Nightmares can be both terrifying and puzzling experiences that can leave us feeling shaken and disturbed. Understanding the neuroscience behind nightmares and how they relate to trauma is crucial in order to better comprehend and address these distressing occurrences. By delving into the intricate workings of the brain, specifically the role of the amygdala, the influence of stress hormones, and the process of memory consolidation and rehearsal, we can gain valuable insights into the root causes of nightmares. Additionally, exploring the connection between nightmares and trauma, including their impact on emotional well-being and their presence in post-traumatic stress disorder, provides a deeper understanding of their significance. Finally, we will examine coping mechanisms such as seeking professional help, therapeutic techniques, and self-care strategies to assist individuals in managing nightmares and the effects of trauma.
The Basics: What Are Nightmares
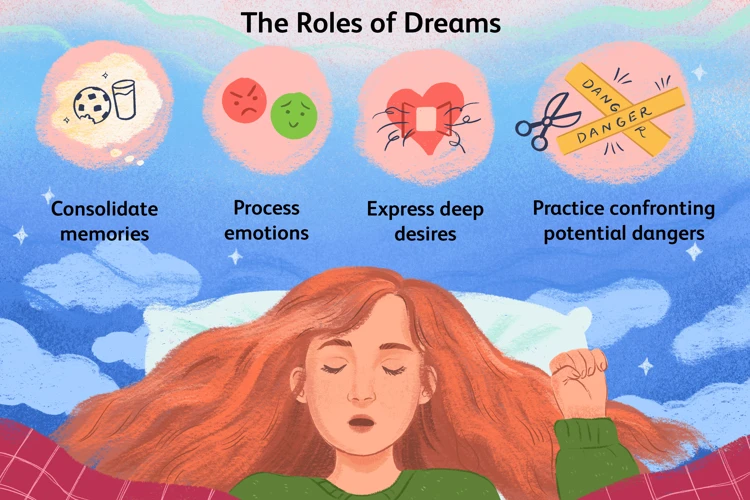
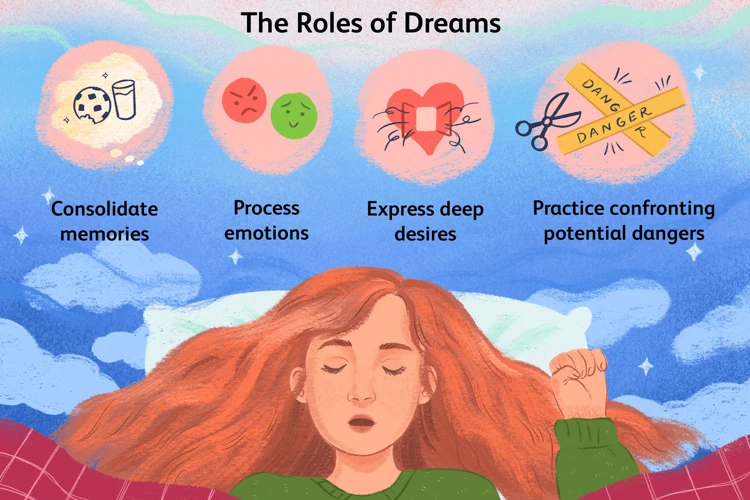
Nightmares are vivid and distressing dreams that occur during the rapid eye movement (REM) stage of sleep. They are often characterized by intense feelings of fear, anxiety, and terror, and can cause individuals to wake up feeling unsettled and emotionally overwhelmed. Nightmares can vary in content and theme, ranging from being chased or attacked, experiencing a traumatic event, or feeling trapped in a dangerous situation. These dreams can be so vivid and realistic that they evoke a strong physiological response, such as an increased heart rate and sweating. While nightmares are a common occurrence for many people, they can become more frequent and intense in individuals who have experienced trauma or are dealing with post-traumatic stress disorder (PTSD). It is important to note that nightmares and bad dreams are not the same thing. Bad dreams may be disturbing but do not usually cause intense fear or result in the same physical response as nightmares. Nightmares often disrupt sleep, causing individuals to wake up feeling tired and anxious, affecting their overall well-being and quality of life. Seeking professional help and exploring therapeutic techniques such as dream analysis can be beneficial in understanding and addressing the underlying causes of nightmares, particularly in the context of trauma and PTSD. Trauma nightmares can be analyzed and interpreted to gain insights into the unresolved emotions and experiences that may be impacting an individual’s mental health and daily life.
The Neuroscience of Nightmares
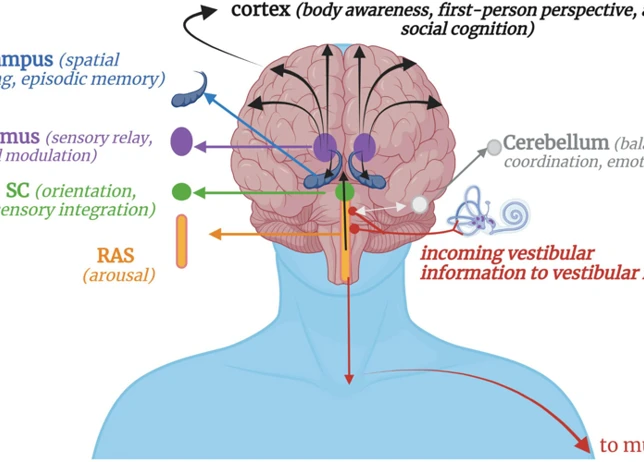
The neuroscience of nightmares uncovers the intricate workings of the brain that contribute to the creation and experience of these intense dreams. One key player in the formation of nightmares is the amygdala, a small almond-shaped structure in the brain that is responsible for processing emotions and fear. During REM sleep, the amygdala becomes hyperactive, leading to the generation of vivid and often frightening dream content. The influence of stress hormones, particularly cortisol, also plays a significant role in the neuroscience of nightmares. In times of stress or trauma, the release of cortisol can disrupt the normal sleep cycle and trigger the occurrence of nightmares. The process of memory consolidation and rehearsal, particularly in relation to emotional experiences, can contribute to the creation of nightmares. During sleep, the brain consolidates memories, including those associated with stressful or traumatic events, which can then be replayed in the form of nightmares. Understanding the neuroscience behind nightmares provides valuable insight into the mechanisms that contribute to their occurrence, and may help inform therapeutic approaches such as trauma dream analysis or exploring the connection between nightmares and PTSD.
1. The Role of the Amygdala
The amygdala, a small almond-shaped structure in the brain, plays a crucial role in the occurrence of nightmares. As an integral part of the limbic system, the amygdala is primarily responsible for processing emotions and detecting potential threats in the environment. When we experience fear or perceive a threatening situation, the amygdala activates and triggers a cascade of responses throughout the body.
During REM sleep, the amygdala continues to be active, although its level of activation may vary. Research suggests that increased amygdala activity during REM sleep is associated with the occurrence of nightmares. This heightened activity can intensify negative emotions and contribute to the creation of frightening dream scenarios. In individuals with post-traumatic stress disorder (PTSD), the amygdala may be hyperactive even during non-REM sleep, leading to persistent distressing dreams.
The amygdala’s connection with other brain regions, particularly the prefrontal cortex, further influences the content and emotional intensity of nightmares. The prefrontal cortex helps regulate emotions and cognitive processes, providing a sense of control and rational thinking. However, during REM sleep, the activity of the prefrontal cortex decreases, resulting in reduced cognitive control over emotions. This lack of inhibition can contribute to the vividness and emotional intensity of nightmares.
It is worth noting that while the amygdala’s role in nightmares is well-established, it is not the sole determinant. Other brain regions and neurotransmitters, such as the hippocampus and the effects of stress hormones, also play significant roles in shaping and modulating the content and emotional aspects of nightmares. Understanding the complex interplay between these neural mechanisms can provide valuable insights into the neuroscience behind nightmares and inform potential therapeutic approaches.
2. The Influence of Stress Hormones
The Influence of Stress Hormones: One key factor in understanding the neuroscience of nightmares is the influence of stress hormones. When we experience fear or a traumatic event, our body releases stress hormones such as cortisol and adrenaline as part of the natural “flight or fight” response. These hormones activate the amygdala, a region in the brain responsible for processing emotions and detecting threats. In the context of nightmares, the release of stress hormones can intensify emotional and physiological reactions during sleep. Research has shown that elevated levels of cortisol, in particular, can influence the content and intensity of dreams, often contributing to the creation of nightmare scenarios. Additionally, stress hormones can disrupt sleep cycles, leading to an increased likelihood of experiencing nightmares throughout the night. It is important to note that this hormonal influence is not limited to individuals who have experienced trauma, as everyday stressors can also trigger the release of stress hormones and potentially lead to nightmares. Managing stress levels and implementing stress-reduction techniques, such as mindfulness or relaxation exercises, may help mitigate the impact of stress hormones on nightmare frequency and intensity.
3. Memory Consolidation and Rehearsal
Memory consolidation and rehearsal play a crucial role in understanding the neuroscience behind nightmares. During sleep, particularly during the REM stage, the brain undergoes a process of consolidating and rehearsing memories from the day. This process involves the strengthening of neural connections related to recent experiences and events. Research suggests that nightmares may be a result of the brain attempting to process and make sense of emotional or traumatic memories. When an individual experiences a traumatic event, the brain may struggle to integrate these memories properly, leading to fragmented and distressing dreams during sleep. During nightmares, the emotional aspects of these memories are often intensified, triggering strong emotional responses and fear. This heightened emotional experience can be understood as the brain’s attempt to rehearse and understand the emotional significance of the traumatic event. By repeatedly reliving and processing these memories during nightmares, the brain may be working towards better incorporating them into long-term memory storage. It’s important to note that while nightmares can be distressing, this process of memory consolidation and rehearsal is a natural response of the brain and can be seen as a potential pathway to healing and recovery. However, when nightmares become recurring and excessively distressing, they can significantly impact an individual’s well-being and may require professional intervention and support to address and manage effectively.
Nightmares and Trauma
Trauma and nightmares often share a close relationship, with nightmares frequently being experienced as a result of traumatic events. When someone undergoes a traumatic experience, such as physical or emotional abuse, a serious accident, or a natural disaster, it can leave a lasting impact on their mental and emotional well-being. Trauma-related nightmares can serve as a replay of the distressing event, constantly reminding the individual of their past trauma and triggering intense emotional responses. These nightmares can be particularly challenging to cope with, as they can cause sleep disturbances, anxiety, and fear of falling asleep. The experience of trauma can disrupt the brain’s normal functioning, leading to changes in sleep patterns and contributing to the occurrence of nightmares. In some cases, nightmares can be a symptom of post-traumatic stress disorder (PTSD), a mental health condition that can develop following a traumatic event. Understanding the connection between nightmares and trauma is crucial in order to provide appropriate support and treatment to those who are struggling with the aftermath of traumatic experiences.
1. Trauma and Nightmares
Trauma and nightmares share a complex and interconnected relationship. Traumatic experiences can leave a lasting impact on the brain and can manifest in the form of vivid and distressing nightmares. When an individual experiences a traumatic event, their brain’s fear processing system, primarily the amygdala, becomes hyperactive. This heightened state of arousal can disrupt sleep patterns and contribute to the occurrence of nightmares. In fact, research has shown that individuals with a history of trauma are more likely to experience nightmares. The content of these nightmares often reflects the traumatic event itself or related themes and emotions. It is important to recognize that nightmares serve as a way for the brain to process and make sense of the traumatic experience, albeit in a distressing and sometimes fragmented manner. The emotional and physiological responses triggered by nightmares can intensify the distress and feelings of helplessness associated with trauma. Understanding the connection between trauma and nightmares is crucial in order to provide appropriate support and interventions for individuals who have experienced trauma and are suffering from the effects of their nightmares. By addressing the underlying trauma and its impact on sleep, it is possible to begin the healing process and alleviate the frequency and intensity of nightmares.
2. Impact on Emotional Well-being
Nightmares can have a significant impact on an individual’s emotional well-being. The vivid and distressing nature of nightmares can leave individuals feeling fearful, anxious, and on edge, even after they have woken up. These intense emotions can persist throughout the day, affecting a person’s mood, concentration, and overall ability to function. Constantly reliving traumatic or distressing experiences during nightmares can lead to a heightened sense of vulnerability and a reduced sense of safety in the waking world. Nightmares can also disrupt the sleep cycle, leading to sleep deprivation and fatigue, which can further exacerbate emotional distress and impact one’s mental health. Additionally, negative emotions triggered by nightmares can spill over into daily life, affecting interpersonal relationships, work performance, and overall quality of life. The fear and anxiety associated with nightmares can create a cycle of sleep anxiety, where individuals dread going to sleep out of fear of experiencing another distressing dream. This can lead to a constant state of hyperarousal and vigilance, perpetuating the emotional impact of nightmares. It is important to recognize the emotional toll that nightmares can have and to seek appropriate support and intervention to address the underlying causes and manage their impact on emotional well-being.
3. Nightmares as a Part of Post-Traumatic Stress Disorder
Nightmares play a significant role in post-traumatic stress disorder (PTSD), a condition that develops in some individuals following a traumatic event. People with PTSD often experience frequent and distressing nightmares that are directly related to the traumatic experience they went through. These nightmares can be intensely vivid, reenacting the traumatic event or embodying similar themes and emotions. One of the hallmark symptoms of PTSD is the re-experiencing of the traumatic event, and nightmares are a manifestation of this symptomatology. The nightmares can be so distressing that individuals may avoid sleep altogether, leading to sleep disturbances and insomnia. These nightmares can perpetuate the cycle of fear and anxiety, contributing to a heightened state of vigilance and hyperarousal, which are common symptoms of PTSD. It is important to address and treat nightmares as a part of PTSD, as they can significantly impact the individual’s overall well-being and hinder their ability to engage in daily activities. Treatment options such as therapy, medication, and self-care strategies can help individuals manage and reduce the frequency and intensity of nightmares, thereby improving their quality of life and psychological well-being. Understanding the role of nightmares in PTSD is crucial for both clinicians and individuals coping with this condition, as it provides insights into the complex nature of trauma-related sleep disturbances.
Coping with Nightmares and Trauma
Coping with nightmares and trauma requires a multifaceted approach to address the underlying causes and manage their impact on emotional well-being. Seeking professional help from therapists or counselors specializing in trauma and sleep disorders is an important step towards finding understanding and support. These professionals can provide guidance and techniques tailored to individual needs, such as cognitive-behavioral therapy (CBT) or Eye Movement Desensitization and Reprocessing (EMDR), which can help individuals process and heal from traumatic experiences. Additionally, therapeutic techniques such as relaxation exercises, mindfulness practices, and creative outlets like art therapy or journaling can be effective tools in reducing the frequency and intensity of nightmares. Furthermore, self-care strategies such as maintaining a consistent sleep routine, creating a calming bedtime ritual, engaging in physical exercise, and practicing stress management techniques can greatly contribute to overall well-being and alleviate the negative impact of nightmares and trauma. It is important to remember that coping methods may vary for each individual, and finding a combination of strategies that work best for them is key to managing nightmares and the effects of trauma effectively.
1. Seeking Professional Help
Seeking professional help is a crucial step in addressing nightmares and trauma-related issues. A trained therapist or counselor can provide valuable guidance and support in navigating the complex emotions and experiences associated with nightmares. Here are some reasons why seeking professional help is beneficial:
- Expertise: Mental health professionals have the knowledge and expertise to assess and diagnose the underlying causes of nightmares and trauma. They can provide an accurate evaluation of the individual’s condition and develop a personalized treatment plan.
- Therapeutic Techniques: Therapists employ a range of therapeutic techniques to help individuals cope with nightmares and trauma. These may include cognitive-behavioral therapy, exposure therapy, and eye movement desensitization and reprocessing (EMDR). These approaches aim to address negative thought patterns, process traumatic experiences, and reduce the frequency and intensity of nightmares.
- Safe and Supportive Environment: Therapy offers a safe and non-judgmental space for individuals to express their emotions and explore the root causes of their nightmares. A therapist can help individuals work through their trauma, develop healthy coping mechanisms, and establish a sense of emotional well-being.
- Medication Management: In some cases, medication may be recommended to alleviate symptoms associated with nightmares and trauma. A mental health professional can assess the need for medication, prescribe appropriate drugs, and provide ongoing monitoring and support.
Remember, seeking professional help is a proactive step towards healing and recovery. It is important to find a therapist who specializes in trauma and has experience in treating nightmares and related issues. Therapy can provide the necessary tools and support to help individuals regain control over their sleep and overall well-being.
2. Therapeutic Techniques
Therapeutic techniques are invaluable tools in helping individuals cope with nightmares and trauma. These techniques focus on addressing the underlying causes of nightmares, reducing their frequency and intensity, and promoting emotional healing. One effective therapeutic technique is Exposure Therapy, which involves gradually exposing the individual to the feared or traumatic elements of their nightmares in a controlled and safe environment. This allows them to confront their fears and build resilience over time. Another technique is Cognitive Behavioral Therapy (CBT), which aims to identify and challenge negative thought patterns associated with nightmares. Through CBT, individuals can learn to reframe their thoughts and develop healthier coping mechanisms. Eye Movement Desensitization and Reprocessing (EMDR) is another technique that has shown promise in the treatment of trauma-related nightmares. It involves guiding individuals to visually track the therapist’s hand movements while recalling distressing memories or nightmares, facilitating the processing and integration of these experiences. Mindfulness techniques, such as meditation and relaxation exercises, can also be effective in reducing anxiety and promoting better sleep quality. Additionally, art therapy, journaling, and group therapy can provide individuals with supportive outlets for expressing their emotions and processing their experiences. It is important to note that therapeutic techniques should be tailored to each individual’s specific needs and preferences in collaboration with a trained mental healthcare professional. The guidance and support of a therapist can greatly enhance the effectiveness of these techniques, promoting healing and recovery from nightmares and trauma.
3. Self-care Strategies
Self-care strategies play a crucial role in managing nightmares and the effects of trauma. These strategies can help individuals cope with the emotional and psychological distress associated with nightmares, promoting overall well-being. Here are some self-care strategies that can be beneficial:
1. Establishing a Regular Sleep Routine: Creating a consistent sleep schedule can help regulate the sleep-wake cycle and promote better quality sleep. This includes going to bed and waking up at the same time each day, creating a relaxing bedtime routine, and ensuring a comfortable sleep environment.
2. Practicing Relaxation Techniques: Engaging in relaxation techniques such as deep breathing, progressive muscle relaxation, or meditation can help reduce anxiety and promote a sense of calm before bedtime. These techniques can help individuals unwind and prepare for a restful night’s sleep.
3. Avoiding Triggers: Identifying and minimizing exposure to potential triggers can be helpful in preventing nightmares. This may involve avoiding stimulating activities or substances before bedtime, such as caffeine, nicotine, or intense media content.
4. Maintaining a Healthy Lifestyle: Adopting a balanced and healthy lifestyle can contribute to better sleep and overall well-being. This includes engaging in regular physical exercise, eating nutritious meals, and managing stress levels.
5. Creating a Safe Sleep Environment: Making the sleep environment comfortable and conducive to relaxation is important. This can involve using calming scents, adjusting the bedroom temperature, and ensuring a dark and quiet space.
6. Engaging in Relaxing Activities: Participating in activities that promote relaxation and stress reduction, such as reading, listening to calming music, or taking a warm bath, can help individuals wind down before bed and improve sleep quality.
7. Seeking Social Support: Talking to friends, family, or support groups about the experiences and emotions associated with nightmares and trauma can provide a sense of understanding and support. Connecting with others who have had similar experiences can be validating and offer valuable insights.
It is important to remember that self-care strategies may vary for each individual, and it may be helpful to explore different approaches to find what works best. These strategies can complement other forms of professional help and therapeutic techniques in managing nightmares and trauma.
Conclusion
In conclusion, understanding the neuroscience behind nightmares and trauma provides valuable insights into the intricate workings of the brain and the impact of distressing experiences. Nightmares, vivid and distressing dreams that often evoke intense fear and anxiety, can disrupt sleep and have a significant impact on emotional well-being. The amygdala plays a key role in processing emotions and fear, while stress hormones can influence the occurrence and intensity of nightmares. Memory consolidation and rehearsal during sleep also contribute to the manifestation of nightmares. When trauma is involved, nightmares can become more frequent and intense, and may be a part of post-traumatic stress disorder (PTSD). Coping with nightmares and trauma involves seeking professional help, utilizing therapeutic techniques such as dream analysis, and practicing self-care strategies. By addressing and managing nightmares, individuals can work towards healing and improving their overall well-being. It is important for those experiencing trauma-related nightmares to seek appropriate support and explore resources that can assist in their journey towards recovery and better mental health.
Frequently Asked Questions
1. What causes nightmares?
Nightmares can have various triggers, including anxiety, stress, trauma, medications, sleep disorders, and even certain foods or substances.
2. Are nightmares a sign of a mental health issue?
Nightmares on their own are not necessarily indicative of a mental health issue. However, recurring nightmares or nightmares that disrupt sleep can be associated with conditions such as post-traumatic stress disorder (PTSD) or anxiety disorders.
3. Can nightmares be prevented?
While it may not be possible to completely prevent nightmares, certain lifestyle changes can help reduce their frequency. Regular exercise, stress management techniques, maintaining a consistent sleep schedule, and avoiding stimulating activities before bed can all contribute to better sleep and potentially minimize nightmares.
4. Are nightmares more common in children?
Nightmares are common among children, particularly during their developmental years. This is because children’s imaginations and emotions are still developing, making them more prone to experiencing intense dreams.
5. How do nightmares affect sleep quality?
Nightmares can disrupt the sleep cycle, causing frequent awakenings throughout the night. This can result in fragmented and poor-quality sleep, leading to daytime sleepiness, fatigue, and difficulties in concentration.
6. Can nightmares be treated with medication?
In some cases, medication may be prescribed to alleviate nightmares associated with specific disorders such as PTSD. However, medication is typically not the first-line treatment and is often used in conjunction with therapy and other non-pharmacological interventions.
7. Can recurring nightmares be a symptom of trauma?
Yes, recurring nightmares are commonly associated with trauma. They can be a way for the brain to process and revisit distressing memories or unresolved emotions related to a traumatic event.
8. What are some self-care strategies to cope with nightmares?
Self-care strategies include establishing a relaxing bedtime routine, practicing stress reduction techniques like deep breathing or meditation, creating a comfortable sleep environment, and avoiding stimulating substances like caffeine or alcohol before bed.
9. How can therapy help with nightmares?
Therapy, such as cognitive-behavioral therapy for nightmares (CBT-N), can provide individuals with tools to manage and reduce the frequency and impact of nightmares. It focuses on identifying triggers, processing trauma, and developing coping mechanisms to promote better sleep.
10. When should I seek professional help for nightmares?
If nightmares are significantly affecting your daily life, causing distress, or are part of a larger mental health concern, it is recommended to seek professional help from a therapist or healthcare provider who specializes in sleep disorders or trauma.