Sleep Disorders and Chronic Fatigue Syndrome: Unraveling the Complex Connection
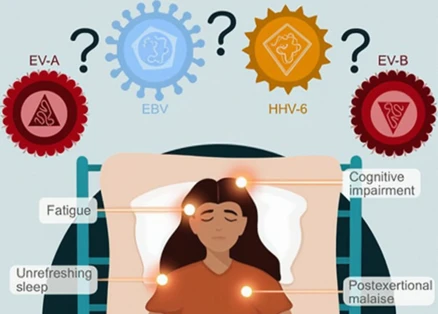
Have you ever experienced the frustration of waking up after a seemingly good night’s sleep, only to find yourself plagued by unrelenting fatigue throughout the day? For individuals with Chronic Fatigue Syndrome (CFS), this exhaustion is a daily battle. But what if we told you that underlying sleep disorders may be amplifying the symptoms of CFS? A growing body of research suggests that there is, indeed, a intricate link between sleep disorders and CFS. In this comprehensive article, we will explore the different types of sleep disorders that often coexist with CFS, delve into the impact of these disorders on CFS symptoms, and discuss strategies and approaches to manage sleep disorders for CFS patients. Get ready to uncover the perplexing relationship between sleep disorders and Chronic Fatigue Syndrome.
The Link: Sleep Disorders and Chronic Fatigue Syndrome
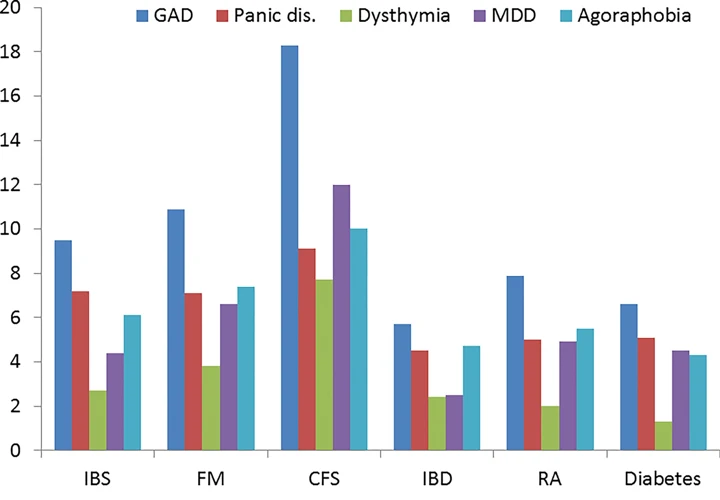
When it comes to Chronic Fatigue Syndrome (CFS), the connection with sleep disorders is undeniably intricate. Research has shown that individuals with CFS are more likely to experience various types of sleep disorders compared to the general population. This link between sleep disorders and CFS raises intriguing questions about the potential role of sleep disturbances in the development and perpetuation of CFS symptoms. Let’s delve into some of the most common sleep disorders that coincide with CFS. Firstly, insomnia<\/strong> can be a major concern for individuals with CFS, causing difficulty falling asleep or staying asleep throughout the night. Secondly, obstructive sleep apnea<\/strong> is another condition that often coexists with CFS, characterized by repeated interruptions in breathing during sleep. This can lead to frequent awakenings and reduced quality of sleep. Lastly, narcolepsy<\/strong>, a neurological disorder that affects the brain’s ability to regulate sleep-wake cycles, can also be seen in conjunction with CFS. Individuals with narcolepsy may experience excessive daytime sleepiness, sudden episodes of sleep, and cataplexy. Exploring the relationship between sleep disorders such as these and CFS sheds light on the complex interplay between sleep and chronic fatigue.
Types of Sleep Disorders
Sleep disorders come in various forms, each with its own unique characteristics and impact on overall well-being. One prevalent sleep disorder is insomnia, which manifests as difficulty falling asleep or staying asleep, leading to persistent fatigue and irritability. Another common sleep disorder is obstructive sleep apnea, where individuals experience interruptions in breathing during sleep, often accompanied by loud snoring and excessive daytime sleepiness. Additionally, narcolepsy is a neurological disorder characterized by sudden bouts of sleepiness, loss of muscle control, and hallucinations. These examples only scratch the surface of the diverse range of sleep disorders that individuals may encounter. By understanding the unique features of each sleep disorder and how they interact with chronic fatigue syndrome, we can begin to unravel the complex relationship between sleep disorders and overall well-being.
Insomnia
Insomnia: Insomnia is a common sleep disorder that can often be found in individuals with Chronic Fatigue Syndrome (CFS). This sleep disorder manifests as difficulty falling asleep, staying asleep, or both. For individuals with CFS, insomnia can be particularly frustrating as it worsens the already debilitating fatigue experienced throughout the day. The relentless cycle of fatigue and insomnia can create a vicious loop, making it challenging for CFS patients to get the restorative sleep they desperately need. In some cases, insomnia may be a primary symptom of CFS, while in others, it may be a consequence of the condition itself. The exact cause of insomnia in individuals with CFS is not fully understood, but it is believed to be related to the dysregulation of the body’s stress response and HPA-axis dysfunction. Individuals with insomnia often report feeling tired, yet unable to fall asleep or stay asleep. This sleep disorder can have significant impacts on various aspects of life, including cognitive function, mood, and overall quality of life. To better understand the relationship between CFS and insomnia, further research is needed to explore the underlying mechanisms and potential treatment options. In the meantime, CFS patients experiencing insomnia may benefit from implementing good sleep hygiene practices, such as maintaining a regular sleep schedule, creating a conducive sleep environment, and practicing relaxation techniques. Additionally, seeking medical advice and exploring potential treatments, such as cognitive-behavioral therapy for insomnia (CBT-I) or medication, can offer relief and support in managing this sleep disorder.
Obstructive Sleep Apnea
Obstructive Sleep Apnea (OSA): A Disturbing Sleep Disorder in the Context of Chronic Fatigue Syndrome<\/strong>
Obstructive Sleep Apnea (OSA) is a common sleep disorder that frequently occurs alongside Chronic Fatigue Syndrome (CFS). This condition is characterized by repeated episodes of partial or complete blockage of the upper airway during sleep, resulting in disrupted breathing patterns. When the airway becomes obstructed, the body’s oxygen levels decrease, leading to sudden awakenings throughout the night. OSA can cause significant sleep fragmentation, preventing individuals from entering deep, restorative sleep stages. The symptoms of OSA, such as loud snoring, gasping for breath, and daytime sleepiness, can exacerbate the fatigue experienced by individuals with CFS. The physiological stress caused by repeated oxygen deprivation can exacerbate other symptoms common in CFS, such as cognitive impairment and muscle pain. Managing OSA in the context of CFS often involves a multi-faceted approach. Continuous Positive Airway Pressure (CPAP) therapy, which involves wearing a mask that delivers a constant flow of air to keep the airway open, is a common treatment for OSA. Lifestyle modifications, including weight loss, avoidance of alcohol and sedatives, and sleep position adjustments, can also help alleviate symptoms. Addressing underlying nasal congestion or structural abnormalities through surgical interventions may be necessary. By recognizing the impact of OSA on CFS symptoms and implementing appropriate management strategies, individuals with CFS can improve their overall sleep quality and potentially alleviate the burden of chronic fatigue.
Narcolepsy
Narcolepsy, a neurological disorder characterized by the brain’s inability to regulate sleep-wake cycles effectively, is one sleep disorder that often coincides with Chronic Fatigue Syndrome (CFS). This condition poses unique challenges for individuals, as it leads to excessive daytime sleepiness and sudden, uncontrollable episodes of falling asleep. These episodes can occur at inappropriate times and in inappropriate places, making it difficult for those with narcolepsy to engage in daily activities. Cataplexy, another characteristic symptom of narcolepsy, involves a sudden loss of muscle tone, often triggered by strong emotions such as laughter or surprise. This can result in temporary muscle weakness or even a complete collapse. The combination of excessive daytime sleepiness and recurrent cataplexy episodes can significantly contribute to the fatigue and general exhaustion experienced by individuals with CFS and narcolepsy. Additionally, sleep paralysis, another phenomenon often associated with narcolepsy, can further exacerbate symptoms. During sleep paralysis, a person is temporarily unable to move or speak while falling asleep or upon waking up, experiencing a brief period of paralysis. This can be an alarming experience and add to the overall disruption of sleep patterns for those with narcolepsy and CFS. Understanding the complexities of narcolepsy within the realm of CFS helps shed light on the intricate relationship between sleep disorders and chronic fatigue. For more information on sleep disorders, such as sleep talking and sleep eating, check out our article on the role of sleep disorders<\/a>.
Impact of Sleep Disorders on Chronic Fatigue Syndrome
The impact of sleep disorders on Chronic Fatigue Syndrome (CFS) cannot be underestimated. For individuals already battling the debilitating symptoms of CFS, the presence of sleep disorders can exacerbate their condition. One significant consequence of sleep disorders in CFS is the increased fatigue and exhaustion<\/strong> experienced by patients. The disrupted sleep and poor sleep quality associated with sleep disorders rob individuals of the restorative rest needed to combat fatigue. These sleep disturbances can lead to a vicious cycle of worsening symptoms, as fatigue begets more fatigue. Additionally, sleep disorders can have a negative impact on cognitive function<\/strong> in CFS patients. Difficulties with concentration, memory, and processing information become more pronounced when sleep is compromised. Lastly, sleep disorders can heighten pain sensitivity<\/strong> in CFS patients, contributing to heightened discomfort and distress. Understanding the multifaceted impact of sleep disorders on CFS highlights the importance of addressing both sleep and chronic fatigue when seeking effective management strategies.
Increased Fatigue and Exhaustion
Increased Fatigue and Exhaustion: One of the significant impacts of sleep disorders on individuals with Chronic Fatigue Syndrome (CFS) is the exacerbation of fatigue and exhaustion. When sleep disorders occur alongside CFS, it creates a vicious cycle where the lack of quality sleep leads to increased fatigue, and this intensified fatigue, in turn, makes it even more challenging to obtain restorative sleep. This cycle perpetuates a constant state of exhaustion. Individuals with CFS and sleep disorders often find themselves trapped in a catch-22 situation, unable to escape the clutches of fatigue. Lack of restful sleep can lead to decreased energy levels, difficulty concentrating, and an overwhelming sense of tiredness that becomes an inherent part of daily life. The impacts of this increased fatigue and exhaustion extend beyond physical discomfort; they can also negatively impact mental health. Sleep deprivation has been linked (anchor: Sleep Deprivation and Mental Health) to issues such as anxiety and depression, further compounding the challenges faced by individuals with CFS and sleep disorders. It is essential for healthcare providers to recognize and address this link between fatigue, sleep disorders, and CFS to develop effective strategies for managing the condition.
Worsening Cognitive Function
Worsening cognitive function is a significant consequence for individuals with Chronic Fatigue Syndrome (CFS) who also experience sleep disorders. The impact of sleep disorders on cognitive function can be profound, exacerbating the cognitive difficulties already associated with CFS. One of the primary cognitive domains affected is memory<\/strong>. Sleep disorders can disrupt the consolidation and retrieval processes of memory, making it challenging for individuals with CFS to retain and recall information. Additionally, attention and concentration are severely affected. Sleep disturbances can lead to decreased focus, impaired concentration, and difficulties in multitasking. The brain’s ability to process information efficiently is compromised, making it harder for individuals to perform daily tasks and maintain productivity. Sleep disorders contribute to brain fog<\/strong>, a commonly reported symptom in CFS. This feeling of mental fogginess and confusion impacts cognitive abilities such as problem-solving, decision-making, and critical thinking. It becomes increasingly challenging for individuals to process information quickly and accurately. The detrimental effects of sleep disorders on cognitive function further emphasize the need for effective management of both CFS and sleep disturbances. However, implementing strategies to improve sleep quality and restore cognitive function can positively impact individuals’ overall quality of life.
Heightened Pain Sensitivity
Heightened pain sensitivity is a significant issue that often accompanies the coexistence of sleep disorders and Chronic Fatigue Syndrome (CFS). Research suggests that individuals with CFS who also experience sleep disorders tend to have an increased sensitivity to pain. This heightened pain sensitivity, known as hyperalgesia, can exacerbate the already debilitating symptoms of CFS. While the exact mechanisms behind this phenomenon are still being studied, it is believed that disrupted sleep patterns and altered neurotransmitter activity play a role. Lack of quality sleep can affect the body’s ability to regulate pain perception, leading to an increased sensitivity to pain stimuli. Sleep deprivation can also contribute to a central sensitization response, causing the brain to interpret non-painful stimuli as painful. The link between heightened pain sensitivity, sleep disorders, and CFS further emphasizes the need for effective management strategies. By addressing and treating sleep disorders, individuals with CFS may experience a reduction in pain sensitivity and an overall improvement in their quality of life. To learn more about coping strategies for sleep-related issues, including sleep paralysis, please visit this informative resource<\/a>.
Managing Sleep Disorders for CFS Patients
When it comes to managing sleep disorders in individuals with Chronic Fatigue Syndrome (CFS), several strategies and approaches can be beneficial. First and foremost, practicing sleep hygiene<\/strong> is essential. This involves maintaining a regular sleep schedule, creating a comfortable sleep environment, avoiding stimulating activities before bed, and establishing a relaxing bedtime routine. Additionally, medical treatments<\/strong> for sleep disorders may include medications to improve sleep quality, such as sedatives for insomnia or continuous positive airway pressure (CPAP) for obstructive sleep apnea. However, it is important to consult with a healthcare professional before starting any medication. For those seeking alternative approaches, techniques like relaxation exercises, cognitive behavioral therapy, or acupuncture may provide relief. Each individual’s experience with CFS and sleep disorders is unique, so it’s essential to find a personalized approach to managing sleep disturbances in the context of Chronic Fatigue Syndrome.
Sleep Hygiene Practices
When it comes to managing sleep disorders in individuals with Chronic Fatigue Syndrome (CFS), implementing good sleep hygiene practices is essential. These practices aim to create a conducive environment and promote healthy habits that can improve the quality and quantity of sleep. Here are some key strategies to consider:
- Establish a regular sleep schedule: Going to bed and waking up at the same time every day, even on weekends, helps regulate the body’s internal clock.
- Create a soothing sleep environment: Keep the bedroom cool, dark, and quiet. Consider using earplugs, eye masks, or white noise machines if necessary.
- Avoid stimulating activities before bed: Limit exposure to screens (e.g., smartphones, tablets, TVs) and engaging in stimulating activities close to bedtime, as they can interfere with the ability to fall asleep.
- Develop a relaxing bedtime routine: Engage in calming activities, such as reading a book, taking a warm bath, or practicing relaxation techniques like deep breathing or meditation.
- Limit daytime napping: If daytime sleepiness is an issue, it’s important to limit napping during the day. If necessary, keep naps short (around 20 minutes) and avoid napping too close to bedtime.
- Avoid consumption of stimulants: Limit or avoid caffeinated beverages, nicotine, and alcohol, as they can disrupt sleep.
- Engage in regular physical activity: Regular exercise can promote better sleep, but it’s important to avoid vigorous exercise close to bedtime, as it can increase alertness.
- Create a comfortable sleep environment: Invest in a comfortable mattress, pillows, and bedding to ensure optimal comfort during sleep.
By incorporating these sleep hygiene practices into daily routines, individuals with CFS can establish healthy sleep habits and potentially improve their sleep quality, which may in turn alleviate some of the symptoms associated with both sleep disorders and CFS.
Medical Treatments
When it comes to managing sleep disorders in individuals with Chronic Fatigue Syndrome (CFS), medical treatments play a crucial role. These treatments are aimed at addressing the underlying sleep disturbances and improving overall sleep quality. Here are some commonly used medical treatments for sleep disorders in CFS patients:
1. Prescription Medications: In certain cases, doctors may prescribe medications to help regulate sleep patterns or address specific sleep disorders. For instance, hypnotic medications may be prescribed to manage insomnia, while stimulant medications can be used to combat excessive daytime sleepiness associated with conditions like narcolepsy.
2. Continuous Positive Airway Pressure (CPAP): For individuals with obstructive sleep apnea, CPAP therapy is often recommended. This treatment involves wearing a mask during sleep that delivers a constant stream of air to keep the airway open, thus preventing interruptions in breathing.
3. Oral Appliances: In some cases of obstructive sleep apnea or other sleep-related breathing disorders, oral appliances may be prescribed. These devices are custom-made to fit the individual’s mouth and work by repositioning the jaw or tongue to keep the airway open during sleep.
4. Light Therapy: Light therapy is a treatment option for individuals with circadian rhythm disorders, such as delayed sleep-wake phase disorder. This therapy involves exposure to bright light, typically in the morning, to help regulate the sleep-wake cycle and promote better sleep at night.
5. Sleep Studies and Diagnostic Testing: Sleep studies, such as polysomnography, can be conducted to assess an individual’s sleep patterns and identify any underlying sleep disorders. These studies involve monitoring various physiological parameters during sleep, including brain activity, breathing patterns, and oxygen levels.
It is important to note that the specific medical treatments prescribed will vary depending on the individual and their specific sleep disorder. Consulting with a healthcare professional who specializes in sleep medicine is essential for accurate diagnosis and personalized treatment plans.
Alternative Approaches
Alternative Approaches: While medical treatments and sleep hygiene practices are commonly prescribed for managing sleep disorders in CFS patients, alternative approaches can also be explored. These alternative approaches aim to address sleep disruptions and alleviate symptoms through natural and holistic means. Here are some alternative approaches that individuals with CFS can consider:
- Acupuncture: This traditional Chinese practice involves the insertion of thin needles into specific points on the body to stimulate the flow of energy. Acupuncture has been suggested as a potential method to improve sleep quality and reduce fatigue in CFS patients.
- Herbal Remedies: Certain herbs, such as valerian root, chamomile, and passionflower, have been used for centuries to promote relaxation and enhance sleep. Herbal remedies can be consumed in the form of teas, capsules, or tinctures, but it’s important to consult with a healthcare professional before incorporating them into your routine.
- Mindfulness and Meditation: Practicing mindfulness and meditation techniques can help calm the mind, reduce stress, and promote better sleep. Techniques such as deep breathing, body scans, and guided imagery can be particularly beneficial for CFS patients struggling with sleep disorders.
- Yoga: Engaging in gentle yoga poses, stretching, and relaxation exercises before bedtime can help relax the body and prepare it for sleep. Yoga not only promotes physical relaxation but also helps calm the mind, making it an effective alternative approach for managing sleep disorders in CFS patients.
It’s important to note that while these alternative approaches have shown promise in some studies, their effectiveness may vary from person to person. It’s always advisable to consult with a healthcare professional or a trained practitioner before embarking on any alternative treatment to ensure safety and appropriateness for individual circumstances.
Conclusion
In conclusion, it is evident that there exists a compelling relationship between sleep disorders and Chronic Fatigue Syndrome (CFS). The coexistence of sleep disorders, such as insomnia, obstructive sleep apnea, and narcolepsy, with CFS highlights the intricate nature of this connection. These sleep disorders can exacerbate the already debilitating symptoms of CFS, including increased fatigue, impaired cognitive function, and heightened pain sensitivity. Managing sleep disorders is crucial for individuals with CFS in order to improve their overall well-being. Implementing proper sleep hygiene practices, seeking medical treatments tailored to specific sleep disorders, and exploring alternative approaches can greatly contribute to alleviating symptoms associated with both sleep disorders and CFS. It is essential for healthcare professionals and individuals with CFS alike to recognize and address the impact of sleep disorders on CFS to provide comprehensive care and support. By unraveling the complex link between sleep disorders and CFS, we can strive towards better understanding and management of this challenging condition.
Frequently Asked Questions
FAQs: Sleep Disorders and Chronic Fatigue Syndrome
1. What is the prevalence of sleep disorders in individuals with Chronic Fatigue Syndrome?
The prevalence of sleep disorders in individuals with Chronic Fatigue Syndrome varies, but studies suggest that a significant portion of CFS patients experience coexisting sleep disturbances, with estimates ranging from 50% to 90%.
2. Can sleep disorders cause Chronic Fatigue Syndrome?
While sleep disorders do not directly cause Chronic Fatigue Syndrome, they can exacerbate the symptoms and contribute to the overall fatigue experienced by individuals with CFS.
3. How does insomnia affect Chronic Fatigue Syndrome?
Insomnia, characterized by difficulty falling asleep or staying asleep, can heighten fatigue levels and worsen other symptoms of Chronic Fatigue Syndrome. Lack of quality sleep further disrupts the already compromised energy levels of CFS patients.
4. Are sleep disorders in Chronic Fatigue Syndrome treatable?
Yes, sleep disorders in individuals with Chronic Fatigue Syndrome can be treated. It is important to properly diagnose the specific sleep disorder and tailor the treatment accordingly, whether through medication, therapy, or other interventions.
5. Can improving sleep quality alleviate Chronic Fatigue Syndrome symptoms?
Improving sleep quality can indeed help alleviate some of the symptoms of Chronic Fatigue Syndrome. By addressing and managing sleep disorders, individuals may experience reduced fatigue, improved cognitive function, and better overall well-being.
6. Is Chronic Fatigue Syndrome a sleep disorder itself?
No, Chronic Fatigue Syndrome is not classified as a sleep disorder. It is considered a complex and debilitating illness characterized by severe fatigue that is not improved by rest and may be worsened by physical or mental activity.
7. Can Chronic Fatigue Syndrome cause sleep paralysis?
While sleep paralysis can occur in individuals with Chronic Fatigue Syndrome, it is not a direct symptom of CFS. Sleep paralysis is more commonly associated with other sleep disorders, such as narcolepsy.
8. Are there lifestyle changes that can help manage sleep disorders in Chronic Fatigue Syndrome?
Yes, adopting healthy sleep hygiene practices, such as maintaining a consistent sleep schedule, creating a comfortable sleep environment, and avoiding stimulants before bedtime, can assist in managing sleep disorders in individuals with Chronic Fatigue Syndrome.
9. What are some alternative approaches to managing sleep disorders in individuals with Chronic Fatigue Syndrome?
Alternative approaches such as relaxation techniques, cognitive-behavioral therapy for insomnia, and acupuncture may be beneficial in managing sleep disorders for individuals with Chronic Fatigue Syndrome. However, it is essential to consult with healthcare professionals before pursuing any alternative treatments.
10. Can proper management of sleep disorders improve the overall quality of life for individuals with Chronic Fatigue Syndrome?
Yes, proper management of sleep disorders can significantly improve the overall quality of life for individuals with Chronic Fatigue Syndrome. By addressing sleep disturbances, individuals may experience reduced fatigue, improved cognitive function, and better overall physical and mental well-being.