With the increasing prevalence of medication use, there is a growing concern about the potential impact on our sleep and dreams. Many individuals have reported experiencing disturbing nightmares after starting certain medications. This phenomenon has led researchers to explore the link between medication and nightmares, and how this connection can be managed. In this article, we will delve into the different types of medications that can potentially influence nightmares, the specific medications within those categories, and strategies for managing medication-related nightmares and improving sleep quality. Whether you are someone who has experienced medication-related nightmares or are simply curious about the topic, this article aims to provide a comprehensive understanding of the impact of medication on our dreams.
Types of Medication

Medication can have various effects on our physical and mental well-being, including our sleep patterns and dreams. Understanding the different types of medication is crucial in order to comprehend their potential impact on nightmares. There are several categories of medication that can potentially influence our dream experiences. These include antidepressants, which are commonly prescribed to manage depression and anxiety. Antipsychotics are another class of medication primarily used to treat mental disorders such as schizophrenia. Sedatives and sleep aids are substances that help induce sleep and are often used to alleviate insomnia. Lastly, beta blockers are medications primarily prescribed to manage cardiovascular conditions and regulate heart rate. Each of these medication types can potentially have an impact on our sleep and dreams, and it is important to understand how they are connected.
1. Antidepressants
Antidepressants are medications commonly prescribed to help manage depression, anxiety, and other mood disorders. While they can be effective in improving mental health, some individuals may experience an unexpected side effect of increased nightmares. The exact mechanism of how antidepressants influence dreaming is not fully understood, but it is believed that the medications may impact the neurotransmitters in the brain that regulate sleep and dreaming. Antidepressants such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are known to affect serotonin levels in the brain, which can potentially disrupt normal REM sleep patterns and contribute to more intense and vivid dreams. Interestingly, these medications can also have paradoxical effects, where they alleviate depression or anxiety but lead to an increase in nightmares. It is essential for individuals starting antidepressant therapy to be aware of this possibility and discuss any changes in dreams with their healthcare provider. If nightmares become distressing or persistent, it may be necessary to adjust the dosage or try a different medication. Additionally, incorporating non-pharmacological treatments such as cognitive-behavioral therapy (CBT) or relaxation techniques can be beneficial in managing both the underlying condition and the nightmares associated with antidepressants.
2. Antipsychotics
Antipsychotics are a class of medication primarily used to treat mental disorders such as schizophrenia and bipolar disorder. While antipsychotics are effective in managing these conditions, they can potentially have an impact on our dreams and sleep patterns. It is important to note that not all individuals who take antipsychotics will experience nightmares, as the effect varies from person to person. However, some studies suggest that certain antipsychotic medications may increase the likelihood of nightmares or vivid dreams. This could be due to the way these medications affect neurotransmitters in the brain, such as dopamine and serotonin. Antipsychotics can also cause disruptions in sleep architecture, leading to disturbances in dreaming. Additionally, the underlying mental health condition being treated with antipsychotics may itself contribute to the presence of nightmares. It is essential for individuals taking antipsychotics to communicate any changes in sleep patterns or nightmares with their healthcare provider, as adjustments to medication dosage or additional strategies may be needed to manage these effects. Research into the relationship between antipsychotics and nightmares is still ongoing, and understanding the individual response to these medications is crucial for effective treatment.
3. Sedatives and Sleep Aids
Sedatives and sleep aids are medications commonly used to promote sleep and alleviate insomnia. These medications work by suppressing the central nervous system, resulting in drowsiness and relaxation. While sedatives and sleep aids can be highly effective in helping individuals fall asleep, they may also have an impact on the content and intensity of dreams, potentially leading to nightmares. It is important to note that not all individuals who use sedatives or sleep aids will experience nightmares. However, for some individuals, these medications can disrupt the normal sleep cycle and result in vivid and unsettling dreams. Additionally, sedatives and sleep aids can alter the REM (Rapid Eye Movement) sleep phase, which is when most dreams occur. This alteration of the sleep cycle may increase the likelihood of experiencing disturbing or vivid dreams. If you are using sedatives or sleep aids and find that nightmares are becoming a recurring issue, it is essential to discuss this with your healthcare provider. They may be able to adjust your dosage or suggest alternative options. Additionally, incorporating non-pharmacological treatments, such as relaxation techniques or cognitive behavioral therapy, can be beneficial in managing nightmares. It is important to strike a balance between achieving restful sleep and minimizing the potential negative impact of sedatives and sleep aids on dream experiences. By working closely with your healthcare provider, you can find an approach that best suits your needs and helps improve your sleep quality.
4. Beta Blockers
Beta blockers are a type of medication commonly prescribed to manage cardiovascular conditions such as hypertension and angina. They work by blocking the effects of adrenaline, which helps to lower blood pressure and reduce heart rate. While beta blockers are primarily used for their cardiovascular benefits, they can also potentially affect our sleep and dreams. It has been reported that some individuals who take beta blockers may experience changes in their dream patterns, including vivid or intense dreams, nightmares, or even unusual dream content. The exact mechanism behind this phenomenon is not fully understood, but it is believed that the impact on dreams may be due to the medication’s influence on the body’s stress response system. Beta blockers may interfere with the release of stress hormones, which can influence the content and emotional tone of dreams. Additionally, beta blockers may also affect sleep architecture and disrupt normal REM (rapid eye movement) sleep patterns, which is the stage of sleep when dreaming most commonly occurs. It is important to note that not everyone who takes beta blockers will experience changes in their dreams, and the severity of these effects can vary from person to person. If you are taking beta blockers and are experiencing disturbing or unusual dream experiences, it is recommended to consult with your healthcare provider for further evaluation and guidance. Understanding the potential impact of beta blockers on our sleep and dreams is an essential step in managing any changes or disturbances that may arise.
The Link Between Medication and Nightmares
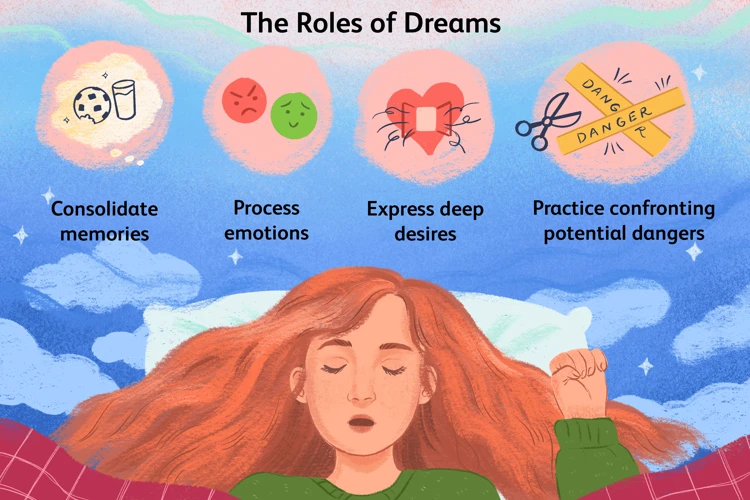
The connection between medication and nightmares has been a subject of interest for researchers and individuals alike. Different types of medication can have varying effects on our dream experiences. Antidepressants, for example, may sometimes cause vivid and intense nightmares as a side effect. This is also true for certain antipsychotics which can disrupt normal sleep patterns and lead to unsettling dreams. Similarly, some sedatives and sleep aids can influence the content and intensity of dreams. Even beta blockers, primarily used for cardiovascular conditions, have been known to affect sleep quality and potentially contribute to more frequent nightmares. Understanding the potential relationship between medication and nightmares is crucial for individuals who may be experiencing unsettling dream experiences. It is important to consult with healthcare providers to address any concerns and explore suitable alternatives if necessary. For those interested in delving further into the topic, understanding the psychology of nightmares can provide valuable insights.
1. Antidepressants and Nightmares
Antidepressant medications are commonly prescribed to individuals experiencing symptoms of depression, anxiety, and other mood disorders.(source) While these medications have shown great efficacy in managing mental health conditions, they can also potentially impact the frequency and content of nightmares. The specific impact of antidepressants on nightmares varies based on the type of medication used. Certain antidepressants, such as selective serotonin reuptake inhibitors (SSRIs) like fluoxetine and sertraline, have been associated with an increase in vivid and intense dreams, including nightmares. This may be due to the way SSRIs affect the brain’s neurotransmitters, particularly serotonin. Additionally, tricyclic antidepressants (TCAs), another class of medications, may also increase the occurrence of nightmares in some individuals. It is important to note that not everyone who takes antidepressants will experience nightmares, and the risk varies from person to person. If you are taking antidepressants and notice an increase in nightmares that significantly disrupts your sleep or causes distress, it is advisable to consult with your healthcare provider for further evaluation and possible adjustments to your medication. Understanding the potential impact of antidepressants on nightmares is crucial for individuals taking these medications and can aid in managing any related sleep disturbances.(source)
2. Antipsychotics and Nightmares
Antipsychotics are a class of medication commonly prescribed to individuals with mental health disorders such as schizophrenia and bipolar disorder. While these medications are effective in managing symptoms like hallucinations, delusions, and mood swings, they can also potentially contribute to the occurrence of nightmares. Research suggests that certain antipsychotics, such as risperidone and quetiapine, may increase the likelihood of experiencing vivid and intense dreams during sleep. The exact mechanism through which antipsychotics influence dreams is not fully understood, but it is believed to be related to alterations in neurotransmitter levels in the brain. It is important to note that not everyone who takes antipsychotic medication will experience nightmares, and the occurrence and severity of nightmares can vary from person to person. If you are taking antipsychotic medication and are experiencing distressing nightmares, it is essential to discuss your concerns with your healthcare provider. They may be able to adjust your dosage or switch you to a different medication that has a lower likelihood of impacting your dreams. Additionally, implementing non-pharmacological treatments, such as talk therapy or stress management techniques, may also help alleviate nightmares associated with antipsychotic use. Understanding the potential link between antipsychotics and nightmares can aid in effectively managing this side effect and improving overall sleep quality. For individuals who are already dealing with mental health issues, experiencing nightmares can exacerbate stress and anxiety levels, so it is crucial to seek appropriate support and treatment. If you’d like to learn more about the connection between stress, anxiety, and nightmares, check out our article here.
3. Sedatives and Sleep Aids and Nightmares
The use of sedatives and sleep aids can potentially lead to nightmares and disrupted dream patterns. Sedatives, such as benzodiazepines and barbiturates, work by suppressing the central nervous system to induce a state of relaxation and drowsiness. While these medications can be effective in promoting sleep, they may also disrupt the normal sleep cycle and lead to vivid and disturbing dreams. Additionally, some sleep aids, such as over-the-counter medications containing diphenhydramine or doxylamine, can have side effects that include nightmares. The exact mechanisms by which sedatives and sleep aids influence dreams are not fully understood, but it is believed that these medications may affect the brain regions involved in regulating REM sleep and dream generation. It is important to note that not everyone who takes sedatives or sleep aids will experience nightmares, as individual reactions may vary. However, if you are experiencing distressing dreams or nightmares after starting a sedative or sleep aid, it is advisable to consult with your healthcare provider for further evaluation and potential adjustments to your medication regimen.
4. Beta Blockers and Nightmares
Beta blockers are a class of medication primarily prescribed for cardiovascular conditions, such as high blood pressure and heart rhythm disorders. While beta blockers are not typically associated with the occurrence of nightmares, there have been some reported cases where individuals experienced disturbing dreams while taking these medications. The exact mechanism behind this connection is not fully understood, but it is believed to be related to the impact of beta blockers on sleep architecture. Beta blockers can potentially interfere with REM (rapid eye movement) sleep, which is the stage of sleep associated with vivid dreaming. By reducing the duration of REM sleep or altering the frequency of REM cycles, beta blockers may disrupt the normal dream process and potentially contribute to the occurrence of nightmares. It is important to note that not everyone who takes beta blockers will experience nightmares, and the occurrence may vary from person to person. If you are taking beta blockers and experiencing distressing dreams or nightmares, it is recommended to discuss this with your healthcare provider in order to explore potential alternatives or adjust the dosage of the medication to alleviate this side effect.
Managing Medication-Related Nightmares
Managing medication-related nightmares can be challenging, but there are strategies that can help alleviate this issue and improve sleep quality. The first step is to communicate with your healthcare provider. Discussing your concerns and experiences with medication-related nightmares can help your healthcare provider understand the impact and explore potential solutions. Adjusting the dosage or switching medication may be considered if nightmares persist and significantly affect your quality of life. Additionally, incorporating non-pharmacological treatments such as cognitive behavioral therapy or relaxation techniques can be beneficial. Keeping a sleep diary to track your medication use, sleep patterns, and nightmares can provide valuable information and help identify patterns or triggers. By actively managing medication-related nightmares, you can work towards achieving restful and rejuvenating sleep.
1. Communicate with Your Healthcare Provider
When experiencing nightmares or any sleep disturbances related to medication use, it is crucial to maintain open communication with your healthcare provider. Your healthcare provider is the most qualified person to help you navigate this situation. They can provide valuable insights, guidance, and potential solutions to alleviate medication-related nightmares. It is essential to inform them about the specific symptoms you are experiencing, including the frequency, duration, and intensity of your nightmares. They can review your medication regimen and assess whether your current medication is likely causing the nightmares. Additionally, your healthcare provider may recommend alternative medications or adjust the dosage to minimize the impact on your dreams. Keep in mind that abruptly stopping or altering medication without professional guidance can be dangerous. Engaging in open and honest conversations with your healthcare provider can ensure that they are well-informed and can provide the best course of action to manage medication-related nightmares effectively. By collaborating with your healthcare provider, you can work towards finding the most suitable solution to improve your sleep quality and reduce the distressing impact of nightmares.
2. Adjusting Dosage or Switching Medication
When experiencing nightmares as a side effect of medication, one possible solution is to adjust the dosage or switch to a different medication. Adjusting the dosage involves working closely with a healthcare provider to find the optimal balance of medication that minimizes the occurrence of nightmares. This can be done by either increasing or decreasing the dosage, depending on the individual’s response. It is important to note that dosage adjustments should only be made under the guidance of a healthcare professional to ensure safety and effectiveness. Switching medication may be another option if the nightmares persist despite dosage adjustments. In such cases, the healthcare provider may recommend a different medication within the same class or explore alternative medication options. This can be a trial-and-error process, as finding the right medication that effectively manages symptoms without causing nightmares can take time. Open communication with the healthcare provider is key to navigating this process and finding the best solution for each individual.
3. Incorporating Non-pharmacological Treatments
When it comes to managing medication-related nightmares, incorporating non-pharmacological treatments can be beneficial. These treatments focus on alternative approaches to improve sleep quality and reduce the occurrence of nightmares. Here are some effective non-pharmacological treatments that can be considered:
1. Cognitive Behavioral Therapy for Insomnia (CBT-I): This therapy aims to change negative thoughts and behaviors surrounding sleep. It helps individuals develop healthier sleep patterns and habits, reducing the likelihood of nightmares.
2. Relaxation techniques: Practices such as deep breathing exercises, progressive muscle relaxation, and guided imagery can help promote relaxation and calmness before sleep. These techniques can reduce anxiety and stress, contributing to a more peaceful sleep environment.
3. Sleep hygiene: Maintaining good sleep hygiene is essential for improving sleep quality. This involves establishing a consistent sleep schedule, creating a comfortable sleep environment, and avoiding stimulating activities or substances before bedtime.
4. Imagery Rehearsal Therapy (IRT): This therapy involves rewriting or reimagining the content of nightmares to promote more positive outcomes. By mentally rehearsing more pleasant dream scenarios, individuals can reduce the frequency and intensity of nightmares.
5. Stress reduction techniques: Engaging in stress-reducing activities like yoga, meditation, or mindfulness exercises can help alleviate anxiety and improve overall sleep quality, potentially reducing nightmares.
It’s worth noting that these non-pharmacological treatments can be used in combination with medication or as standalone approaches, depending on individual needs and preferences. Consulting with a healthcare provider can help determine the most suitable non-pharmacological treatment options for managing medication-related nightmares.
4. Keeping a Sleep Diary
Keeping a sleep diary can be an effective tool in managing medication-related nightmares. By documenting your sleep patterns, you can gain valuable insights into the frequency and intensity of your nightmares, as well as potential triggers or patterns. Start by recording the time you go to bed and wake up each day, noting any significant events or emotions before bedtime, and detailing your dream experiences upon waking up. This diary can help you identify any correlations between medication use and the occurrence of nightmares. Additionally, you can use the sleep diary to track any changes in medication dosages or adjustments, which can then be compared to variations in your sleep quality and dream content. The diary can also be a helpful resource when discussing your experiences with your healthcare provider, as it provides concrete data to inform potential changes in medication or dosage. Remember to be consistent with your sleep diary and make sure to include any relevant details that may contribute to your understanding of your nightmares. With time, this practice can help you gain better control over your sleep patterns and manage medication-related nightmares effectively.
Conclusion
In conclusion, it is clear that the use of medication can have a significant impact on our nightmares and overall sleep quality. The link between medication and nightmares is complex and varies depending on the type of medication used. Antidepressants, antipsychotics, sedatives and sleep aids, as well as beta blockers, have been found to potentially influence the occurrence and intensity of nightmares. It is essential to communicate effectively with healthcare providers about any concerns or experiences with medication-related nightmares. Adjusting dosage or switching to alternative medications may be necessary to alleviate these side effects. Furthermore, incorporating non-pharmacological treatments, such as therapy or relaxation techniques, can be beneficial. Keeping a sleep diary can also provide valuable insights into the frequency and severity of nightmares, aiding in the management process. Overall, it is important to prioritize open communication with healthcare professionals and explore various strategies to effectively manage medication-related nightmares and improve sleep quality. By taking proactive steps, individuals can find relief from disturbing dreams and achieve a better night’s rest.
Frequently Asked Questions
1. Are nightmares a common side effect of medication?
While nightmares can be a side effect of certain medications, they are not a common occurrence for everyone taking medication. The likelihood of experiencing nightmares as a side effect can depend on the specific medication and individual factors.
2. Do all antidepressants cause nightmares?
No, not all antidepressants cause nightmares. However, some individuals may experience an increase in vivid dreams or nightmares while taking certain types of antidepressants. It is important to discuss any concerns with your healthcare provider.
3. Can antipsychotics contribute to nightmares?
Although antipsychotics can have various side effects, including changes in sleep patterns, nightmares are not a commonly reported side effect. However, individual experiences may vary, and it is essential to communicate any concerning symptoms with your doctor.
4. Do sedatives and sleep aids affect dream content?
Yes, sedatives and sleep aids can influence dream content. These medications are designed to promote sleep, and they may increase the likelihood of experiencing vivid dreams or nightmares for some individuals.
5. Are beta blockers known to cause nightmares?
Nightmares are not a commonly reported side effect of beta blockers. These medications primarily target cardiovascular conditions and are not typically associated with disturbing dream experiences. If you are concerned about nightmares while taking beta blockers, consult your healthcare provider.
6. How can I manage nightmares caused by medication?
Managing nightmares caused by medication involves open communication with your healthcare provider. They can help assess whether the medication is the likely cause and guide any necessary adjustments in dosage or switching to a different medication. Incorporating non-pharmacological treatments such as therapy or relaxation techniques may also be beneficial.
7. Should I stop taking my medication if it is causing nightmares?
No, it is important not to stop taking your medication without consulting your healthcare provider. Abruptly discontinuing medication can have adverse effects on your health. Instead, discuss your concerns with your doctor, who can explore alternative options or adjust the dosage.
8. Can medication-related nightmares be a sign of a deeper issue?
While nightmares can be a side effect of medication, they can also be a sign of underlying psychological or emotional issues. It is essential to discuss your experiences with your healthcare provider to determine the appropriate course of action and address any potential underlying causes.
9. Is keeping a sleep diary helpful in managing medication-related nightmares?
A sleep diary can be a useful tool in understanding patterns and triggers for medication-related nightmares. Keeping track of your sleep quality, medication schedule, and any associated nightmares can help you and your healthcare provider make informed decisions regarding your treatment plan.
10. Can adjusting the dosage or switching medication prevent medication-related nightmares?
In some cases, adjusting the dosage or switching to a different medication within the same category can help alleviate medication-related nightmares. However, this can vary depending on individual responses and the specific medication involved. Consulting with your healthcare provider is crucial in finding the most appropriate solution for your situation.








