When our minds are plagued by the haunting images and intense emotions of nightmares, we often wonder what their significance may be. It turns out that these nighttime terrors are not simply figments of our imagination, but can serve as a window into the deep-seated traumas we may have experienced in our waking lives. In this article, we will delve into the connection between nightmares and trauma, exploring how these unsettling dreams can be linked to past traumatic events. By understanding this connection, we can gain insight into the impact of trauma on our sleep and mental well-being, as well as explore coping strategies and treatment options to help navigate this unsettling terrain. So, fasten your seatbelts as we embark on a journey through the complex labyrinth of nightmares and their ties to trauma.
Nightmares and Trauma: An Overview
Nightmares and trauma share a complex and intertwined relationship. Nightmares, which are intense and distressing dreams that often awaken us from sleep, have been found to have a strong connection to traumatic experiences. Trauma refers to a deeply distressing or disturbing event that has a lasting impact on an individual’s emotional well-being. It can result from various situations such as accidents, natural disasters, abuse, or witnessing violence. Nightmares can serve as a manifestation of the psychological and emotional repercussions of these traumatic events.
There are different types of nightmares, ranging from those that are realistic and recall specific elements of the trauma to more abstract and symbolic dreams that capture the emotional essence of the experience. These nightmares can be vivid and terrifying, often replaying the traumatic event or incorporating elements of it. The intensity and frequency of nightmares may vary depending on the individual, their resilience, and the severity of the trauma they have endured.
Nightmares related to trauma can have a profound impact on an individual’s mental health. They can cause heightened emotional reactions, leading to feelings of fear, anxiety, and distress upon waking. Additionally, trauma-related nightmares can act as triggers, evoking intense emotions and memories associated with the traumatic event.
Recurrent traumatic nightmares, which are characterized by the repeated occurrence of specific nightmares related to the trauma, can be particularly distressing and disruptive to sleep. These nightmares can disrupt the individual’s ability to rest and recharge, leading to sleep disturbances and daytime fatigue. In some cases, recurrent nightmares can be symptomatic of nightmare disorders, such as post-traumatic stress disorder (PTSD), which often co-occurs with trauma.
Understanding the neuroscientific aspects of the nightmare-trauma connection can provide further insights. The amygdala, a key brain structure involved in emotional processing, plays a significant role. Trauma can activate the amygdala, leading to heightened emotional responses and increased vulnerability to nightmares. Sleep disruptions, such as nightmares, can also impair the brain’s ability to process and consolidate memories, which may contribute to the persistence of trauma-related nightmares.
Common themes often emerge in trauma-related nightmares. These themes may include re-experiencing the traumatic event itself, feelings of helplessness and vulnerability, and self-blame or guilt. These themes can reflect the emotional impact of the trauma and the unresolved psychological conflicts associated with it.
While navigating the challenging terrain of trauma-related nightmares can be overwhelming, there are coping strategies and treatment options available to individuals. Implementing self-care techniques, such as maintaining a consistent sleep schedule, creating a relaxing bedtime routine, and engaging in stress-reducing activities, can help manage nightmares and improve sleep quality. Therapy, such as cognitive-behavioral therapy for nightmares (CBT-N), can also be effective in addressing traumatic experiences and their impact on sleep.
Nightmares and trauma are deeply interconnected, with nightmares often serving as a reflection of past traumatic events. Understanding the impact of trauma on nightmares is crucial for both individuals who experience these distressing dreams and healthcare professionals involved in their treatment. By unraveling the complex relationship between nightmares and trauma, we can better comprehend the emotional and psychological toll of traumatic experiences while exploring strategies for healing and bringing about restful sleep.
1. Types of Nightmares
Types of nightmares can vary in terms of their content, intensity, and emotional impact. Understanding these different types can provide insights into the nature and significance of the dreams individuals experience.
1. Realistic Nightmares: Realistic nightmares depict the traumatic event in a detailed and vivid manner. These nightmares often involve reliving aspects of the traumatic experience, including specific scenes, sounds, and emotions. Individuals may wake up feeling distressed and overwhelmed by the realistic portrayal of the trauma.
2. Symbolic Nightmares: Symbolic nightmares, on the other hand, use metaphors and symbolism to represent the underlying emotions and themes associated with the trauma. These dreams may not directly mirror the traumatic event but instead capture its emotional essence. Decoding the symbols and hidden meanings within symbolic nightmares can provide valuable insights into an individual’s psychological state and the unresolved issues related to the trauma.
3. Recurring Nightmares: Recurring nightmares are characterized by the repetition of a specific dream or dream theme. These nightmares may occur frequently and persist over an extended period. They often revolve around the traumatic event, replaying it or incorporating its elements in different variations. Recurring nightmares can be particularly distressing as they contribute to sleep disturbances and can exacerbate the emotional impact of the trauma.
4. Lucid Nightmares: Lucid nightmares occur when individuals become aware that they are dreaming during the nightmare. In a lucid nightmare, individuals may attempt to alter the dream sequence or wake themselves up. While this awareness can provide a sense of control, it can also intensify the emotional experience of the nightmare, making it more challenging to manage.
Recognizing the different types of nightmares can be crucial in understanding their implications for individuals who have experienced trauma. By identifying patterns and themes within nightmares, it becomes possible to gain deeper insights into the emotional processing and psychological impact of the traumatic event. This understanding can inform therapeutic interventions and strategies aimed at addressing and alleviating the distress associated with trauma-related nightmares.
If you want to learn more about preventing nightmares and improving sleep, you can refer to our article on “Preventing Nightmares and Improving Sleep.”
2. Defining Trauma
Defining trauma is essential to understanding its connection with nightmares. Trauma refers to an overwhelmingly distressing or disturbing event that elicits a sense of threat, helplessness, or fear. It can result from various situations, such as physical or sexual abuse, witnessing violence or death, experiencing natural disasters, or being involved in accidents. Traumatic events can have a profound impact on an individual’s mental, emotional, and physical well-being, often causing long-lasting psychological distress. It’s important to note that trauma is a subjective experience, and different individuals may respond differently to similar events.
Trauma can disrupt a person’s sense of safety, stability, and trust in themselves and others. The emotional aftermath of trauma can manifest in various ways, including nightmares. Nightmares act as the mind’s attempt to process and make sense of the traumatic experience. They can feature vivid and distressing imagery, intense emotions, and a feeling of reliving the trauma. It’s crucial to recognize that the experience of trauma varies from individual to individual, and the impact on their mental health and dream life can differ significantly.
Understanding the definition of trauma helps us grasp the significance of its connection to nightmares. Traumatic experiences can deeply affect an individual’s psychological state, leading to an increased likelihood of experiencing nightmares. By exploring this connection, we can gain insight into the intricate relationship between trauma and nightmares, and how addressing trauma is crucial in mitigating the frequency and intensity of these distressing dreams. To learn more about the role of nightmares in processing emotions and memories related to trauma, check out our article on “The Role of Nightmares in Processing Emotions and Memories“. Additionally, being aware of potential warning signs of recurring nightmares is essential in identifying and addressing this connection, as explored in our article “Unveiling the Potential Warning Signs of Recurring Nightmares“.
The Impact of Trauma on Nightmares

The impact of trauma on nightmares is profound, causing various changes in dream patterns and emotional experiences during sleep. Here are several ways trauma can influence nightmares:
1. Heightened Emotional Reactions:
Trauma can lead to heightened emotional reactions in nightmares. Individuals who have experienced trauma may find themselves feeling intense fear, anxiety, or distress during their dreams. These emotions can be so strong that they often wake up feeling a lingering sense of unease or uneasiness. The emotional intensity of nightmares related to trauma serves as a reflection of the deep-seated impact of the traumatic event on the individual’s psyche.
2. Trauma-Triggers in Dreams:
One of the significant impacts of trauma on nightmares is the occurrence of trauma triggers within the dreams themselves. Trauma triggers are elements, such as sounds, images, or situations, that evoke memories or emotional responses associated with the traumatic event. For example, a person who experienced a car accident may have nightmares involving the screeching of brakes or the sound of a collision. These triggers can intensify the emotional experience of the dream and cause a sense of distress upon waking.
3. Recurrent Traumatic Nightmares:
Recurrent traumatic nightmares are a common manifestation of the impact of trauma on sleep. These nightmares involve repetitive themes or scenarios related to the traumatic event, often replaying the experience in different variations. The specific details may differ, but the emotional intensity and distress associated with the trauma remain consistent. Recurrent traumatic nightmares can be disruptive to sleep, leading to frequent awakenings and difficulties in falling back asleep. This, in turn, can contribute to sleep deprivation and daytime fatigue.
4. Nightmare Disorders and PTSD:
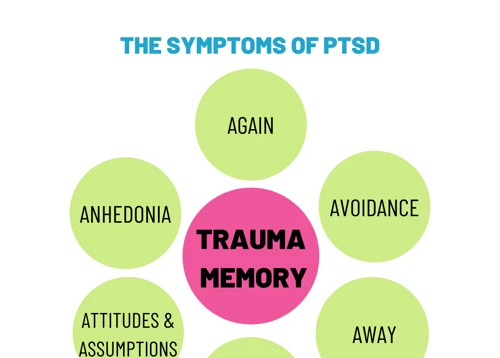
Nightmare disorders can be a direct outcome of trauma, especially in individuals with post-traumatic stress disorder (PTSD). PTSD is a mental health condition that develops after experiencing or witnessing a traumatic event. Nightmares are one of the core symptoms of PTSD and can significantly impact an individual’s quality of life. People with PTSD may experience intrusive and distressing nightmares related to their trauma, contributing to high levels of psychological distress and sleep disturbances.
Understanding the impact of trauma on nightmares is crucial for individuals seeking to heal and improve their sleep quality. Recognizing the emotional intensity, trauma triggers, and the potential for recurrent nightmares can aid in identifying the connection between the traumatic event and the nightmares experienced. By addressing the underlying trauma through therapy and implementing appropriate coping strategies, individuals can work towards reducing the impact of trauma on their nightmares and finding healing and restful sleep.
1. Heightened Emotional Reactions
One of the key effects of trauma on nightmares is the presence of heightened emotional reactions. When individuals experience trauma, it can leave a lasting impact on their emotional well-being. This emotional upheaval often spills over into their dreams, resulting in intense and overwhelming emotional reactions within nightmares.
Trauma-related nightmares are characterized by the exacerbation of emotions such as fear, anxiety, sadness, or anger. These emotions can be so intense that they linger even after waking up, causing distress and disrupting daily life. The vividness and realism of trauma-related nightmares contribute to the potent emotional response they evoke. People may wake up from these nightmares in a state of panic, with their hearts racing and their bodies drenched in sweat.
These heightened emotional reactions can have a profound impact on an individual’s psychological well-being. Nightmares that trigger intense emotions can further reinforce feelings of fear, vulnerability, and helplessness associated with the trauma. The emotional toll of trauma-related nightmares can also lead to increased levels of stress, anxiety, and mood disturbances throughout the day.
To better understand the impact of heightened emotional reactions in trauma-related nightmares, let’s consider an example. Imagine a person who has survived a car accident. In their nightmares, they may find themselves trapped inside a vehicle, reliving the terror and helplessness they felt during the actual event. The emotions of fear and anxiety that overwhelmed them during the accident become magnified within the nightmare, intensifying their emotional response and leaving them feeling emotionally drained upon awakening.
It is important to note that everyone’s experience of trauma and nightmares is unique. Some individuals may experience a wide range of emotions within their nightmares, while others may predominantly feel a specific emotion related to the traumatic event. The nature and intensity of these emotional reactions can vary, depending on factors such as the individual’s coping mechanisms, resilience, and the specific details of the traumatic experience.
Addressing these heightened emotional reactions in trauma-related nightmares is crucial for promoting healing and improved well-being. Techniques such as relaxation exercises, deep breathing, and grounding techniques can help individuals manage their emotional responses to nightmares. Seeking support from loved ones, therapists, or support groups can also provide a safe space to process and express these intense emotions.
By recognizing and addressing the heightened emotional reactions within trauma-related nightmares, individuals can take significant steps towards healing and reclaiming their emotional well-being. Understanding the profound impact of emotions within nightmares allows for the development of targeted coping strategies and therapeutic interventions to help individuals navigate the intricate terrain of trauma-related nightmares.
2. Trauma-Triggers in Dreams
Trauma triggers in dreams are elements or stimuli within a dream that directly connect to the traumatic event or evoke strong emotional responses associated with the trauma. These triggers can range from specific people, places, or objects to sensory experiences or symbolic representations. The presence of trauma triggers in dreams can intensify the emotional impact of nightmares, making them more distressing and vivid. These triggers often reflect the unresolved emotions, fears, and memories deeply ingrained in the individual’s psyche after the traumatic experience.
In some cases, trauma triggers in dreams may closely resemble the actual events or situations that occurred during the traumatic incident. For example, a person who experienced a car accident may have nightmares where they relive the crash, hear screeching tires, or see shattered glass. These realistic depictions in dreams can heighten the emotional distress and anxiety upon waking.
However, trauma triggers in dreams can also manifest in symbolic or metaphorical ways. The subconscious mind may use symbols or abstract representations to capture the essence of the trauma and the associated emotions. For instance, a person who survived a physical assault might have nightmares where they are pursued by an unidentified figure or trapped in confined spaces, symbolizing their fear and helplessness during the traumatic event.
It’s important to note that trauma triggers in dreams can vary for each individual based on their specific experiences and psychological makeup. What may trigger one person’s nightmares may not have the same effect on another. The intensity and frequency of these triggers may also change over time as the individual processes and heals from the trauma.
Recognizing and understanding trauma triggers in dreams can be a crucial step in the healing process. It allows individuals to become more aware of their emotional reactions and apprehensions tied to particular elements or situations in their dreams. By identifying these triggers, individuals can work with mental health professionals to develop coping strategies, such as relaxation techniques, grounding exercises, and exposure therapy, to gradually reduce the distress caused by these triggers.
Addressing trauma triggers in dreams is a significant aspect of therapy for trauma-related nightmares. Therapists trained in trauma-focused approaches, such as eye movement desensitization and reprocessing (EMDR) or cognitive-behavioral therapy (CBT), can guide individuals in processing and reframing the traumatic memories embedded in their dreams. Through these therapeutic interventions, individuals can gradually reduce the emotional intensity of trauma triggers, empowering them to regain control over their dreams and promote emotional healing.
Understanding how trauma triggers manifest in dreams provides us with valuable insights into the complex relationship between nightmares and trauma. By unraveling the specific elements that trigger emotional responses in dreams, individuals can take steps towards healing, resilience, and reclaiming a sense of safety and peace in their sleep and daily lives.
3. Recurrent Traumatic Nightmares
Recurrent traumatic nightmares are a distressing and debilitating aspect of trauma-related sleep disturbances. These nightmares are characterized by the repeated occurrence of specific dreams that are closely tied to the traumatic event. Unlike common nightmares that tend to vary in content and theme, recurrent traumatic nightmares often revolve around the same distressing imagery, emotions, and scenarios associated with the trauma.
These nightmares can be intrusive and vivid, causing intense fear, anxiety, and distress upon waking. The frequency and severity of recurrent traumatic nightmares can vary among individuals, with some experiencing them multiple times a week, while others may have them less frequently but still find them profoundly disturbing.
The impact of these nightmares extends beyond sleep disturbances. They can disrupt an individual’s overall well-being, affecting daytime functioning, quality of life, and mental health. The exhausting nature of recurrent traumatic nightmares can lead to chronic fatigue, irritability, difficulty concentrating, and a heightened sense of hypervigilance.
It’s important to note that recurrent traumatic nightmares are not simply a replaying of the traumatic event itself. While elements of the trauma may be present in the nightmares, the dreams often incorporate symbolic or distorted representations of the experience. These distorted images and themes can capture the emotional essence of the trauma rather than replicating it exactly, making them uniquely personal to each individual.
Addressing recurrent traumatic nightmares requires a comprehensive approach that focuses on both the underlying trauma and the sleep disturbances themselves. Therapeutic interventions such as cognitive-behavioral therapy for nightmares (CBT-N) have shown promise in helping individuals manage and reduce the frequency and intensity of these nightmares.
CBT-N involves identifying and challenging negative thought patterns and beliefs that contribute to the persistence of recurrent traumatic nightmares. By exploring the underlying emotions and meanings attached to the nightmares, individuals can begin to process and heal from the traumatic experiences that fuel these dreams.
In addition to therapeutic interventions, self-care techniques can also play a vital role in managing recurrent traumatic nightmares. Establishing a consistent sleep routine, creating a calm and relaxing sleep environment, and practicing relaxation techniques before bed can promote better sleep and reduce the occurrence of nightmares. Engaging in activities that promote overall well-being, such as exercise, mindfulness, and healthy coping strategies, can also contribute to the reduction of nightmares and improved sleep quality.
While recurrent traumatic nightmares can be deeply distressing, it’s essential to remember that healing is possible. With proper support, therapy, and self-care, individuals can gradually reduce the frequency and intensity of these nightmares, allowing for a more restful and peaceful sleep experience.
4. Nightmare Disorders and PTSD
Nightmare disorders, including those associated with post-traumatic stress disorder (PTSD), are a significant concern for individuals who have experienced trauma. PTSD is a mental health disorder that can develop following a traumatic event, and nightmares are one of its hallmark symptoms.
Nightmares in individuals with PTSD are often vivid and disturbing, causing significant distress and impairing their overall quality of life. These nightmares can be an ongoing re-experiencing of the traumatic event, creating a relentless cycle of fear and anxiety. Nightmares in PTSD can also be different from regular nightmares in terms of content and intensity. They may involve specific and realistic elements of the trauma, with individuals feeling as though they are reliving the event.
It’s important to note that not everyone who experiences trauma develops PTSD or nightmare disorders. However, it is estimated that around 70-80% of individuals with PTSD experience nightmares. The frequency and intensity of nightmares can vary, with some individuals reporting multiple nightmares per night, while others have them less frequently.
Nightmares associated with PTSD can have a significant impact on sleep quality and overall well-being. They can lead to sleep disturbances, causing individuals to feel exhausted and fatigued during the day. The fear and anxiety triggered by these nightmares can also contribute to hypervigilance, avoidance behaviors, and a constant state of alertness, further exacerbating the symptoms of PTSD.
Treatment options are available for individuals with nightmare disorders and PTSD. One effective approach is cognitive-behavioral therapy for nightmares (CBT-N). This therapy focuses on identifying and modifying negative thought patterns and behaviors associated with nightmares. CBT-N may involve techniques such as image rehearsal therapy (IRT), where individuals rewrite the script of their nightmares to create more positive or controllable outcomes. This process can help reduce the frequency and intensity of nightmares, leading to improved sleep quality and a decrease in overall PTSD symptoms.
In addition to therapy, medications may be prescribed to help manage nightmare disorders related to PTSD. These medications can include selective serotonin reuptake inhibitors (SSRIs), which are commonly used to treat anxiety and depression. SSRIs can help regulate sleep patterns and reduce the frequency of nightmares, offering relief to individuals with PTSD.
Nightmare disorders and PTSD are intricately connected, with nightmares being a prevalent symptom of this mental health disorder. Seeking appropriate treatment and support is crucial for individuals who experience these distressing nightmares. Whether through therapy, medication, or a combination of approaches, managing nightmare disorders associated with PTSD can alleviate the emotional burden and improve overall well-being.
Neuroscience and the Nightmare-Trauma Connection
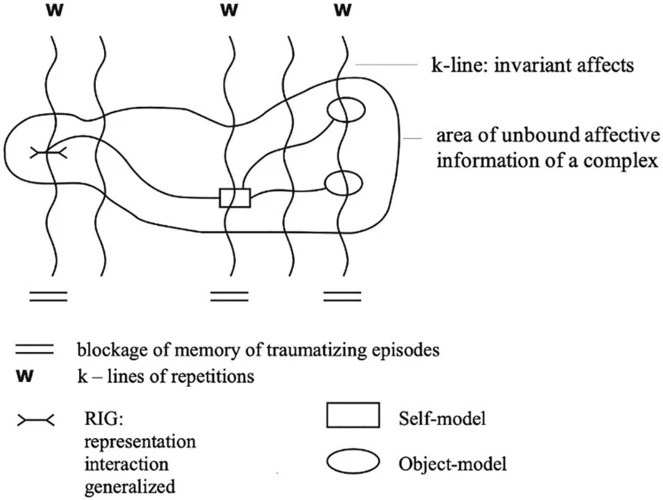
Neuroscience plays a crucial role in understanding the connection between nightmares and trauma. One key aspect of this connection lies in the role of the amygdala, a part of the brain involved in processing emotions and fear responses. In individuals who have experienced trauma, the amygdala can become hypersensitive and overactive, leading to heightened emotional reactions. This hyperactivity can manifest in nightmares, as the amygdala processes the emotional memories associated with the traumatic event, resulting in intense and distressing dreams.
Sleep disruptions also play a significant role in the nightmare-trauma connection. Trauma can disrupt normal sleep patterns, leading to difficulties falling asleep, frequent awakenings, and overall poor sleep quality. Sleep disturbances, in turn, can contribute to the occurrence and persistence of nightmares. During REM (rapid eye movement) sleep, the stage of sleep most closely associated with dreaming, the brain consolidates memories and processes emotions. However, in individuals who have experienced trauma, this process can be disrupted, leading to the consolidation of distressing and fragmented memories, which can manifest as nightmares.
Neuroplasticity, the brain’s ability to adapt and reorganize itself, also plays a role in healing from trauma and its associated nightmares. Through therapeutic interventions and supportive environments, individuals can engage in processes that promote neuroplasticity and facilitate the rewiring of neural pathways associated with trauma. This can lead to a reduction in the occurrence and intensity of nightmares over time.
Understanding the neuroscience behind the nightmare-trauma connection allows researchers and healthcare professionals to develop targeted interventions. For example, therapies such as imagery rehearsal therapy (IRT) can help individuals with trauma-related nightmares by guiding them to imagine alternative, more positive dream scenarios. This technique aims to modify the emotional and cognitive aspects of the nightmares, reducing the distress associated with them.
Additionally, emerging research suggests that certain medications may be effective in treating trauma-related nightmares. These medications, such as prazosin, help regulate the brain’s response to stress by blocking adrenergic receptors, which can reduce nightmare frequency and severity.
By using neuroscience to explore the nightmare-trauma connection, researchers and specialists can gain valuable insights into the underlying mechanisms of these distressing dreams. This knowledge can pave the way for the development of innovative therapeutic approaches and interventions that target specific brain processes and promote healing from trauma-related nightmares. Ultimately, a deeper understanding of the neuroscience behind the nightmare-trauma connection offers hope for individuals seeking relief from the impact of traumatic experiences on their sleep and well-being.
1. The Role of the Amygdala
The amygdala, a small almond-shaped structure deep within the brain, plays a crucial role in the connection between nightmares and trauma. As a key component of the brain’s limbic system, the amygdala is primarily responsible for processing and regulating emotions, especially those related to fear and threat detection. In the context of trauma, the amygdala becomes highly activated, leading to heightened emotional reactions and a heightened sensitivity to potential dangers.
When a traumatic event occurs, the amygdala rapidly assesses the situation and triggers the body’s stress response, also known as the “fight-or-flight” response. This response prepares the body to react to potential threats by releasing stress hormones such as adrenaline and cortisol. In the case of nightmares, the amygdala can continue to be hyperactive, responding as if the trauma is happening again even during sleep.
The heightened activity in the amygdala during both wakefulness and sleep can lead to nightmares that vividly reenact the traumatic event or incorporate its emotional essence. These nightmares often evoke intense fear, anxiety, and distress, leaving individuals feeling overwhelmed and vulnerable. As a result, waking up from these nightmares can be a jarring and unsettling experience.
The amygdala’s involvement in the nightmare-trauma connection goes beyond the dream state. It can also influence the waking state, leading to heightened emotional sensitivity and hyperarousal. Individuals who have experienced trauma may find themselves more easily triggered by reminders or situations resembling aspects of the original trauma. These triggers can evoke intense emotional reactions and contribute to the persistence of nightmares.
Understanding the role of the amygdala in nightmares and trauma can pave the way for potential therapeutic approaches. Techniques that aim to regulate and calm the amygdala’s hyperactivity, such as mindfulness, relaxation exercises, and exposure therapy, can be beneficial in reducing the frequency and intensity of traumatic nightmares. By targeting the amygdala’s response to fear and trauma, it becomes possible to modulate the emotional reactivity associated with nightmares and promote a sense of safety and healing.
The amygdala’s involvement in the nightmare-trauma connection highlights its significance in processing and regulating emotions related to traumatic experiences. Its hyperactivity can lead to increased emotional sensitivity, heightened fear responses, and the manifestation of traumatic nightmares. Recognizing the amygdala’s role opens up avenues for therapeutic interventions that can help individuals find relief from the distressing impact of trauma-related nightmares.
2. Sleep Disruptions and Trauma
Sleep disruptions are a common consequence of trauma and can significantly impact an individual’s overall well-being. When someone has experienced a traumatic event, their sleep patterns may become disrupted, leading to difficulties falling asleep, staying asleep, or experiencing restful sleep. These sleep disturbances can be attributed to the physiological and psychological effects of trauma on the body and mind.
One of the primary reasons for sleep disruptions following trauma is heightened arousal and hypervigilance. Individuals who have experienced trauma often remain on high alert, constantly scanning their surroundings for potential threats. This hypervigilance can make it challenging to relax and fall asleep, as the individual may be constantly expecting danger. As a result, they may experience difficulty initiating sleep or struggle with frequent awakenings throughout the night.
Nightmares can also contribute to sleep disruptions in individuals with a history of trauma. Trauma-related nightmares can be vivid, distressing, and recurrent, causing individuals to wake up abruptly during the night. The fear and anxiety evoked by these nightmares can make it difficult to fall back asleep, prolonging sleep disruptions and leading to fragmented sleep.
Another common sleep disturbance associated with trauma is insomnia. Insomnia can manifest as difficulty falling asleep, staying asleep, or experiencing restorative sleep. Trauma-related insomnia may occur due to the intrusive thoughts, flashbacks, and hypervigilance that often accompany traumatic experiences. The mind remains active and alert, preventing the individual from entering a state of deep and restful sleep.
Sleep disruptions resulting from trauma can have far-reaching consequences on an individual’s physical and mental health. Ongoing sleep disturbances can contribute to chronic fatigue, daytime sleepiness, decreased immune function, and impaired cognitive abilities. Sleep deprivation can exacerbate existing symptoms of trauma, such as difficulty concentrating, irritability, and emotional instability, making it even more challenging for individuals to heal and recover from their traumatic experiences.
Addressing sleep disruptions in individuals with trauma requires a comprehensive approach that acknowledges the interconnectedness of sleep and mental well-being. This may involve implementing relaxation techniques before bedtime, creating a calming sleep environment, and establishing a consistent sleep routine. Cognitive-behavioral therapy for insomnia (CBT-I) can be an effective treatment option, helping individuals reestablish healthy sleep patterns and manage trauma-related sleep disturbances.
It is essential to recognize that sleep disruptions resulting from trauma are a significant aspect of post-traumatic recovery and should be addressed with care and understanding. Supporting individuals in restoring restful sleep can contribute to their overall healing and well-being, allowing them to reclaim a sense of safety, security, and control in their lives. Prioritizing sleep and seeking appropriate treatment can play a vital role in the recovery journey of individuals affected by trauma.
3. Neuroplasticity and Healing from Trauma
Neuroplasticity, the brain’s ability to reorganize and form new connections, plays a crucial role in the process of healing from trauma. Traumatic experiences can profoundly impact the brain, leading to changes in its structure and function. However, research has shown that the brain has the remarkable ability to adapt and recover from such trauma through neuroplasticity.
Neuroplasticity allows the brain to rewire itself by forming new neural pathways and modifying existing ones. This process is essential for healing from trauma. It enables individuals to reframe their thoughts and perceptions, helping them to move from a state of distress to a state of resilience and recovery.
Healing from trauma involves working through and integrating the memories and emotions associated with the traumatic event. Through neuroplasticity, the brain can undergo changes that facilitate this process. Therapy modalities such as Eye Movement Desensitization and Reprocessing (EMDR) and trauma-focused cognitive-behavioral therapy (TF-CBT) leverage neuroplasticity to help individuals process and reframe their traumatic experiences.
During therapy, the brain’s neural networks can be reshaped, enabling individuals to reprocess and make meaning out of their traumatic memories. By establishing new connections and associations, positive changes in emotional regulation and perception of the traumatic event can occur. This process can alleviate the frequency and intensity of trauma-related nightmares, leading to improved sleep quality and overall well-being.
Engaging in activities that promote neuroplasticity, such as mindfulness meditation, exercise, and creative pursuits, can also aid in the healing process. These activities strengthen neural connections, enhance emotional regulation, and promote overall brain health. By actively engaging in these practices, individuals can harness the power of neuroplasticity to promote healing and recovery from trauma.
It is important to note that healing from trauma is a gradual and individualized process. The brain’s capacity for neuroplasticity allows for ongoing growth and adaptation, even long after the traumatic event has occurred. This means that individuals can continue to experience healing and progress on their journey towards recovery.
Harnessing the potential of neuroplasticity in healing from trauma offers hope and empowerment to individuals affected by traumatic experiences. It emphasizes the brain’s capacity for change and the possibility of transforming the negative impact of trauma into a catalyst for growth, resilience, and restoration.
To learn more about the role of neuroplasticity in trauma healing, you can read our comprehensive guide on the subject here.
Common Themes in Trauma-Related Nightmares
Trauma-related nightmares often encompass common themes that reflect the emotional and psychological impact of the traumatic event. These recurring themes can provide insight into the unresolved conflicts and distress experienced by individuals who have endured trauma.
1. Re-Experiencing the Traumatic Event: One of the primary themes in trauma-related nightmares involves the re-experiencing of the traumatic event itself. Individuals may find themselves reliving the details and emotions associated with the trauma, as if they were back in that moment. These nightmares can be vivid and overwhelming, evoking intense fear, helplessness, and distress.
2. Helplessness and Vulnerability: Feelings of helplessness and vulnerability are common themes in trauma-related nightmares. Individuals may find themselves in situations where they are unable to protect themselves or escape danger, mirroring the powerlessness experienced during the traumatic event. These nightmares can intensify feelings of fear and anxiety, further impacting the individual’s sense of security and control.
3. Guilt, Shame, and Self-Blame: Trauma-related nightmares may also involve themes of guilt, shame, and self-blame. Individuals often question their actions or inactions during the traumatic event, blaming themselves for the outcome. These nightmares can be accompanied by overwhelming feelings of guilt and shame, exacerbating the emotional distress associated with the trauma.
It is important to note that the specific themes in trauma-related nightmares can vary depending on the individual’s unique experiences and the nature of the trauma they have endured. Some individuals may have nightmares that closely resemble the actual events, while others may experience more symbolic or abstract dreams that capture the emotional essence of the trauma.
By identifying and understanding these common themes, individuals and healthcare professionals can gain valuable insights into the psychological impact of trauma. Recognizing that trauma-related nightmares often revolve around these themes can help validate individuals’ experiences and provide a starting point for addressing and processing the underlying trauma.
In the next section, we will explore coping strategies and treatment options that can assist individuals in managing trauma-related nightmares and promoting healing from the psychological wounds of trauma.
1. Re-Experiencing the Traumatic Event
Re-experiencing the traumatic event is a common theme in nightmares related to trauma. When individuals have experienced a deeply distressing or traumatic event, their memories and emotions become deeply ingrained in their subconscious. This can lead to the re-emergence of the traumatic event in their nightmares, causing them to relive the experience in a vivid and emotionally charged way.
In these nightmares, individuals may find themselves transported back to the scene of the trauma, witnessing the event unfold as if it were happening in real-time. The details of the event may be reenacted with startling clarity, including the sights, sounds, and sensations associated with the original trauma. This can be incredibly distressing and overwhelming, intensifying feelings of fear, anxiety, and helplessness.
The re-experiencing of the traumatic event in nightmares can serve as a way for the mind to process and make sense of the trauma. It is a manifestation of the unresolved emotions and memories surrounding the event. These nightmares can be particularly disruptive to sleep, often causing individuals to wake up in a state of distress, and making it difficult to fall back asleep.
It is important to note that not everyone who has experienced trauma will re-experience the event in their nightmares. The presence or absence of this theme in nightmares can vary depending on individual factors such as the severity of the trauma, coping mechanisms, and the effectiveness of trauma processing and healing.
Addressing the re-experiencing of the traumatic event in nightmares requires a comprehensive and holistic approach to trauma healing. Therapy modalities, such as trauma-focused therapy or eye movement desensitization and reprocessing (EMDR), can help individuals process their experiences and reduce the frequency and intensity of the re-enactment in their nightmares.
Additionally, practicing self-care techniques to promote a sense of safety and relaxation before sleep can be beneficial. Engaging in relaxation exercises, such as deep breathing or meditation, can help reduce anxiety and create a more peaceful mindset before bed. Creating a comforting sleep environment, such as using dim lighting, soothing scents, or relaxing music, can also contribute to a sense of security and aid in minimizing re-experiencing in nightmares.
By acknowledging and addressing the theme of re-experiencing the traumatic event in nightmares, individuals can begin the process of healing and working towards a healthier relationship with sleep. It is through this healing journey that they can gradually reduce the distress associated with these nightmares and regain a sense of control and peace in their lives.
2. Helplessness and Vulnerability
In trauma-related nightmares, themes of helplessness and vulnerability often emerge, reflecting the emotional impact of the traumatic event. These nightmares can evoke a sense of powerlessness, where the dreamer feels unable to escape or defend themselves against the threat presented in the dream. The feelings of helplessness can be overwhelming and create a sense of fear and anxiety even after waking up.
One common manifestation of helplessness in these nightmares is the feeling of being chased or pursued by an unknown or faceless entity. The dreamer may experience difficulty running or moving, highlighting their perceived lack of control in the situation. This sense of vulnerability can also manifest in dreams where the dreamer finds themselves in dangerous or life-threatening situations, without the ability to protect themselves or seek help.
Trauma-related nightmares may depict the dreamer being trapped, held captive, or restrained in some way. These dreams serve as metaphors for the individual’s emotional state, symbolizing the feeling of being trapped in the trauma or unable to break free from its effects. The vulnerability experienced in these nightmares can be a reflection of the powerlessness and loss of control that may accompany a traumatic experience.
It is important to note that these themes of helplessness and vulnerability in nightmares do not define the individual’s strength or resilience in waking life. Rather, they are a representation of the deep-rooted emotions and psychological conflicts associated with the trauma. Processing and understanding these themes can be an essential step towards healing and moving forward.
To cope with the feelings of helplessness and vulnerability experienced in trauma-related nightmares, individuals can explore various techniques. One effective approach is to engage in therapy, particularly cognitive-behavioral therapy for nightmares (CBT-N). This therapy focuses on identifying and challenging negative thoughts, emotions, and beliefs associated with the trauma and its impact on nightmares. CBT-N can help individuals regain a sense of control, develop coping strategies, and work towards reducing the distress caused by these nightmares.
Additionally, practicing self-care techniques can provide a sense of empowerment and support. This may include engaging in relaxation exercises, such as deep breathing or meditation, to reduce anxiety and promote a sense of calm. Establishing a safe and comforting sleep environment can also contribute to a feeling of security and reduce the occurrence of nightmares.
By addressing the themes of helplessness and vulnerability within trauma-related nightmares, individuals can begin to regain control over their dreams and their emotional well-being. Recognizing that these dreams are a reflection of the trauma and utilizing coping strategies can facilitate the healing process and promote a sense of empowerment in overcoming the effects of the traumatic experience.
3. Guilt, Shame, and Self-Blame
Guilt, shame, and self-blame are common themes that frequently emerge in trauma-related nightmares. When individuals have experienced a traumatic event, they may internalize feelings of guilt, believing that they are somehow responsible for what happened to them. These feelings can be overwhelming and may manifest in nightmares, causing distress and perpetuating negative self-perception.
In these nightmares, individuals may find themselves reliving the traumatic event and experiencing a deep sense of guilt for their perceived role in it. They may imagine alternative scenarios where they could have prevented or changed the outcome, amplifying their feelings of responsibility. These dreams can be intense and emotionally charged, with individuals waking up feeling burdened by guilt and self-blame.
Shame is another powerful emotion that can be intertwined with guilt and self-blame in trauma-related nightmares. Individuals may feel a deep sense of shame about the traumatic event itself or about their own reactions and responses during the event. This shame can seep into their dreams, leading to nightmares filled with humiliation, public exposure, or a sense of being fundamentally flawed. These nightmares can exacerbate feelings of shame and reinforce negative self-perception.
The cycle of guilt, shame, and self-blame can be relentless, as individuals may struggle to make sense of the traumatic experience and assign blame either to themselves or others involved. These emotions can have a lasting impact on their mental well-being, contributing to depression, anxiety, and low self-esteem.
It is important for individuals experiencing trauma-related nightmares characterized by guilt, shame, and self-blame to understand that these emotions are a common response to trauma. Recognizing that guilt and self-blame are often misplaced and part of the natural coping process can be a crucial step towards healing. Seeking therapy or counseling can provide a safe and supportive environment to explore these complex emotions, challenge negative self-perceptions, and develop healthier frameworks for self-understanding and forgiveness.
In therapy, techniques such as cognitive restructuring and self-compassion exercises can help individuals challenge their distorted beliefs and develop a more balanced perspective. By reframing the traumatic event and their role in it, individuals can begin to let go of the burden of guilt and shame. It is important to emphasize that healing from trauma is a journey, and it takes time, patience, and support.
By addressing the themes of guilt, shame, and self-blame in trauma-related nightmares, individuals can begin to untangle the complex web of emotions associated with their traumatic experiences. Recognizing that these feelings are a normal response to trauma and seeking appropriate treatment can pave the way for healing, self-forgiveness, and ultimately, a restoration of mental well-being.
Coping Strategies and Treatment Options
Coping with trauma-related nightmares requires a multi-faceted approach that combines effective coping strategies and appropriate treatment options. Here are some strategies and interventions individuals can consider:
1. Self-Care Techniques for Nightmares:
Taking care of oneself can play a significant role in managing trauma-related nightmares. Some self-care techniques include:
– Establishing a consistent sleep schedule: Maintaining a regular sleep routine can help regulate your body’s internal clock and promote better sleep.
– Creating a relaxing bedtime routine: Engaging in activities that promote relaxation, such as taking a warm bath, practicing deep breathing exercises, or reading a calming book before bed, can signal to your body that it is time to wind down.
– Creating a comfortable sleep environment: Making your sleep environment conducive to restful sleep by ensuring it is dark, quiet, and at a comfortable temperature can minimize disruptive factors that may contribute to nightmares.
– Practicing stress-reducing activities: Engaging in stress-reducing activities during the day, such as mindfulness exercises, yoga, or engaging in hobbies, can help lower overall stress levels and promote better sleep at night.
2. Therapy and Trauma Healing:
Seeking professional therapy can assist individuals in addressing the underlying trauma and managing trauma-related nightmares. Some therapy approaches commonly used include:
– Cognitive-Behavioral Therapy (CBT): CBT aims to identify and challenge negative thoughts and beliefs related to trauma, helping individuals develop healthier coping mechanisms and reduce the frequency and intensity of nightmares.
– Eye Movement Desensitization and Reprocessing (EMDR): EMDR combines techniques from CBT with bilateral stimulation, such as eye movements or alternating audio tones, to help individuals process traumatic memories and reduce symptoms associated with trauma.
– Imagery Rehearsal Therapy (IRT): IRT involves modifying the content of nightmares and rehearsing alternative, more positive outcomes, allowing individuals to gain a sense of control over their dreams and reduce the distress associated with nightmares.
– Exposure Therapy: Exposure therapy gradually exposes individuals to trauma-related triggers in a safe and controlled environment, helping them build resilience and reduce anxiety and fear responses associated with the trauma.
It’s important to remember that treatment options may vary based on individual needs and preferences. Seeking guidance from a mental health professional can help determine the most suitable approach for addressing trauma-related nightmares. Developing a comprehensive treatment plan can improve overall well-being and increase the likelihood of experiencing peaceful and restful nights.
1. Self-Care Techniques for Nightmares
1. Self-Care Techniques for Nightmares:
Dealing with nightmares can be a distressing experience, but there are various self-care techniques that can help individuals manage their nightmares and improve their overall sleep quality. These strategies can provide a sense of control and empowerment over the nighttime terrors. Here are some self-care techniques to consider:
a) Establish a Relaxing Bedtime Routine: Creating a calming bedtime routine can signal to your body and mind that it’s time to wind down and prepare for sleep. This can include activities like taking a warm bath, practicing relaxation exercises such as deep breathing or meditation, or engaging in light reading.
b) Maintain a Consistent Sleep Schedule: Keeping a regular sleep schedule can help regulate your body’s internal clock and promote more restful sleep. Try to go to bed and wake up at the same time every day, even on weekends. This consistency can reduce the likelihood of sleep disruptions, including nightmares.
c) Create a Comfortable Sleep Environment: Make your bedroom a sanctuary for sleep by ensuring it is dark, quiet, and at a comfortable temperature. Consider using blackout curtains, earplugs, or a white noise machine to create a soothing ambiance that promotes deep sleep.
d) Practice Stress Reduction Techniques: Stress and anxiety can contribute to the occurrence of nightmares. Engaging in stress-reducing activities such as yoga, mindfulness, or journaling can help alleviate anxiety before bedtime. Experiment with different techniques to find what works best for you.
e) Limit Stimulants and Alcohol: Consuming stimulants like caffeine and nicotine, as well as alcohol, close to bedtime can disrupt sleep patterns and increase the chances of experiencing nightmares. It’s best to avoid these substances in the hours leading up to sleep.
f) Create a Safe Sleep Space: If certain objects or reminders trigger traumatic memories or nightmares, consider removing them from your sleep environment. Surround yourself with comforting objects or images that promote feelings of safety and security.
g) Seek Support: Sharing your experiences with a trusted friend, family member, or therapist can provide valuable support and validation. They can also offer insights and coping strategies based on their own experiences or professional expertise.
Remember, self-care techniques for nightmares may require trial and error to find what works best for you. It’s important to be patient and kind to yourself as you navigate through this process. If self-care techniques alone do not effectively manage your nightmares, it may be beneficial to explore therapy options or consult with a healthcare professional for further assistance.
2. Therapy and Trauma Healing
Therapy plays a crucial role in helping individuals heal from trauma and manage the impact of nightmares. There are various therapeutic approaches that have proven effective in trauma healing and addressing trauma-related nightmares.
One important therapeutic modality is cognitive-behavioral therapy (CBT), which focuses on identifying and modifying negative thought patterns and behaviors. CBT has been adapted specifically for nightmares, known as cognitive-behavioral therapy for nightmares (CBT-N). CBT-N aims to reduce the frequency and intensity of nightmares by addressing the underlying causes and triggers. It helps individuals develop coping skills and techniques to manage the distress associated with nightmares. Additionally, CBT-N can help individuals reframe their thoughts and beliefs related to the trauma, promoting healing and reducing the emotional impact of the traumatic event. Improving sleep hygiene and implementing relaxation techniques are often included in CBT-N to promote better sleep quality.
Eye Movement Desensitization and Reprocessing (EMDR) is another therapeutic approach that has shown efficacy in trauma healing. EMDR involves bilateral stimulation, typically through eye movements, while focusing on traumatic memories. This process aims to reprocess the traumatic memories and alleviate associated distress and symptoms. While EMDR is primarily used to treat PTSD, it can also be beneficial for individuals who experience trauma-related nightmares.
Other therapeutic modalities, such as exposure therapy and narrative therapy, can also be effective in trauma healing. Exposure therapy encourages individuals to gradually confront and process their traumatic memories and experiences in a safe and controlled environment. This process can help reduce the emotional reaction associated with the trauma and alleviate the frequency and intensity of nightmares. Narrative therapy, on the other hand, allows individuals to construct a coherent and meaningful narrative of their traumatic experiences, promoting healing and a sense of empowerment.
It is important to note that therapy should be tailored to individual needs and preferences. Collaborating with a trained therapist who specializes in trauma can help individuals navigate the healing process and address the impact of nightmares on their mental well-being. Therapists can provide a safe and supportive space for individuals to process their trauma, explore coping mechanisms, and develop strategies for managing nightmares. Combining therapy with self-care techniques and a comprehensive treatment plan can greatly enhance the healing process and improve overall quality of life for individuals recovering from trauma.
Conclusion
In conclusion, the connection between nightmares and trauma is a profound and intricate one. Nightmares often serve as a manifestation of the emotional and psychological impact of traumatic experiences. These intense and distressing dreams can reenact the traumatic event or incorporate elements of it, evoking fear, anxiety, and distress upon waking. Recurrent traumatic nightmares can disrupt sleep and contribute to sleep disturbances and fatigue. The neuroscientific aspect of this connection involves the amygdala, which plays a role in heightened emotional reactions and vulnerability to nightmares. The themes that emerge in trauma-related nightmares reflect the emotional impact of the trauma and unresolved psychological conflicts. Coping strategies such as maintaining a consistent sleep schedule and engaging in self-care techniques can help manage nightmares. Therapy, such as cognitive-behavioral therapy, can also be effective in addressing traumatic experiences and their impact on sleep. By understanding the connection between nightmares and trauma, we can strive for healing and seek the tools and techniques that will enable us to find restful sleep and emotional well-being. So, if you find yourself trapped in the labyrinth of nightmares, remember that there is hope for healing and a brighter tomorrow.
Frequently Asked Questions
1. Can nightmares be a sign of trauma?
Yes, nightmares can be a sign of trauma. Traumatic experiences can leave a lasting impact on an individual’s mental well-being, and nightmares often serve as a manifestation of the psychological and emotional repercussions of these events.
2. Are there different types of nightmares?
Yes, there are different types of nightmares. They can range from realistic portrayals of the traumatic event to more abstract and symbolic dreams that capture the emotional essence of the experience.
3. How do trauma-related nightmares affect mental health?
Trauma-related nightmares can have a profound impact on mental health. They can cause heightened emotional reactions, leading to feelings of fear, anxiety, and distress upon waking. Recurrent nightmares can also disrupt sleep, leading to daytime fatigue and impaired functioning.
4. Can nightmares trigger traumatic memories?
Yes, nightmares can act as triggers, evoking intense emotions and memories associated with the traumatic event. They may bring back vivid imagery, emotions, and sensations related to the trauma, contributing to the re-experiencing of the event.
5. How are recurrent traumatic nightmares different from regular nightmares?
Recurrent traumatic nightmares are characterized by the repeated occurrence of specific nightmares related to the trauma. They are often more vivid, intense, and emotionally distressing compared to regular nightmares.
6. Can nightmares be a symptom of post-traumatic stress disorder (PTSD)?
Yes, nightmares can be a symptom of PTSD. Nightmares are a common feature of PTSD and are one of the criteria used to diagnose the disorder.
7. What role does the amygdala play in the nightmare-trauma connection?
The amygdala, a brain structure involved in emotional processing, plays a significant role in the nightmare-trauma connection. Trauma can activate the amygdala, leading to heightened emotional responses and increased vulnerability to nightmares.
8. How do sleep disruptions contribute to trauma-related nightmares?
Sleep disruptions, including nightmares, can impair the brain’s ability to process and consolidate memories. This may contribute to the persistence of traumatic memories and the occurrence of trauma-related nightmares.
9. What are common themes in trauma-related nightmares?
Common themes in trauma-related nightmares often include re-experiencing the traumatic event, feelings of helplessness and vulnerability, as well as guilt, shame, and self-blame. These themes can reflect the emotional impact of the trauma and unresolved psychological conflicts.
10. What are some coping strategies and treatment options for trauma-related nightmares?
Coping strategies for trauma-related nightmares include maintaining a consistent sleep schedule, creating a relaxing bedtime routine, and engaging in stress-reducing activities. Therapy, such as cognitive-behavioral therapy for nightmares (CBT-N), can also be effective in addressing traumatic experiences and their impact on sleep.