Nightmares and sleep disorders can be incredibly distressing and disruptive to our overall well-being. They can leave us feeling exhausted, anxious, and unable to function at our best. Fortunately, there are various medication options available that can help alleviate the symptoms associated with these conditions. In this article, we will explore the causes of nightmares, the impact they have on our sleep, and the different types of medication that can be used to treat them. Additionally, we will discuss common sleep disorders and their relationship to nightmares. We will also examine the role of medication in treating sleep disorders and explore alternative approaches and lifestyle changes that can help improve our sleep quality.
Understanding Nightmares
Understanding Nightmares can provide valuable insights into the causes and effects of these disturbing experiences. Nightmares are intense, vivid, and often terrifying dreams that can jolt a person awake in a state of fear or anxiety. They can occur during any stage of sleep but are most commonly associated with Rapid Eye Movement (REM) sleep. Causes of Nightmares can vary and may include factors such as stress, trauma, medications, or underlying mental health conditions. Additionally, certain foods, sleep disorders, and lifestyle factors like poor sleep hygiene can contribute to the occurrence of nightmares. It is important to note that nightmares serve a purpose in our psychological well-being, allowing us to process and cope with emotional concerns and fears. While occasional nightmares are a normal occurrence, when they become frequent or prolonged, they can significantly impact our quality of sleep and overall well-being. To learn more about the science behind nightmares, check out our article on the science of lucid dreaming and nightmares. Also, sleep deprivation can have a profound impact on the frequency and content of nightmares, as explored in our article on sleep deprivation and its impact on nightmares and dreams. Additionally, some individuals may experience sleep paralysis, a temporary inability to move or speak while falling asleep or waking up. To learn more about this phenomenon, read our article on understanding sleep paralysis.
1.1 Causes of Nightmares
Causes of Nightmares can vary from person to person and can be influenced by various factors. One common cause is emotional distress or trauma. When individuals experience significant emotional events or undergo traumatic experiences, it can manifest in their dreams as nightmares. This can include events such as accidents, natural disasters, war, or personal loss. Stress is also a significant contributor to nightmares. Daily stressors, such as work pressures, relationship difficulties, or financial problems, can result in heightened arousal levels during sleep, leading to nightmares. Additionally, certain medications can also cause nightmares as a side effect. Medications such as antidepressants, antipsychotics, and beta blockers have been associated with an increased likelihood of experiencing nightmares. Specific substances like alcohol and recreational drugs can disrupt the sleep cycle and contribute to vivid and disturbing dreams. Some medical conditions, such as sleep disorders like sleep apnea or restless legs syndrome, can disrupt sleep and increase the occurrence of nightmares. It is essential to identify and address the underlying causes of nightmares to effectively manage them. If you suspect that a specific medication is contributing to your nightmares, consult your healthcare provider to discuss potential alternatives.
1.2 Impact of Nightmares on Sleep
The impact of nightmares on sleep can be significant and far-reaching. When individuals experience frequent nightmares, it can disrupt their sleep patterns and lead to poor sleep quality. Nightmares can cause individuals to wake up suddenly, often in a state of fear or distress, making it difficult for them to fall back asleep. This can result in fragmented sleep and reduce the amount of time spent in restorative sleep stages. As a consequence, individuals may wake up feeling tired, groggy, and unrested. The emotional intensity and content of nightmares can create a state of anxiety or dread around bedtime, leading to a fear of falling asleep. This anticipation of nightmares can perpetuate a cycle of sleep disruption and anxiety, further exacerbating the negative impact on sleep. The cumulative effects of sleep disturbances due to nightmares can have detrimental effects on daytime functioning, including decreased concentration, impaired memory, mood disturbances, and reduced overall quality of life. Addressing the impact of nightmares on sleep is crucial to promote restful sleep and overall well-being.
Sleep Disorders: An Overview
Sleep Disorders: An Overview
Sleep disorders are a group of conditions that affect the quality, timing, and duration of sleep. These disorders can have a significant impact on a person’s overall well-being and daily functioning. Here, we will provide an overview of some common sleep disorders and explore their relationship with nightmares.
Common Sleep Disorders
1. Insomnia: Insomnia is characterized by difficulty falling asleep, staying asleep, or experiencing non-restorative sleep. It can be caused by various factors such as stress, anxiety, medication, or underlying medical conditions.
2. Sleep Apnea: Sleep apnea is a disorder that causes pauses in breathing during sleep. These pauses can occur multiple times throughout the night and disrupt the natural sleep cycle. It can lead to excessive daytime sleepiness, fatigue, and increased risk of cardiovascular problems.
3. Restless Legs Syndrome (RLS): RLS is a condition characterized by an irresistible urge to move the legs, often accompanied by uncomfortable sensations such as tingling or crawling. Symptoms are typically worse at night and can greatly disrupt sleep.
4. Narcolepsy: Narcolepsy is a neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. It causes excessive daytime sleepiness, sudden and uncontrollable episodes of sleep, and in some cases, loss of muscle tone (cataplexy).
Relationship between Sleep Disorders and Nightmares
Sleep disorders and nightmares often coexist and can exacerbate each other. For example, individuals with insomnia may have difficulty falling asleep, leading to increased anxiety and an elevated risk of experiencing nightmares. Sleep apnea, characterized by disrupted breathing during sleep, can cause frequent awakenings and fragmented sleep, potentially triggering more frequent nightmares.
Similarly, conditions like RLS or narcolepsy can interfere with the normal sleep architecture, leading to disturbances in REM sleep, the stage most closely associated with dreaming and nightmares. These disruptions in sleep patterns can contribute to the development or exacerbation of nightmares.
Understanding the connection between sleep disorders and nightmares is essential for developing effective treatment strategies. By addressing the underlying sleep disorder, it is possible to minimize the occurrence of nightmares and improve overall sleep quality.
2.1 Common Sleep Disorders
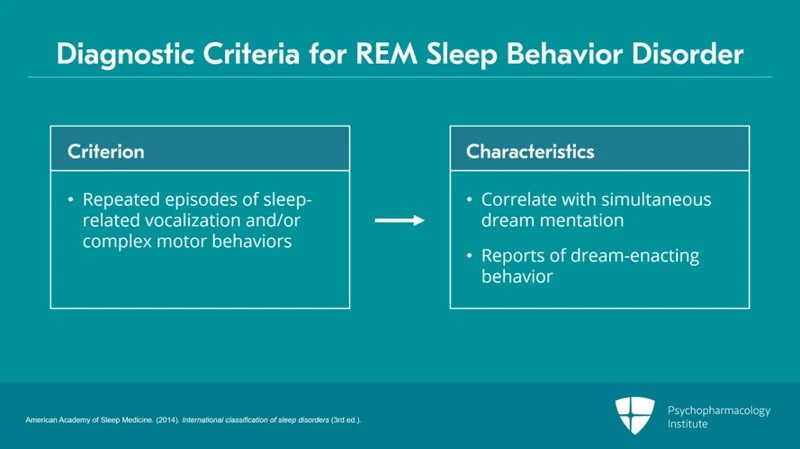
Common Sleep Disorders encompass a range of conditions that can significantly disrupt our sleep patterns and overall quality of rest. One of the most prevalent sleep disorders is insomnia, which refers to difficulty falling asleep or staying asleep throughout the night. Insomnia can be caused by various factors, including stress, anxiety, certain medications, or underlying medical conditions. Another common sleep disorder is sleep apnea, a condition characterized by episodes of interrupted breathing during sleep. Sleep apnea can lead to frequent awakenings and daytime sleepiness. Restless Leg Syndrome (RLS), another prevalent sleep disorder, is characterized by an irresistible urge to move the legs, often accompanied by uncomfortable sensations. This movement can disrupt sleep and make it challenging to fall asleep or stay asleep. A lesser-known sleep disorder is narcolepsy, which involves excessive daytime sleepiness and sudden sleep attacks during the day. Narcolepsy can also lead to cataplexy, a sudden loss of muscle tone triggered by strong emotions. Lastly, parasomnias, such as sleepwalking or night terrors, can disrupt sleep and cause individuals to engage in unusual behaviors during sleep. Understanding the different types of sleep disorders and their impact on sleep is crucial in finding appropriate treatment approaches.
2.2 Relationship between Sleep Disorders and Nightmares
The relationship between sleep disorders and nightmares is complex and interconnected. Sleep disorders can contribute to the occurrence of nightmares, while nightmares can also exacerbate sleep disorders. Let’s explore this relationship further.
Insomnia: Insomnia is a common sleep disorder characterized by difficulty falling asleep, staying asleep, or waking up too early. Individuals with insomnia often experience fragmented and disrupted sleep, which can increase the likelihood of nightmares. The anxiety and stress associated with insomnia can also contribute to the content and intensity of nightmares.
Sleep Apnea: Sleep apnea is a sleep disorder characterized by interrupted breathing during sleep. It can lead to fragmented sleep and frequent awakenings throughout the night. These disruptions in sleep can contribute to the occurrence of nightmares. Additionally, the fear and anxiety associated with sleep apnea, such as choking or gasping for breath, can manifest in nightmares.
Restless Legs Syndrome (RLS): RLS is a condition characterized by uncomfortable sensations in the legs, often accompanied by an irresistible urge to move them. This can lead to difficulty falling asleep and maintaining a restful sleep. The discomfort and restlessness associated with RLS may influence the content and frequency of nightmares.
Narcolepsy: Narcolepsy is a neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. It is characterized by excessive daytime sleepiness, sudden loss of muscle tone (cataplexy), and hallucinations. The hallucinations experienced during narcolepsy, particularly during episodes of sleep paralysis, can be vivid and frightening, resembling nightmares.
Post-Traumatic Stress Disorder (PTSD): PTSD is a mental health condition that can develop after experiencing or witnessing a traumatic event. Nightmares are a common symptom of PTSD and often revolve around the traumatic event. The nightmares can be so distressing that individuals may fear falling asleep or experience sleep disturbances such as insomnia.
The relationship between sleep disorders and nightmares is bidirectional. Sleep disorders can increase the likelihood of experiencing nightmares, while nightmares can disrupt sleep and worsen the symptoms of sleep disorders. Understanding this relationship is crucial in developing effective treatment plans that address both the underlying sleep disorder and the associated nightmares.
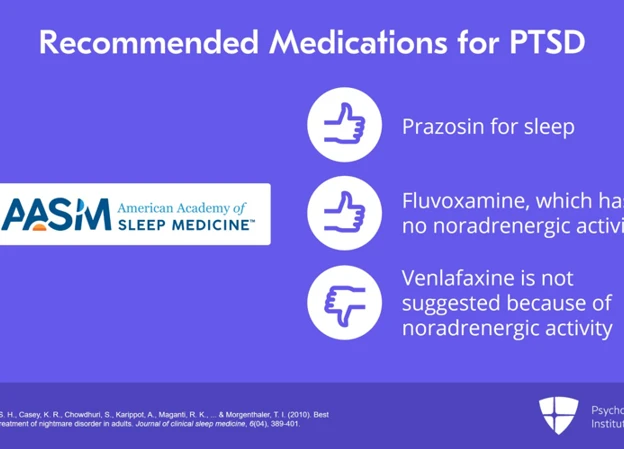
The Role of Medication in Treating Nightmares

The Role of Medication in Treating Nightmares is an important aspect of managing these distressing dreams and improving sleep quality. There are different types of medication available that can help reduce the frequency and intensity of nightmares. Types of Medication for Nightmares may include antidepressants, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors (SNRIs), which can regulate neurotransmitters in the brain and reduce the occurrence of nightmares. Another medication commonly used for nightmares is prazosin, an alpha-blocker that helps decrease adrenaline levels and manage symptoms of post-traumatic stress disorder (PTSD) and associated nightmares. Other medications like clonidine, atypical antipsychotics, and anti-anxiety medications may also be prescribed in certain cases. How Medication Helps Reduce Nightmares can vary depending on the specific medication being used. SSRIs and SNRIs, for example, can help regulate serotonin levels in the brain, which can improve mood stability and reduce the occurrence of nightmares. Prazosin works by blocking adrenaline receptors, preventing the brain from entering the “fight or flight” response during sleep, thus reducing the intensity of nightmares. While medication can be an effective treatment for nightmares, it is important to understand that it may not be suitable for everyone. Consulting with a healthcare professional is crucial to determine the most appropriate medication and dosage for an individual’s specific needs. It is also important to note that medication is often used as part of a comprehensive treatment plan that may include therapy, lifestyle changes, and other interventions to address underlying causes of nightmares.
3.1 Types of Medication for Nightmares
There are different types of medication available to help in the treatment of nightmares. One type of medication commonly prescribed is selective serotonin reuptake inhibitors (SSRIs). SSRIs are primarily used as antidepressants, but they can also help reduce the frequency and intensity of nightmares. They work by increasing the levels of serotonin in the brain, which is thought to regulate mood and sleep. Examples of SSRIs include fluoxetine (Prozac), sertraline (Zoloft), and paroxetine (Paxil).
Another type of medication that may be used to treat nightmares is prazosin. Prazosin is an alpha-1 blocker typically prescribed to treat high blood pressure, but it has shown efficacy in reducing nightmares. It works by blocking adrenaline receptors in the brain, decreasing overall arousal levels and preventing nightmares from occurring.
Anticonvulsant medications such as topiramate (Topamax) and gabapentin (Neurontin) may also be prescribed to help reduce nightmares. These medications work by stabilizing brain activity, which can help prevent the occurrence of vivid and distressing dreams.
It is important to consult with a healthcare provider before starting any medication for nightmares. They can assess your individual situation and determine the most appropriate medication for your specific needs. They will also consider potential interactions with other medications and any underlying medical conditions that may affect treatment options.
3.2 How Medication Helps Reduce Nightmares
Medication can be a helpful tool in reducing nightmares and improving the quality of sleep. Different types of medication may be prescribed based on the underlying causes and severity of the nightmares. One commonly prescribed medication is Selective Serotonin Reuptake Inhibitors (SSRIs). SSRIs work by increasing the levels of serotonin in the brain, which can help regulate mood and reduce the occurrence and intensity of nightmares. Another type of medication that may be prescribed is Prazosin, which is an alpha blocker commonly used to treat high blood pressure. Prazosin has been found to be effective in reducing nightmares, particularly in individuals with post-traumatic stress disorder (PTSD). This medication works by blocking certain receptors that are involved in the regulation of blood pressure and stress responses, which can help decrease the frequency and intensity of nightmares. Other medications such as Beta Blockers and Antidepressants may also be prescribed in certain cases to help reduce nightmares. It is important to note that the use of medication should always be discussed with a healthcare professional, as they can assess individual needs and recommend the most appropriate treatment options. Additionally, medication should be used in conjunction with other therapeutic interventions such as counseling or therapy to address any underlying psychological factors contributing to the nightmares.
3.3 Possible Side Effects of Medication
When considering medication for treating nightmares, it is important to be aware of the possible side effects that may accompany these medications. While medication can be effective in reducing nightmares, it is crucial to weigh the benefits against the potential risks. Some common side effects of these medications include:
1. Drowsiness: Certain medications may cause drowsiness or sedation, which can impact daytime functioning and productivity. It is advisable to take these medications before bedtime to minimize daytime drowsiness.
2. Nausea and Upset Stomach: Some individuals may experience gastrointestinal discomfort, such as nausea, vomiting, or stomach pain, as a side effect of certain medications. It is important to discuss any persistent or severe gastrointestinal symptoms with a healthcare professional.
3. Dizziness and Balance Issues: Certain medications may cause dizziness or affect balance, increasing the risk of falls or accidents. It is crucial to exercise caution while engaging in activities that require coordination and balance.
4. Headache: Headaches can occur as a side effect of some medications. If headaches persist or worsen, it is important to consult a healthcare professional.
5. Changes in Mood or Behavior: In some cases, medication may cause changes in mood, including irritability, agitation, or mood swings. If these changes are severe or persistent, it is essential to seek medical advice.
6. Weight Changes: Certain medications may lead to weight gain or weight loss. Monitoring changes in weight and discussing them with a healthcare professional is recommended.
7. Allergic Reactions: While rare, some individuals may experience allergic reactions to certain medications. Symptoms may include rash, itching, swelling, or difficulty breathing. In the case of any allergic reaction, immediate medical attention should be sought.
It is important to remember that these are potential side effects, and not everyone will experience them. The severity and occurrence of side effects can vary from person to person. It is crucial to discuss any concerns or side effects with a healthcare professional for appropriate guidance and management.
Medication for Sleep Disorders
Medication for Sleep Disorders plays a vital role in managing the symptoms and improving the quality of sleep for individuals suffering from various sleep disorders. There are different types of medication that may be prescribed based on the specific sleep disorder and its underlying causes. Types of Medication for Sleep Disorders include benzodiazepines, non-benzodiazepine hypnotics, melatonin agonists, and tricyclic antidepressants. Benzodiazepines, such as diazepam and lorazepam, are commonly prescribed for short-term treatment of insomnia. Non-benzodiazepine hypnotics, such as zolpidem and eszopiclone, are designed to induce sleep and promote longer periods of sleep. Melatonin agonists, such as ramelteon and tasimelteon, work by regulating the sleep-wake cycle and are often prescribed for individuals with circadian rhythm disorders. Tricyclic antidepressants, such as amitriptyline and doxepin, can be prescribed for individuals with insomnia or other sleep-related disorders. Benefits of Medication for Sleep Disorders can include improvement in sleep quality, reduction in sleep latency, increased total sleep time, and decreased awakenings throughout the night. These medications help regulate sleep patterns and promote a more restful and rejuvenating sleep experience. It is essential to consult with a healthcare professional before starting any medication for sleep disorders, as there may be potential risks and considerations involved. To learn more about alternative approaches and lifestyle changes that can complement medication for sleep disorders, check out our article on alternative approaches to nightmares and sleep disorders.
4.1 Types of Medication for Sleep Disorders
When it comes to treating sleep disorders, there are various types of medication that can be prescribed to help improve sleep quality. Here are some of the most common types of medication used for sleep disorders:
1. Sedative-Hypnotics: These medications, such as benzodiazepines and non-benzodiazepines, work by depressing the central nervous system, promoting relaxation and drowsiness. They can help individuals fall asleep faster and stay asleep longer.
2. Melatonin Agonists: Melatonin is a hormone that regulates sleep-wake cycles. Melatonin agonists, like ramelteon, mimic the effects of this hormone, helping to regulate sleep patterns. They are often used for insomnia.
3. Antidepressants: Certain antidepressant medications, such as tricyclic antidepressants and selective serotonin reuptake inhibitors (SSRIs), can also be effective in treating sleep disorders. They can help regulate sleep patterns and improve overall sleep quality.
4. Antipsychotics: In some cases, antipsychotic medications may be prescribed to individuals with sleep disorders, particularly those with underlying mental health conditions that contribute to disrupted sleep.
5. Stimulants: While stimulants may seem counterintuitive for treating sleep disorders, they can be prescribed in specific cases. These medications, such as modafinil, are used to combat excessive daytime sleepiness associated with conditions like narcolepsy.
It’s important to note that the choice of medication will depend on the specific sleep disorder and individual needs. Consulting with a healthcare professional is essential to determine the most appropriate medication for each individual case. Additionally, medications should always be used under medical supervision to monitor for any potential side effects or interactions with other medications.
4.2 Benefits of Medication for Sleep Disorders
Medication can offer numerous benefits in treating sleep disorders and improving quality of sleep. Benefits of Medication for Sleep Disorders include the potential to regulate sleep patterns, reduce the frequency and intensity of symptoms, and promote a more restful and rejuvenating sleep. Different types of medication target specific sleep disorders, such as insomnia, sleep apnea, and restless legs syndrome, among others. For insomnia, medications like benzodiazepines and non-benzodiazepine sedative-hypnotics can help induce sleep and increase sleep duration. They can also help individuals fall back asleep if they wake up during the night. Sleep apnea, a condition characterized by interrupted breathing during sleep, may be treated with continuous positive airway pressure (CPAP) machines or oral appliances that help keep the airway open. Medications for restless legs syndrome, which causes an overwhelming urge to move the legs during rest, may include dopamine agonists or anticonvulsants to reduce symptoms. The benefits of medication can vary depending on the individual and the specific sleep disorder being treated. It is important to work with a healthcare professional to determine the most appropriate medication and dosage for one’s sleep disorder, taking into consideration factors such as medical history, potential side effects, and drug interactions.
4.3 Risks and Considerations of Medication
When considering medication for sleep disorders, it is important to carefully evaluate the potential risks and considerations involved. While medication can be effective in managing sleep disorders, there are certain factors to keep in mind. One significant consideration is the possibility of side effects. Different medications may have different side effects, ranging from mild to severe. Common side effects of sleep disorder medications include drowsiness, dizziness, headache, and gastrointestinal issues. It is essential to discuss these potential side effects with a healthcare professional to assess their potential impact on daily functioning.
Another consideration is the risk of dependency or addiction. Some sleep disorder medications, particularly those in the benzodiazepine or sedative-hypnotic class, have the potential for dependency. Prolonged use or misuse of these medications can lead to tolerance, meaning higher doses may be required to achieve the same effect, increasing the risk of addiction. Careful monitoring by a healthcare professional is crucial to ensure the appropriate use of these medications to minimize the risk of dependency.
Additionally, medication may interact with other substances or medications. It is important to disclose all current medications, including over-the-counter drugs and supplements, to a healthcare professional before starting any new sleep disorder medication to avoid potential interactions that could have adverse effects.
Finally, it is essential to follow the recommended dosage and duration of medication as prescribed by a healthcare professional. Abruptly stopping medication or altering the dosage without medical guidance can have unintended consequences and may exacerbate sleep disorder symptoms.
Considering these risks and making informed decisions in consultation with a healthcare professional can help ensure the safe and effective use of medication for sleep disorders. It is important to weigh the potential benefits against the potential risks and thoroughly discuss any concerns or questions with a healthcare provider.
Alternative Approaches to Nightmares and Sleep Disorders
Alternative Approaches to Nightmares and Sleep Disorders can provide additional options for individuals who may prefer non-medication strategies or want to complement their medication treatment. Non-Medication Strategies for addressing nightmares and sleep disorders include techniques such as cognitive-behavioral therapy (CBT), imagery rehearsal therapy (IRT), and exposure therapy. CBT can help individuals identify and challenge negative thought patterns and behaviors that contribute to nightmares. IRT involves practicing positive imagery before sleep to create new dream scenarios and reduce the occurrence of distressing nightmares. Exposure therapy gradually exposes individuals to the content of their nightmares in a safe and controlled environment to reduce fear and anxiety associated with specific triggers. These therapies are often conducted by trained professionals such as psychologists or sleep specialists. Additionally, lifestyle changes can play a significant role in improving sleep quality. Creating a soothing bedtime routine, optimizing sleep environment, maintaining a consistent sleep schedule, and avoiding stimulants like caffeine or electronic devices close to bedtime can all contribute to better sleep. Practicing relaxation techniques such as deep breathing exercises, meditation, or yoga can help reduce stress and promote a sense of calm before sleep. It’s important to remember that alternative approaches may vary in effectiveness for different individuals, and it’s always recommended to consult with a healthcare professional for personalized guidance and support.
5.1 Non-Medication Strategies
Non-medication strategies can be effective in managing and reducing nightmares and sleep disorders. Cognitive Behavioral Therapy for Insomnia (CBT-I) is a commonly recommended approach that focuses on identifying and changing negative thought patterns and behaviors related to sleep. This therapy emphasizes relaxation techniques, sleep hygiene practices, and the development of a consistent sleep schedule. Another technique, Imagery Rehearsal Therapy (IRT), involves changing the content and outcome of nightmares through visualization and mental rehearsal. This therapy aims to rewrite the script of the nightmare, transforming it into a more positive and less distressing experience. Progressive Muscle Relaxation (PMR) and Mindfulness-Based Stress Reduction (MBSR) are relaxation techniques that can help reduce stress and promote better sleep. These techniques involve tensing and relaxing specific muscle groups or focusing on the present moment and allowing thoughts to pass without judgment. Additionally, sleep environment optimization can significantly impact sleep quality. This includes creating a comfortable and calming sleep environment, ensuring a cool temperature, minimizing noise and light disturbances, and using relaxation techniques before bedtime. Implementing lifestyle changes such as regular exercise, maintaining a healthy diet, and managing stress can also have a positive impact on sleep. By incorporating these non-medication strategies, individuals can improve their sleep patterns and reduce the occurrence of nightmares and sleep disorders.
5.2 Lifestyle Changes to Improve Sleep
Implementing lifestyle changes can play a significant role in improving sleep quality and reducing the frequency of nightmares. Here are some lifestyle changes that can be beneficial:
1. Establish a consistent sleep routine: Going to bed and waking up at the same time every day, even on weekends, helps regulate your body’s internal clock and promotes better sleep.
2. Create a sleep-friendly environment: Make your bedroom a comfortable and relaxing space by keeping it cool, dark, and quiet. Use earplugs, eye masks, or white noise machines if necessary.
3. Avoid stimulating activities before bed: Limit exposure to screens (such as phones, tablets, and TVs) at least an hour before bedtime, as the blue light emitted by these devices can disrupt your sleep patterns.
4. Practice relaxation techniques: Engage in activities that help you unwind and relax before bed, such as reading a book, taking a warm bath, practicing meditation or deep breathing exercises.
5. Regular exercise: Engaging in moderate-intensity exercise during the day can promote better sleep at night. However, it’s important to avoid exercising too close to bedtime, as it can have a stimulating effect.
6. Manage stress: Stress and anxiety can contribute to sleep disturbances and nightmares. Find healthy coping mechanisms for stress, such as engaging in hobbies, practicing mindfulness, or seeking therapy or counseling.
7. Watch your diet: Avoid consuming heavy meals, caffeine, nicotine, and alcohol close to bedtime, as these substances can disrupt sleep patterns.
8. Create a relaxing bedtime routine: Develop a calming routine before bed, such as listening to soothing music, practicing gentle stretching or yoga, or using aromatherapy with lavender or chamomile scents.
Remember, everyone is different, so it may take some trial and error to find the lifestyle changes that work best for you. By incorporating these adjustments into your daily routine, you can promote better sleep and reduce the occurrence of nightmares.
Conclusion
In conclusion, understanding the role of medication in treating nightmares and sleep disorders can provide relief and improve overall sleep quality. Medication options for nightmares include antidepressants, anti-anxiety medications, and blood pressure medications. These medications work by reducing the intensity and frequency of nightmares, allowing for more restful sleep. However, it is important to note that medication may have possible side effects such as drowsiness, dry mouth, or changes in appetite. It is crucial to work closely with a healthcare professional to find the right medication and dosage that suits individual needs while considering any potential risks. When it comes to sleep disorders, medication can also play a crucial role in managing symptoms. Common medications for sleep disorders include sleeping pills, melatonin supplements, and medications that target specific sleep disorders such as insomnia or sleep apnea. These medications can help regulate sleep patterns, improve sleep quality, and alleviate symptoms associated with sleep disorders. However, it is important to weigh the benefits of medication against any risks or considerations, such as dependency or interactions with other medications. It is also important to explore alternative approaches to managing nightmares and sleep disorders, including non-medication strategies such as cognitive-behavioral therapy, relaxation techniques, and lifestyle changes. These approaches can complement medication or serve as standalone options for those who prefer non-pharmacological interventions. By understanding the unique challenges of nightmares and sleep disorders, individuals can take proactive steps towards achieving better sleep health and overall well-being.
Frequently Asked Questions
1. What is the difference between a nightmare and a bad dream?
A nightmare is a type of bad dream characterized by intense fear or terror that can wake a person up, causing feelings of distress upon awakening. Bad dreams, on the other hand, may be unpleasant but do not typically evoke the same level of fear or anxiety.
2. Can nightmares be a symptom of an underlying sleep disorder?
Yes, nightmares can be a symptom of various sleep disorders, such as sleep apnea, restless leg syndrome, or narcolepsy. It is important to seek professional help if you experience frequent nightmares that disrupt your sleep.
3. Are children more prone to nightmares than adults?
Yes, nightmares are more common in children, particularly between the ages of 3 and 6. This is believed to be related to their active imagination, developing emotional regulation, and the processing of new experiences.
4. Can medication completely eliminate nightmares?
Medication can help reduce the frequency and intensity of nightmares, but it may not completely eliminate them. It is often used as part of a comprehensive treatment plan that may include therapy and lifestyle changes.
5. Are there any natural remedies that can help with nightmares?
Although more research is needed, some natural remedies like relaxation techniques, aromatherapy, and keeping a dream journal may help manage nightmares. However, it is recommended to consult with a healthcare professional before trying any alternative approaches.
6. Do medications for nightmares have any side effects?
Like any medication, those used for nightmares can have potential side effects. These may include drowsiness, dizziness, headache, and gastrointestinal issues. It is essential to discuss potential side effects with your healthcare provider before starting any medication.
7. Can nightmares be a sign of an underlying psychological condition?
Yes, recurrent nightmares can be a symptom of underlying psychological conditions such as post-traumatic stress disorder (PTSD), anxiety disorders, or depression. It is important to seek professional help if nightmares are causing significant distress.
8. Can keeping a consistent sleep schedule help reduce nightmares?
Yes, maintaining a regular sleep schedule, including consistent bedtimes and wake times, can help promote better sleep quality and reduce the occurrence of nightmares. Creating a relaxing pre-sleep routine can also be beneficial.
9. Are there any medications that specifically target nightmares associated with PTSD?
Yes, certain medications, such as prazosin, have been found to be effective in reducing nightmares specifically related to post-traumatic stress disorder (PTSD). They work by blocking certain receptors in the brain associated with nightmares.
10. Should I consult a doctor if nightmares are affecting my daily functioning?
Yes, if nightmares are interfering with your ability to function during the day, it is advisable to consult a healthcare professional. They can evaluate your situation, provide a proper diagnosis, and recommend appropriate treatment options.