Narcolepsy in children is a complex and often misunderstood sleep disorder that can have a profound impact on a child’s daily life. This neurological condition is characterized by excessive daytime sleepiness, sudden muscle weakness, hallucinations, and disrupted nighttime sleep. Recognizing the signs of narcolepsy in children is crucial for early intervention and support. In this article, we will explore the signs, diagnosis, and intervention strategies for narcolepsy in children, as well as lifestyle recommendations and the importance of emotional support for these young individuals.
What is Narcolepsy?
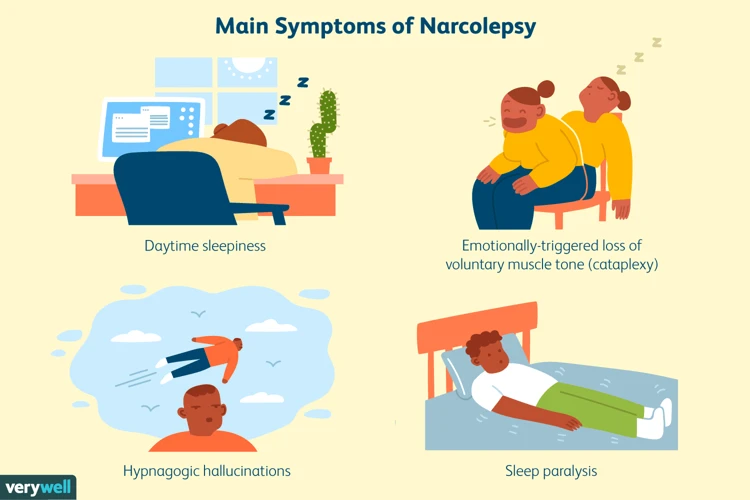
Narcolepsy is a chronic neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. It is characterized by excessive daytime sleepiness, which can cause frequent and uncontrollable episodes of excessive sleepiness during the day. Individuals with narcolepsy often experience sudden and overwhelming sleep attacks, where they may fall asleep unexpectedly, even in the middle of an activity. These sleep attacks can be disruptive and potentially dangerous, especially if they occur while driving or operating machinery. Other common symptoms of narcolepsy include sudden muscle weakness or loss of muscle control, known as cataplexy, as well as hallucinations and sleep paralysis during the transition between sleep and wakefulness. The exact cause of narcolepsy is still unknown, but research suggests that it may involve a combination of genetic and environmental factors. It is important to note that narcolepsy is a lifelong condition that cannot be cured but can be managed with the help of healthcare professionals. There are several treatment options available, including medication and behavioral strategies, which will be discussed in more detail later in this article. For those interested in learning more about the science behind narcolepsy, or reading about famous narcolepsy success stories, or demystifying cataplexy in narcolepsy, follow the provided links for further information.
Signs of Narcolepsy in Children
Narcolepsy in children can present with a variety of signs and symptoms that may differ from those seen in adults. It is important for parents and caregivers to be aware of these signs in order to seek appropriate medical attention and support.
One of the hallmark symptoms of narcolepsy in children is excessive daytime sleepiness (EDS). Children with narcolepsy may struggle to stay awake during the day, often feeling excessively tired and fatigued. They may have difficulty concentrating, lack energy, and may even fall asleep during activities such as school, playing, or socializing.
Another key sign of narcolepsy in children is sudden muscle weakness or loss of muscle control, also known as cataplexy. This symptom is often triggered by strong emotions such as laughter, excitement, or anger. During a cataplectic episode, a child’s muscles may become limp or weak, causing them to slump, drop things, or have trouble speaking. It is important to note that not all children with narcolepsy experience cataplexy.
Children with narcolepsy may also experience hallucinations and sleep paralysis. Hallucinations can occur during the transition between wakefulness and sleep and may involve vivid and often frightening images or sensations. Sleep paralysis, on the other hand, is a temporary inability to move or speak while falling asleep or waking up, usually lasting for a few seconds to a couple of minutes. Both hallucinations and sleep paralysis can be distressing for children and may contribute to anxiety or fear surrounding sleep.
In addition to the daytime symptoms, narcolepsy in children can also disrupt nighttime sleep. Children may experience frequent nighttime awakenings, nightmares, or restless sleep. These disruptions can further contribute to daytime sleepiness and impact overall well-being.
If you’d like to read inspiring stories of individuals who have successfully managed narcolepsy, check out our famous narcolepsy success stories. For a deeper understanding of the science behind narcolepsy, consider exploring our comprehensive article on the science behind narcolepsy. To learn more about cataplexy, an associated symptom of narcolepsy, you may find our article on demystifying cataplexy in narcolepsy helpful.
Excessive Daytime Sleepiness
Excessive daytime sleepiness is one of the primary symptoms of narcolepsy in children. It refers to an overwhelming and persistent feeling of sleepiness that goes beyond typical tiredness. Children with narcolepsy may struggle to stay awake during the day, even when engaging in activities they typically find enjoyable. This excessive sleepiness can affect their ability to concentrate, learn, and participate in daily activities. It may also lead to frequent napping, which can disrupt their regular sleep patterns. Parents and caregivers may notice that their child often appears drowsy or fatigued, regardless of the amount of sleep they have had. Addressing excessive daytime sleepiness is crucial in managing narcolepsy and improving the child’s quality of life.
Sudden Muscle Weakness
Sudden muscle weakness, also known as cataplexy, is a common symptom of narcolepsy in children. Cataplexy is characterized by a sudden loss of muscle tone, leading to weakness or paralysis of voluntary muscles. It can be triggered by strong emotions such as laughter, excitement, or anger. During an episode of cataplexy, a child may experience weakness in their facial muscles, resulting in drooping eyelids, difficulty speaking, or even complete collapse. In some cases, cataplexy can be mild and affect only certain muscle groups, while in others, it can cause a complete loss of muscle control, causing the child to fall to the ground. These episodes of sudden muscle weakness can last for a few seconds to a couple of minutes before the child regains normal muscle function. It’s important for parents and caregivers to be aware of this symptom and take appropriate precautions to ensure the child’s safety during episodes of cataplexy.
Hallucinations and Sleep Paralysis
Hallucinations and sleep paralysis are two distinct but related symptoms commonly experienced by individuals with narcolepsy. Hallucinations refer to vivid and often scary sensory experiences that occur during the transition between wakefulness and sleep. These hallucinations can involve seeing, hearing, or feeling things that aren’t actually there. They can vary in intensity and may be accompanied by a sense of fear or confusion. Sleep paralysis, on the other hand, is the temporary inability to move or speak while falling asleep or waking up. It can last for a few seconds to a few minutes and can be quite distressing. During episodes of sleep paralysis, individuals may also experience hallucinations, further adding to the sense of terror. Sleep paralysis occurs due to the brain’s failure to transition smoothly between sleep stages, causing a temporary loss of muscle control. These experiences can be confusing and frightening, especially for children who may not understand what is happening to them. It is important for parents and caregivers to provide support and reassurance to help children cope with these symptoms.
Disrupted Nighttime Sleep
Disrupted nighttime sleep is another common sign of narcolepsy in children. While excessive daytime sleepiness is a hallmark symptom, it is often accompanied by disturbances in nighttime sleep patterns. Children with narcolepsy may experience frequent nighttime awakenings, difficulty falling asleep, or an overall poor quality of sleep. These disruptions can further contribute to daytime sleepiness and exacerbate the symptoms of narcolepsy. Sleep fragmentation, which refers to a pattern of frequent awakenings throughout the night, is also common in children with narcolepsy. These awakenings can be brief and may go unnoticed, but they can disrupt the normal sleep cycle and prevent the child from getting the restorative sleep they need. Additionally, children with narcolepsy may experience vivid dreams or nightmares that can further disrupt their sleep and contribute to daytime fatigue. It is important for parents and caregivers to recognize these sleep disturbances and discuss them with a healthcare professional to ensure proper diagnosis and intervention for children with narcolepsy.
Diagnosing Narcolepsy in Children

Diagnosing narcolepsy in children involves a thorough evaluation of their medical history, physical examination, and sleep studies. During the initial assessment, the healthcare provider will collect information about the child’s sleep patterns, symptoms, and any family history of sleep disorders. It is essential to rule out other medical conditions that may mimic the symptoms of narcolepsy. The physical examination may involve a neurologic assessment to identify any potential underlying neurological issues.
Sleep studies, such as polysomnography and multiple sleep latency tests (MSLT), play a critical role in the diagnosis of narcolepsy. Polysomnography records various physiological measurements during sleep, including brain waves, eye movements, and muscle activity. It helps to assess the quality of nighttime sleep and detect any disruptions. MSLT is typically conducted during the daytime and measures the child’s tendency to fall asleep and the time it takes to enter REM sleep during multiple nap opportunities. Children with narcolepsy often exhibit a shorter sleep onset latency and a tendency to enter REM sleep quickly during these tests.
A diagnosis of narcolepsy is made when the child exhibits excessive daytime sleepiness and has at least two or more REM sleep-related abnormalities in the MSLT. It is important to consult with a healthcare professional who specializes in sleep disorders to ensure an accurate diagnosis and appropriate treatment plan. The diagnostic process may require multiple evaluations over a period of time to gather sufficient data for an accurate diagnosis.
Medical History and Physical Examination
When diagnosing narcolepsy in children, medical professionals typically begin with a thorough medical history and physical examination. The medical history involves collecting information about the child’s sleep patterns, including the duration and quality of sleep, as well as any symptoms or behaviors that are indicative of narcolepsy. The doctor may inquire about daytime sleepiness, episodes of sudden muscle weakness or cataplexy, hallucinations, and sleep paralysis. It is important for parents or caregivers to provide detailed and accurate information to assist in the diagnosis. Additionally, a physical examination will be conducted to rule out any other underlying medical conditions that may be causing the symptoms. The doctor may check for signs of other sleep disorders or neurological conditions that could mimic narcolepsy symptoms. This comprehensive assessment helps healthcare professionals determine if further testing, such as sleep studies, is necessary for an accurate diagnosis.
Sleep Studies
Sleep studies, also known as polysomnography, play a crucial role in the diagnosis of narcolepsy in children. These studies are conducted in a specialized sleep center or laboratory and involve monitoring various physiological factors during sleep. The information gathered from sleep studies provides valuable insights into the child’s sleep patterns and helps healthcare professionals make an accurate diagnosis. During a sleep study, several electrodes are placed on the child’s scalp, face, and body to record brain waves, eye movements, muscle activity, heart rate, and breathing patterns. Additionally, sensors are used to monitor oxygen levels and airflow. The child is then allowed to sleep while the data is collected throughout the night. This data is later analyzed by sleep specialists to determine if there are any abnormalities in the child’s sleep architecture, such as disruptions in REM sleep or frequent awakenings. Sleep studies are a safe and non-invasive procedure that helps differentiate narcolepsy from other sleep disorders and provides valuable information for treatment planning. It is important for parents and caregivers to follow the instructions provided by the sleep center to ensure accurate results.
Intervention and Support
Intervention and support are crucial for children with narcolepsy to manage their symptoms and improve their quality of life. Here are some key strategies that can be employed:
1. Medication: Medications can help regulate sleep patterns and reduce excessive daytime sleepiness in children with narcolepsy. Stimulants, such as modafinil and amphetamines, are commonly prescribed to promote wakefulness during the day. Sodium oxybate, a central nervous system depressant, can also be used to improve nighttime sleep and reduce cataplexy.
2. Behavioral Strategies: Implementing behavioral strategies can help children cope with narcolepsy symptoms. This may include maintaining a consistent sleep schedule, practicing good sleep hygiene, and taking scheduled naps to manage daytime sleepiness. It can also be helpful to educate family members, teachers, and caregivers about narcolepsy to ensure a supportive environment.
3. Educational Support: Children with narcolepsy may require additional support in an educational setting. This can involve accommodations such as allowing frequent breaks, providing a quiet space for naps if needed, and allowing flexibility in deadlines and assignments. It is also important for teachers and school staff to be educated about narcolepsy to better understand and support the child’s needs.
4. Lifestyle Modifications: Making certain lifestyle modifications can also contribute to managing narcolepsy symptoms. Regular exercise, a healthy diet, and avoiding caffeine and alcohol close to bedtime can promote better sleep. Creating a relaxing bedtime routine and ensuring a comfortable sleep environment can also help improve nighttime sleep quality.
It is worth noting that every child’s needs may vary, and individualized treatment plans should be developed in collaboration with healthcare professionals. Intervention and support can significantly help children with narcolepsy to lead fulfilling lives by managing their symptoms effectively.
Medication
Medication plays a crucial role in managing narcolepsy in children. There are several types of medications that are commonly prescribed to help alleviate the symptoms and improve the quality of life for children with narcolepsy. One common class of medications used is stimulants, which help to promote wakefulness and reduce excessive daytime sleepiness. These medications work by stimulating the central nervous system and increasing levels of certain neurotransmitters in the brain. Some commonly prescribed stimulant medications for narcolepsy include methylphenidate and amphetamines. Another class of medications used for narcolepsy is selective serotonin reuptake inhibitors (SSRIs), which are primarily used to manage cataplexy, hallucinations, and sleep paralysis. These medications work by increasing the levels of serotonin in the brain, which can help to regulate sleep and improve overall symptoms. Additionally, sodium oxybate, also known as gamma-hydroxybutyrate (GHB), is a medication that is sometimes prescribed to manage both excessive daytime sleepiness and cataplexy. It is taken at night and helps to improve the quality of nighttime sleep, reduce the severity of cataplexy episodes, and promote daytime wakefulness. It is important to note that medication should always be prescribed and closely monitored by a healthcare professional specialized in sleep disorders, as each child’s treatment plan may vary depending on their specific symptoms and needs.
Behavioral Strategies
Behavioral strategies play a crucial role in managing narcolepsy in children. These strategies focus on creating a supportive and structured environment that promotes healthy sleep habits. Some effective behavioral strategies for children with narcolepsy include:
1. Maintaining a Consistent Sleep Schedule: Establishing a regular sleep schedule is important to regulate the child’s sleep-wake cycle. Encourage a consistent bedtime and wake-up time, even on weekends, to promote better sleep quality.
2. Napping Strategically: Encourage planned, scheduled naps throughout the day to help combat excessive daytime sleepiness. Short power naps of around 20 minutes can provide a temporary boost in alertness without interfering with nighttime sleep.
3. Creating a Sleep-Friendly Environment: Ensure the child’s bedroom is conducive to sleep by keeping it cool, dark, and quiet. Minimize screen time before bed and establish a relaxing bedtime routine to help signal the body that it’s time to sleep.
4. Regular Exercise: Engaging in regular physical activity can improve overall sleep quality and help manage symptoms of narcolepsy. Encourage the child to participate in activities they enjoy, such as swimming, biking, or playing sports.
5. Nutrition and Hydration: A healthy diet and proper hydration can impact sleep quality. Encourage the child to consume a balanced diet, limiting caffeine and sugary foods close to bedtime.
6. Monitoring Medication: If the child is prescribed medication for narcolepsy, ensure that they take it as prescribed and monitor its effectiveness. Work closely with the healthcare provider to make any necessary adjustments.
By implementing these behavioral strategies, parents and caregivers can help children with narcolepsy manage their symptoms and improve their quality of life. It is important to remember that each child is unique, and some strategies may work better for certain individuals than others. Working closely with healthcare professionals and sleep specialists can provide tailored guidance and support for effective management of narcolepsy.
Educational Support
When it comes to educational support for children with narcolepsy, it is important to create an environment that accommodates their unique needs and challenges. Here are some strategies that can be implemented to provide effective educational support:
1. Individualized Education Plan (IEP): An IEP is a legally binding document that outlines specific accommodations and modifications for students with special needs. It is important for parents and educators to work together to develop an IEP that addresses the individual needs of the child with narcolepsy. This may include adjustments to the classroom environment, such as allowing the student to take short naps during the day, providing extra time for assignments or tests, and making sure the classroom is well-lit and not too warm, as these conditions can exacerbate sleepiness.
2. Flexible Scheduling: Children with narcolepsy may benefit from a flexible schedule that allows for breaks or rest periods throughout the day. This can help them manage their energy levels and prevent excessive daytime sleepiness from interfering with their academic performance. Additionally, allowing the child to have access to accommodations such as a quiet space for rest or a designated area for taking medication can greatly contribute to their overall well-being and academic success.
3. Teacher Education and Awareness: It is crucial for teachers and school staff to be educated about narcolepsy and its impact on a student’s daily life and academic performance. By providing training and resources to educators, they can better understand the condition and implement strategies that support the child in the classroom. This may involve implementing classroom strategies to minimize distractions, being flexible with deadlines, and promoting awareness and understanding among classmates to create a supportive and inclusive environment.
4. Peer Support: In addition to educational support from teachers and school staff, fostering peer support can also be beneficial for children with narcolepsy. This can be done through organized support groups within the school or creating opportunities for the child to connect with peers who may have similar experiences. Peer support can help reduce feelings of isolation and provide a sense of belonging, which is important for the overall well-being of the child.
By implementing these educational support strategies, children with narcolepsy can have equal access to education and thrive academically while managing their symptoms effectively. It is essential for parents, educators, and healthcare professionals to work collaboratively to ensure that the child’s educational needs are met in a supportive and understanding environment.
Lifestyle Recommendations for Narcolepsy in Children

Children with narcolepsy can benefit from incorporating certain lifestyle recommendations into their daily routines to better manage their symptoms and improve their overall well-being. Here are some lifestyle recommendations for children with narcolepsy:
1. Maintain a Consistent Sleep Schedule: Establishing a regular sleep schedule can help regulate the sleep-wake cycle and promote better nighttime sleep. Encourage your child to go to bed and wake up at the same time every day, including weekends and holidays.
2. Create a Sleep-Friendly Environment: Designing a conducive sleep environment is essential for promoting quality sleep. Make sure your child’s bedroom is dark, quiet, and comfortable. Consider using blackout curtains, earplugs, or white noise machines to minimize disruptions during sleep.
3. Practice Good Sleep Hygiene: Teach your child healthy sleep habits, such as winding down before bed, avoiding stimulating activities close to bedtime, and limiting screen time in the evening. Encourage relaxing activities like reading or taking a warm bath before sleep.
4. Support Regular Nap Schedule: Scheduled naps during the day may help manage excessive daytime sleepiness. Work with your child’s school or daycare to accommodate scheduled nap times when needed.
5. Encourage Physical Activity: Regular exercise can improve sleep quality and daytime alertness. Encourage your child to engage in age-appropriate physical activities, such as playing sports, swimming, or bike riding.
6. Healthy Diet: Promote a balanced diet for your child, including plenty of fruits, vegetables, whole grains, and lean proteins. Avoid heavy meals close to bedtime and limit caffeine intake, as it can interfere with sleep.
7. Manage Stress: Help your child develop stress-management techniques, such as deep breathing exercises, mindfulness, or engaging in hobbies they enjoy. Stress can worsen narcolepsy symptoms, so it’s important to support your child’s emotional well-being.
It’s important to consult with a healthcare professional to discuss these lifestyle recommendations and how they can be tailored to your child’s specific needs. Implementing these strategies, along with medical interventions and support, can help children with narcolepsy lead fulfilling lives while managing their condition.
The Importance of Emotional Support
The importance of emotional support cannot be overstated when it comes to children with narcolepsy. A diagnosis of narcolepsy can have a significant impact on a child’s emotional well-being, as they may feel isolated, misunderstood, or embarrassed by their symptoms. It is crucial for parents, caregivers, and healthcare professionals to provide a supportive and understanding environment for these children. Here are some key reasons why emotional support is essential for children with narcolepsy:
1. Reducing stigma: Narcolepsy is often misunderstood, and children with this condition may face stigma and misconceptions from their peers or even adults. Emotional support can help in challenging and dispelling these misconceptions, allowing the child to feel more accepted and understood.
2. Building self-esteem: Children with narcolepsy may struggle with low self-esteem due to the challenges they face with their sleep disorder. Providing emotional support can help boost their self-confidence and reassure them that their condition does not define their worth or abilities.
3. Addressing anxiety and depression: Living with narcolepsy can lead to heightened levels of anxiety and depression, especially if the child is dealing with difficulties at school or social situations due to their symptoms. Emotional support can help the child cope with these emotional challenges and provide them with strategies to manage their anxiety or seek professional help if needed.
4. Encouraging open communication: By fostering an environment of emotional support, children with narcolepsy are more likely to feel comfortable discussing their symptoms, concerns, and any challenges they may be facing. This open communication can lead to better overall management of the condition and an improved quality of life.
5. Promoting resilience: Emotional support plays a vital role in helping children with narcolepsy build resilience and develop coping strategies to navigate the challenges they may encounter. By offering a safe space to express their emotions and providing guidance, caregivers and healthcare professionals can empower these children to overcome obstacles and thrive.
Emotional support is crucial for children with narcolepsy. It can help reduce stigma, build self-esteem, address anxiety and depression, encourage open communication, and promote resilience. Creating a supportive and understanding environment for these children is essential for their emotional well-being and overall quality of life.
Conclusion
In conclusion, narcolepsy is a complex sleep disorder that can significantly impact the lives of children. It is crucial to recognize the signs and symptoms of narcolepsy in order to provide early intervention and support. Excessive daytime sleepiness, sudden muscle weakness, hallucinations, and disrupted nighttime sleep are common indicators of narcolepsy in children. Diagnosing narcolepsy may involve medical history, physical examinations, and sleep studies. Once diagnosed, various interventions and support systems can be implemented to help manage the condition. Medication, behavioral strategies, and educational support are important components of narcolepsy management. Additionally, lifestyle recommendations, such as maintaining a consistent sleep schedule and creating a sleep-friendly environment, can greatly benefit children with narcolepsy. Emotional support is also crucial for children with narcolepsy, as it helps them cope with the challenges posed by the condition. Overall, with proper diagnosis, intervention, and support, children with narcolepsy can lead fulfilling lives and manage their symptoms effectively.
Frequently Asked Questions
1. What age does narcolepsy usually onset in children?
Narcolepsy typically begins to manifest in children between the ages of 10 and 20, although it can develop at any age.
2. Can narcolepsy in children be mistaken for laziness or lack of motivation?
Yes, the excessive daytime sleepiness and sudden episodes of sleep attacks in children with narcolepsy can sometimes be mistaken for laziness or lack of motivation, leading to potential misunderstandings and challenges in academic and social settings.
3. Is narcolepsy a rare condition in children?
No, narcolepsy is not considered a rare condition in children. It may be underdiagnosed or misdiagnosed due to its complex symptoms, but it is estimated that narcolepsy affects approximately 1 in 2,000 individuals.
4. Can narcolepsy in children affect their academic performance?
Yes, the excessive daytime sleepiness and disruptions in sleep patterns can significantly impact a child’s academic performance, as they may struggle to stay awake and alert during classes, leading to difficulties in concentration, memory, and learning.
5. Is narcolepsy hereditary?
There appears to be a genetic component to narcolepsy, as it can run in families. However, having the genetic predisposition does not guarantee that an individual will develop narcolepsy.
6. Are there any specific triggers that can worsen symptoms in children with narcolepsy?
Yes, certain triggers can exacerbate symptoms in children with narcolepsy, including stress, excitement, boredom, and changes in sleep patterns or routines.
7. Can narcolepsy in children be treated with medication?
Yes, medication can play a crucial role in managing narcolepsy in children. Stimulant medications, such as methylphenidate or amphetamines, are often prescribed to help improve wakefulness and reduce daytime sleepiness.
8. Are there any lifestyle adjustments that can benefit children with narcolepsy?
Yes, establishing a consistent sleep schedule, maintaining a healthy diet, engaging in regular exercise, and creating a conducive sleep environment can all have positive effects on managing narcolepsy symptoms in children.
9. Can narcolepsy in children improve over time?
While narcolepsy is a chronic condition, the symptoms can vary in severity and may change over time. With proper management and support, children with narcolepsy can lead fulfilling and productive lives.
10. Is emotional support important for children with narcolepsy?
Absolutely. Emotional support from family, friends, and healthcare professionals is crucial for children with narcolepsy. It can help them cope with the challenges of living with a chronic condition and improve their overall well-being.








