightmares and sleep disorders, you can read our comprehensive article on exploring nightmares and sleep disorders.
Nightmare Re-experiencing
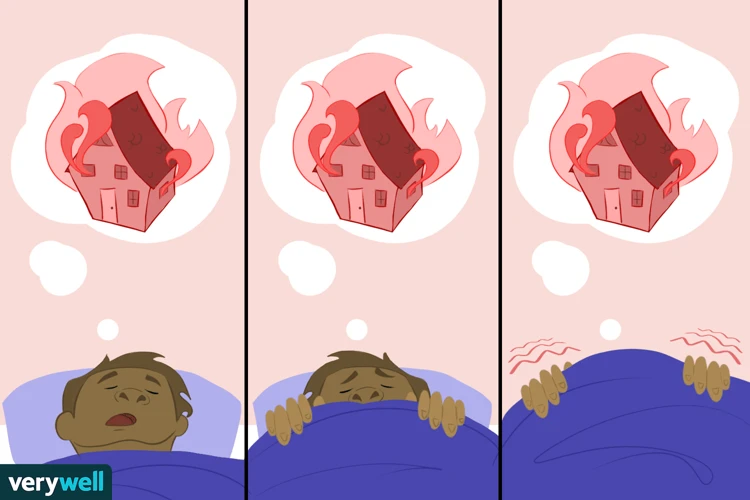
Nightmare re-experiencing is a distressing symptom commonly observed in individuals with PTSD. It involves the vivid and intrusive recurrence of the traumatic event in the form of nightmares during sleep. These nightmares often mirror the original traumatic experience, incorporating sensory details, emotions, and feelings of helplessness. The experience of nightmare re-experiencing can be overwhelming, as it reactivates the trauma-related distress and can lead to heightened arousal and fear upon waking. Individuals may find it challenging to fall back asleep or may be hesitant to sleep altogether, fearing the recurrence of these distressing nightmares. This symptom contributes to the cycle of anxiety and avoidance often seen in PTSD, as individuals may start to avoid sleep or certain triggers associated with their traumatic experiences. To understand more about nightmares in children and strategies for parents to manage them, you can refer to our informative article on nightmares in children: causes and strategies for parents.
Emotional Dysregulation
Emotional dysregulation is a prominent psychological consequence of nightmares in individuals with PTSD. Nightmares often evoke intense and distressing emotions, such as fear, terror, sadness, anger, or guilt. These emotional responses can be overwhelming and difficult to manage, leading to a dysregulation of emotions both during sleep and wakefulness. Individuals may struggle to regulate their emotions throughout the day, experiencing heightened sensitivity and reactivity to stressors. This emotional dysregulation can impair their ability to effectively cope with daily challenges and contribute to interpersonal difficulties. The emotional intensity experienced during nightmares can spill over into waking life, making it challenging to distinguish between dream and reality and perpetuating a sense of constant anxiety and hypervigilance. Strategies for managing emotional dysregulation in PTSD may involve techniques such as mindfulness exercises, grounding techniques, and emotion regulation skills training to help individuals regain control over their emotions and reduce the impact of nightmares on their daily functioning.
Sleep Disturbances
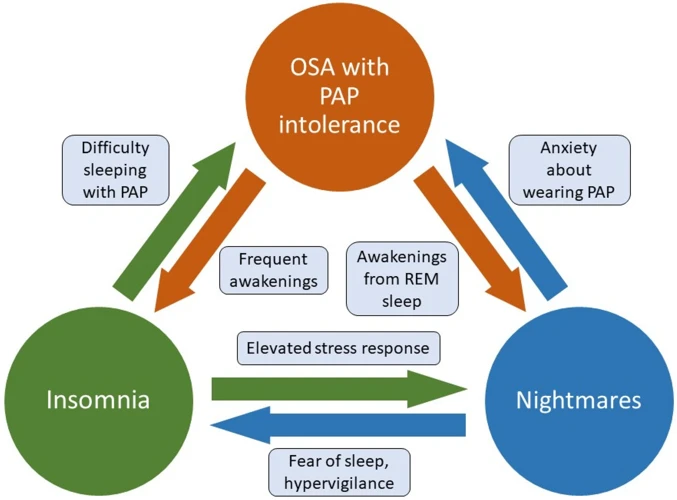
Sleep Disturbances: One of the significant impacts of nightmares in PTSD is the disruption it causes to sleep patterns and overall sleep quality. Sleep disturbances are a common symptom experienced by individuals with PTSD, and nightmares play a significant role in contributing to these disruptions. Nightmares can result in fear and anxiety, making it difficult for individuals to fall asleep or return to sleep after waking up. The intense emotions and vivid imagery experienced during nightmares can also lead to physiological arousal, such as increased heart rate and sweating, further hindering the ability to achieve restful sleep.
The presence of nightmares can lead to sleep fragmentation, where individuals experience multiple awakenings throughout the night. This can prevent the individual from reaching deep, restorative stages of sleep, such as rapid eye movement (REM) sleep and slow-wave sleep (SWS). As a result, individuals with PTSD may feel perpetually fatigued, have difficulty concentrating, and experience daytime drowsiness.
The constant fear of experiencing nightmares can create a fear of sleep itself, contributing to insomnia and sleep avoidance behaviors. This vicious cycle of sleep disturbances, nightmares, and anxiety can significantly impact an individual’s overall psychological well-being and exacerbate their PTSD symptoms.
It is important for individuals with PTSD to seek professional help to address their sleep disturbances. Therapies such as Cognitive Behavioral Therapy for Insomnia (CBT-I) can be effective in improving sleep quality and reducing nightmares. By targeting the underlying causes of sleep disturbances and providing techniques to manage anxiety and nightmares, individuals can experience better sleep, reduced daytime impairment, and an overall improvement in their quality of life.
The Neurobiological Basis of Nightmares in PTSD
Nightmares in PTSD have a profound neurobiological basis that sheds light on the intricate mechanisms underlying their occurrence. The amygdala, an almond-shaped structure in the brain, plays a crucial role in processing and regulating emotions, particularly fear. In individuals with PTSD, the amygdala becomes hyperactive, leading to heightened emotional responses and increased reactivity to trauma-related stimuli. This hyperactivity directly contributes to the intense emotional content of nightmares experienced by individuals with PTSD. The hippocampus, a region responsible for memory consolidation, is adversely affected in PTSD. The impaired functioning of the hippocampus results in fragmented and distorted memories, which are frequently revisited during nightmares. Additionally, the prefrontal cortex, known for its role in executive functions and emotional regulation, becomes compromised in individuals with PTSD, impeding the ability to effectively control fear responses and effectively process traumatic memories. Understanding the neurobiological basis of nightmares in PTSD is crucial in developing targeted treatment interventions that aim to modulate these brain regions and alleviate the distressing symptoms.
The Role of the Amygdala
The amygdala, a small almond-shaped structure located deep within the brain, plays a crucial role in the manifestation of nightmares in individuals with PTSD. Known for its involvement in emotional processing and fear response, the amygdala becomes hyperactive in people with PTSD, heightening fear and anxiety responses. This hyperactivity is particularly relevant when it comes to nightmares. During REM sleep, when nightmares occur, the amygdala is activated, leading to the generation of intense emotional experiences. The amygdala’s heightened activity during nightmares further reinforces the trauma-related memories and emotions associated with the original traumatic event. This contributes to the re-experiencing of past trauma during nightmares and the subsequent emotional dysregulation individuals with PTSD often face. Understanding the role of the amygdala in nightmares provides valuable insight into the underlying neurobiology of PTSD. It highlights the importance of targeting this structure and its associated neural circuits in therapeutic interventions aimed at mitigating nightmares and their impact on overall well-being.
The Role of the Hippocampus
The hippocampus, a vital structure located in the brain’s medial temporal lobe, plays a crucial role in the formation and consolidation of memories, including those associated with traumatic experiences. In individuals with PTSD, the hippocampus is believed to be directly affected and compromised. Research suggests that the hippocampus may contribute to the occurrence of nightmares in PTSD through its involvement in memory processing and emotional regulation.
Memory Processing: The hippocampus functions as a memory hub, aiding in the encoding, consolidation, and retrieval of memories. In individuals with PTSD, the hippocampus may struggle to properly encode and consolidate memories related to the traumatic event. This impaired memory processing can lead to fragmented and disorganized memories, which may manifest in nightmares as terrifying and fragmented dream sequences.
Emotional Regulation: The hippocampus also serves a critical role in emotional regulation by modulating the stress response. In individuals with PTSD, the hippocampus may exhibit reduced volume and altered functioning, leading to an impaired ability to regulate emotional responses. This dysregulation can result in heightened fear and anxiety, which may be reflected in the intense emotional content of nightmares.
The interaction between the hippocampus and other brain regions, such as the amygdala and prefrontal cortex, further contributes to the occurrence of nightmares in PTSD. The amygdala, involved in processing emotions, and the prefrontal cortex, responsible for executive functions and threat appraisal, work in conjunction with the hippocampus to shape the content and intensity of nightmares.
Understanding the role of the hippocampus in nightmares can help inform therapeutic interventions aimed at targeting memory processing and emotional dysregulation. By employing techniques like trauma-focused therapy and interventions designed to enhance hippocampal functioning, clinicians can potentially lessen the frequency and intensity of nightmares in individuals with PTSD, ultimately improving their overall quality of life.
The Role of the Prefrontal Cortex
The prefrontal cortex (PFC) plays a critical role in the occurrence and regulation of nightmares in individuals with PTSD. This region of the brain is responsible for higher-order cognitive functions such as decision-making, attention, and emotion regulation. In individuals with PTSD, the PFC may exhibit abnormalities in functioning, impairing its ability to effectively regulate fear and emotional responses during sleep. These dysregulations contribute to the frequency and intensity of nightmares experienced.
Studies have shown that reduced activation in the PFC during REM sleep is associated with increased nightmare frequency in individuals with PTSD. This suggests that the PFC’s role in inhibiting fear responses and regulating emotional reactivity is compromised, allowing distressing dream content to prevail. Additionally, the PFC’s role in context processing and memory integration is disrupted, leading to fragmented and intrusive memories being incorporated into nightmares.
The PFC interacts with other brain regions involved in fear processing, such as the amygdala and hippocampus, contributing to the nightmare mechanisms in PTSD. Dysfunction in the communication between these regions can result in an imbalance between fear extinction and fear consolidation processes, leading to the persistence of traumatic memories within nightmares.
While the exact mechanisms underlying the PFC’s involvement in nightmares in PTSD are still being investigated, it is clear that this brain region plays a critical role in regulating emotional responses and fear processing during sleep. Understanding these neural processes can inform the development of targeted therapeutic interventions that aim to restore PFC function and alleviate nightmare-related distress in individuals with PTSD.
Treatment Approaches for Nightmares in PTSD
Treatment approaches for nightmares in PTSD involve a multifaceted approach aimed at reducing the frequency and intensity of these distressing dreams, improving overall sleep quality, and alleviating the psychological distress associated with Post-Traumatic Stress Disorder. Cognitive Behavioral Therapy (CBT) is a commonly utilized therapeutic intervention that focuses on identifying and modifying negative thought patterns and behaviors related to nightmares. This approach includes techniques such as exposure therapy, imagery rehearsal therapy, and rescripting, which aim to desensitize individuals to the content of nightmares and replace them with more positive and adaptive dream scenarios. Another effective treatment option is Eye Movement Desensitization and Reprocessing Therapy (EMDR) that incorporates bilateral eye movements or other forms of sensory stimulation to process traumatic memories and alleviate the distress associated with nightmares. Medications, such as selective serotonin reuptake inhibitors (SSRIs), may also be prescribed to help reduce the frequency of nightmares. The combination of therapy and medication can provide substantial relief to individuals suffering from PTSD-related nightmares, aiding them in their journey towards healing and recovery.
Cognitive Behavioral Therapy
Cognitive Behavioral Therapy: Cognitive Behavioral Therapy (CBT) is a widely recognized and effective treatment approach for managing nightmares in individuals with PTSD. This therapy focuses on identifying and restructuring maladaptive thought patterns and behaviors that contribute to the maintenance of nightmares. CBT for nightmares typically involves several techniques, including imagery rehearsal therapy (IRT), which aims to modify the content and emotional intensity of nightmares. During IRT, individuals are encouraged to rewrite their nightmares, incorporating new and positive elements that help resolve the original traumatic experiences. By repeatedly rehearsing these revised dream scenarios, individuals can gain a sense of mastery and reduce distress associated with nightmares.
CBT also targets cognitive distortions and beliefs related to nightmares. Therapists help individuals recognize and challenge irrational thoughts and fears associated with nightmares, replacing them with more realistic and adaptive cognitions. This cognitive restructuring promotes a sense of control and reduces the emotional impact of nightmares.
In addition to addressing cognitive factors, CBT for nightmares in PTSD may also incorporate behavioral techniques. This may include implementing a regular sleep schedule, practicing relaxation techniques before bedtime, and implementing safety behaviors to reduce anxiety and promote better sleep. Trauma-focused CBT, which integrates exposure therapy and cognitive restructuring, may also be used to address the underlying trauma that contributes to nightmares.
Research has shown that CBT can significantly reduce nightmare frequency, intensity, and associated distress in individuals with PTSD. It equips individuals with practical skills and strategies to cope with nightmares effectively and regain a sense of control over their sleep and well-being. If you’re interested in exploring more about nightmares and how they relate to sleep disorders, you can check out our detailed article on exploring nightmares and sleep disorders.
Eye Movement Desensitization and Reprocessing Therapy
Eye Movement Desensitization and Reprocessing Therapy (EMDR) has emerged as a promising treatment approach for nightmares in PTSD. This therapy, initially developed for trauma-related disorders, aims to reprocess traumatic memories and alleviate associated distress. EMDR incorporates elements of cognitive-behavioral therapy (CBT) and bilateral stimulation, which can involve eye movements, hand taps, or auditory tones. The goal of EMDR is to facilitate the integration of traumatic memories, allowing individuals to reprocess the distressing experiences in a safe and controlled environment. During EMDR sessions, the therapist guides the individual through a series of trauma-focused protocols, including identifying a target memory, associated negative beliefs, and disturbing emotions or physical sensations. Bilateral stimulation is then used while the individual holds these elements of the trauma in mind, promoting the desensitization and reprocessing of the traumatic memory. The therapist helps the individual replace negative beliefs with positive ones, fostering cognitive restructuring and emotional healing. EMDR has shown promising results in reducing the frequency and intensity of nightmares in individuals with PTSD. This therapy not only targets nightmares but also addresses other symptoms of PTSD, offering a comprehensive treatment approach. To learn more about different treatment approaches for nightmares in PTSD, you can read our article on exploring the connection between nightmares and sleep disorders.
Medications
Medications can be a valuable component of the treatment approach for managing nightmares in individuals with PTSD. While therapy remains the primary treatment method, certain medications can help alleviate the intensity and frequency of nightmares, allowing individuals to experience more restful sleep. Two types of medications are commonly prescribed in the context of PTSD-related nightmares: selective serotonin reuptake inhibitors (SSRIs) and prazosin.
SSRIs, such as sertraline and paroxetine, are antidepressant medications that can help regulate mood and reduce anxiety. They are often prescribed to individuals with PTSD to address the overall symptoms of the disorder, including nightmares. By increasing the availability of serotonin in the brain, SSRIs can help normalize sleep patterns and reduce the occurrence of distressing dreams during REM sleep.
Prazosin, on the other hand, is an alpha-1 adrenergic blocker typically used to treat high blood pressure. However, it has shown efficacy in reducing the severity and frequency of nightmares in individuals with PTSD. Prazosin works by blocking norepinephrine, a stress hormone, from binding to alpha-1 receptors in the brain, thereby reducing the hyperarousal and anxiety associated with nightmares.
It is important to note that while medications can be beneficial in managing nightmares, they are not a standalone solution. They should be used in conjunction with therapy, particularly cognitive-behavioral therapy (CBT) or eye movement desensitization and reprocessing therapy (EMDR), to address the underlying trauma and provide comprehensive treatment for PTSD. Additionally, the decision to use medication should be made in consultation with a healthcare professional who can assess individual needs, potential side effects, and interactions with other medications.
Understanding the role of medications in addressing nightmares in PTSD allows healthcare providers to tailor treatment plans to fit the unique needs of each individual. By combining therapy, medication, and other self-help strategies, individuals with PTSD can gain better control over their nightmares, leading to improved sleep and overall well-being.
Self-Help Strategies for Managing Nightmares in PTSD
When it comes to managing nightmares in PTSD, self-help strategies can play a crucial role in alleviating distress and improving overall sleep quality. Here are some effective approaches individuals can employ:
- Maintaining a Consistent Sleep Schedule: Establishing and sticking to a regular sleep routine can help regulate sleep patterns and reduce the likelihood of nightmares.
- Creating a Relaxing Bedtime Routine: Engaging in calming activities before bed, such as reading, taking a warm bath, or practicing deep breathing exercises, can promote relaxation and reduce anxiety.
- Engaging in Relaxation Techniques: Incorporating relaxation techniques, such as progressive muscle relaxation or guided imagery, can help reduce stress and promote a sense of calm before sleep.
Implementing these self-help strategies alongside professional treatment can empower individuals with PTSD to take an active role in managing their nightmares and improving sleep quality. By addressing the psychological impact of nightmares and implementing these strategies, individuals can find relief and restore a sense of peace to their nightly rest.
Maintaining a Consistent Sleep Schedule
Maintaining a consistent sleep schedule is crucial for individuals with PTSD who experience nightmares. Sleep disruptions and irregular sleep patterns can worsen the frequency and intensity of nightmares, amplifying the overall distress and impacting daily functioning. Here are some strategies that can help establish a consistent sleep schedule:
- Set a regular bedtime: Determine a specific time to go to bed each night and stick to it, even on weekends or days off. This helps regulate the body’s internal clock and promotes better sleep.
- Create a calming bedtime routine: Engage in activities that promote relaxation before bed, such as taking a warm bath, reading a book, or practicing deep breathing exercises. Establishing a consistent routine signals to the brain that it’s time to wind down and prepare for sleep.
- Avoid stimulating activities before bed: Minimize exposure to screens (such as smartphones or tablets) and stimulating activities, as they can interfere with sleep. Instead, opt for calming activities like listening to soft music or practicing gentle stretching.
- Create a sleep-friendly environment: Ensure that the bedroom is quiet, dark, and at a comfortable temperature. Consider using earplugs, eye masks, or white noise machines to block out disruptive sounds and create a soothing atmosphere.
- Avoid caffeine and heavy meals: Limit the consumption of caffeine and large meals close to bedtime, as they can disrupt sleep and increase the likelihood of nightmares. Opt for lighter, sleep-friendly snacks if needed.
- Stay consistent with wake-up times: Set a regular time to wake up each morning, even if sleep was disturbed during the night. Consistency in wake-up times helps regulate the sleep-wake cycle and promotes better overall sleep quality.
By implementing these strategies and maintaining a consistent sleep schedule, individuals with PTSD can create an environment conducive to restful sleep and reduce the frequency and severity of nightmares.
Creating a Relaxing Bedtime Routine
Creating a relaxing bedtime routine can be immensely beneficial in managing nightmares for individuals with PTSD. By establishing a consistent routine, the body and mind can gradually relax, preparing for a restful sleep. Here are some strategies to incorporate into a soothing bedtime routine:
1. Set a Regular Sleep Schedule: Maintaining a consistent sleep schedule can help regulate the body’s internal clock, promoting more restful sleep. Aim to go to bed and wake up at the same time every day, even on weekends, to establish a steady sleep-wake cycle.
2. Create a Calming Environment: Make your bedroom a sanctuary for sleep. Ensure the room is cool, dark, and quiet, and remove any distractions that may interfere with sleep. Consider using blackout curtains, earplugs, or white noise machines to create a peaceful atmosphere.
3. Practice Relaxation Techniques: Engaging in relaxation techniques before bed can help alleviate stress and anxiety that may contribute to nightmares. Deep breathing exercises, progressive muscle relaxation, or guided imagery can help calm the mind and promote relaxation.
4. Avoid Stimulants: Limit the consumption of caffeine, nicotine, and alcohol, especially in the evening. These substances can disrupt sleep and trigger nightmares. Opt for herbal tea or warm milk instead, promoting relaxation and drowsiness.
5. Unwind with a Bedtime Ritual: Engage in activities that promote relaxation and winding down before bed. This could include reading a book, taking a warm bath, journaling, or practicing gentle stretching or yoga.
Remember, it is essential to find a routine that works best for you. Experiment with different strategies and adjust as necessary. By incorporating a relaxing bedtime routine into your daily life, you can create a conducive atmosphere for restful sleep and reduce the likelihood of nightmares.
Engaging in Relaxation Techniques
Engaging in relaxation techniques can be a helpful strategy for managing nightmares in individuals with PTSD. These techniques aim to calm the mind and body, promote relaxation, and improve overall sleep quality. One effective technique is deep breathing, where individuals focus on slow, deep breaths, inhaling deeply through the nose and exhaling slowly through the mouth. This can help reduce anxiety and induce a sense of calmness before sleep. Progressive muscle relaxation involves systematically tensing and then releasing different muscle groups, promoting physical and mental relaxation. Another technique is guided imagery, where individuals imagine themselves in a peaceful and calming environment, such as a serene beach or a lush garden. This visualization can help distract from nightmares and create a more positive mental and emotional state. Other relaxation techniques such as meditation, yoga, and aromatherapy can also be beneficial in reducing stress and promoting relaxation before bedtime. Experimenting with different techniques and finding what works best for each individual is important. By incorporating relaxation techniques into a regular bedtime routine, individuals with PTSD can create an environment more conducive to peaceful sleep.
Conclusion
In conclusion, understanding the role of nightmares in Post-Traumatic Stress Disorder (PTSD) is crucial for comprehensive treatment and support. Nightmares not only contribute to the psychological distress experienced by individuals with PTSD but also serve as a vivid reenactment of their traumatic experiences, perpetuating a cycle of re-traumatization. The psychological impact of nightmares includes nightmare re-experiencing, emotional dysregulation, and sleep disturbances, all of which further compound the symptoms of PTSD. On a neurobiological level, the amygdala, hippocampus, and prefrontal cortex play critical roles in the occurrence and persistence of nightmares in individuals with PTSD. Treatment approaches, such as Cognitive Behavioral Therapy, Eye Movement Desensitization and Reprocessing Therapy, and medication, have shown promise in managing nightmares and alleviating the overall burden of PTSD. Additionally, self-help strategies like maintaining a consistent sleep schedule, creating a relaxing bedtime routine, and engaging in relaxation techniques can aid individuals in managing nightmares. By addressing the complexity of nightmares in PTSD, we can provide a more comprehensive and effective approach to improve the quality of life for those battling this debilitating disorder.
Frequently Asked Questions
1. Can everyone with PTSD experience nightmares?
No, not everyone with PTSD experiences nightmares. While nightmares are a common symptom of PTSD, it is possible for individuals with PTSD to have other sleep disturbances or not to have any sleep-related symptoms at all.
2. Why do nightmares occur in PTSD?
Nightmares in PTSD are believed to occur due to the brain’s attempts to process and make sense of the traumatic experiences. The vivid and distressing nature of the nightmares reflects the emotional intensity and unresolved trauma associated with PTSD.
3. Are nightmares only experienced during REM sleep?
Yes, nightmares primarily occur during rapid eye movement (REM) sleep, which is the stage of sleep associated with vivid dreaming. However, individuals with PTSD may also experience sleep disturbances during non-REM sleep stages.
4. How do nightmares impact daily functioning in individuals with PTSD?
Nightmares can severely impact the daily functioning of individuals with PTSD. They can result in sleep deprivation, increased irritability, difficulties in concentration and memory, heightened anxiety, and a decreased quality of life.
5. Can nightmares in PTSD be treated effectively?
Yes, nightmares in PTSD can be effectively treated. There are various evidence-based treatment approaches, such as cognitive-behavioral therapy (CBT) and eye movement desensitization and reprocessing (EMDR), that have shown success in reducing the frequency and intensity of nightmares.
6. Are nightmares in PTSD a sign of poor prognosis?
While nightmares in PTSD can be distressing, their presence does not necessarily indicate a poor prognosis. With appropriate treatment and support, individuals with nightmares in PTSD can achieve significant improvements in their overall well-being and symptom management.
7. Are there any medications specifically prescribed for nightmares in PTSD?
There are no medications specifically approved for treating nightmares in PTSD. However, some medications, such as certain antidepressants and prazosin, may be prescribed off-label to help reduce nightmare frequency and improve sleep quality.
8. Can self-help strategies be effective in managing nightmares in PTSD?
Yes, self-help strategies can be effective in managing nightmares in PTSD. Techniques such as maintaining a consistent sleep schedule, creating a relaxing bedtime routine, and engaging in relaxation techniques like deep breathing or meditation can help promote better sleep and reduce the occurrence of nightmares.
9. Are nightmares in children with PTSD different from those in adults?
Nightmares in children with PTSD may manifest differently from those in adults. Children may have nightmares that incorporate elements of their trauma, but they can also have more general nightmares that reflect their fears and anxieties. Addressing nightmares in children requires age-appropriate interventions and parental support.
10. Can learning more about nightmares help reduce their impact on individuals with PTSD?
Yes, learning more about nightmares and their connection to PTSD can help individuals with PTSD gain a better understanding of their experiences. This knowledge can empower them to seek appropriate treatment, develop coping strategies, and engage in self-care practices that can reduce the impact of nightmares on their daily lives and overall well-being.