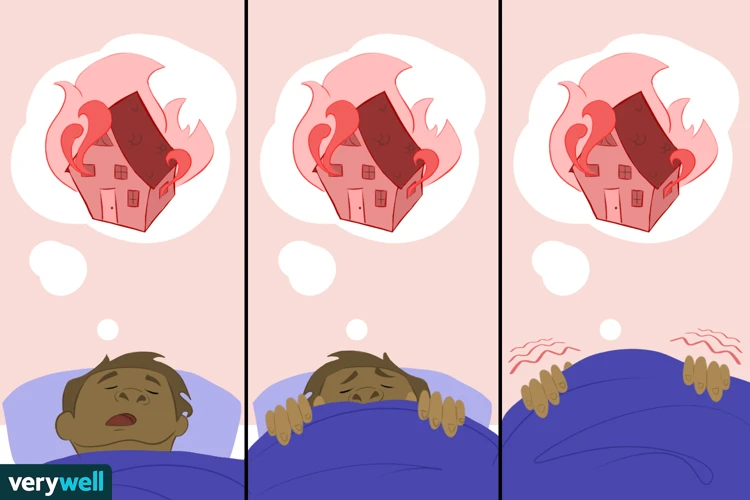
Tossing and turning in bed, plagued by vivid and unsettling nightmares, can be a distressing experience. What many people may not realize is that certain medications they are taking could be the culprit behind these haunting dreams. It’s an unsettling link that can leave individuals perplexed and searching for answers. In this article, we will delve into the connection between medications and nightmares, identifying common medications that have been known to cause this unsettling side effect. We will also explore how these medications can trigger nightmares, discussing the underlying mechanisms at play. Finally, we will provide strategies to minimize nightmares caused by medications, offering practical tips to help individuals find relief and restore peaceful sleep. So, if you’re curious about understanding the link between medications and nightmares, keep reading to unravel this mysterious connection.
Common Medications That Can Cause Nightmares
Antidepressant medications, often prescribed to manage depression and anxiety, can sometimes cause nightmares as a side effect. Selective serotonin reuptake inhibitors (SSRIs) like Prozac, Zoloft, and Paxil, commonly used to treat depression, have been associated with an increase in vivid and disturbing dreams. The exact mechanism behind this side effect is not fully understood, but it is believed to be linked to the alteration of serotonin levels in the brain.
Beta blockers, commonly used for the treatment of heart conditions such as high blood pressure and heart disease, have also been reported to cause nightmares in some individuals. While the precise relationship between beta blockers and nightmares remains unclear, it is believed to be linked to the drug’s impact on the central nervous system and possible disruption of REM sleep.
Certain medications prescribed for the management of Parkinson’s disease, such as levodopa, amantadine, and pramipexole, have been linked to an increased risk of nightmares. These medications work by regulating dopamine levels in the brain, and the alteration of dopamine levels may contribute to the occurrence of vivid and unsettling dreams.
Some cholesterol-lowering drugs, known as statins, have been associated with nightmares as a potential side effect. The exact mechanism by which these medications cause nightmares is not well understood, but it is believed to be related to the impact of statins on brain function and neurotransmitter activity.
Stimulant medications commonly prescribed for attention-deficit hyperactivity disorder (ADHD), such as Ritalin and Adderall, may also trigger nightmares in some individuals. The exact cause is not clear, but it is postulated that the stimulant effect on the brain’s neurotransmitters, such as dopamine and norepinephrine, may play a role in disrupting sleep patterns and triggering intense dreams.
It’s important to note that while these medications have been associated with nightmares, not everyone who takes them will experience this side effect. If you are experiencing disturbing dreams after starting a new medication, it is crucial to consult with your healthcare provider for further evaluation and guidance.
1. Antidepressants
Antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), are widely prescribed for the treatment of depression and anxiety disorders. While they can be effective in managing these conditions, one potential side effect that some individuals may experience is an increase in nightmares. The specific mechanisms by which antidepressants cause nightmares are not yet fully understood, but research suggests that alterations in serotonin levels in the brain may play a role. Serotonin is a neurotransmitter that regulates mood, sleep, and dreaming. When levels of serotonin are disrupted, it can lead to changes in dreaming patterns, including an increase in vivid and unsettling dreams.
Additionally, antidepressants may affect other neurotransmitters involved in sleep and dreaming, such as norepinephrine and dopamine, further contributing to nightmare occurrence. The disruption of these neurotransmitters can lead to alterations in sleep architecture and REM sleep, the stage of sleep where dreaming occurs most frequently. As a result, individuals taking antidepressants may experience more intense and disturbing dreams.
It is worth noting that not all individuals who take antidepressants will experience nightmares. The occurrence of nightmares as a side effect can vary from person to person. Factors such as individual susceptibility, dosage, and duration of medication use may influence the likelihood of experiencing nightmares.
If you are concerned about the impact of antidepressants on your sleep and dreaming patterns, it is important to speak with your healthcare provider. They can provide guidance and potentially adjust your medication regimen if necessary. Additionally, practicing good sleep hygiene and implementing relaxation techniques, such as meditation or deep breathing exercises, may also help mitigate the occurrence of nightmares. If nightmares persist or significantly interfere with your daily life, it may be beneficial to seek further evaluation from a sleep specialist or therapist who specializes in sleep disorders. They can offer additional strategies and treatments to address any sleep disturbances you may be experiencing.
2. Beta Blockers
Beta blockers are a class of medications commonly prescribed for various cardiovascular conditions, including high blood pressure, heart disease, and arrhythmias. While they are generally effective and well-tolerated, some individuals may experience nightmares as a side effect. The link between beta blockers and nightmares is not fully understood, but researchers believe it may be related to the impact these medications have on the central nervous system. Beta blockers work by blocking the effects of adrenaline and other stress hormones, which can potentially disrupt normal sleep patterns and lead to the occurrence of vivid and unsettling dreams. Additionally, beta blockers may interfere with the rapid eye movement (REM) stage of sleep, which is when most dreams occur. This disruption of REM sleep can contribute to the intensity and frequency of nightmares. If you are prescribed beta blockers and are experiencing troubling dreams, it is important to discuss this side effect with your healthcare provider. They may be able to adjust the dosage or timing of the medication to minimize the impact on your sleep and help alleviate the occurrence of nightmares.
3. Medications for Parkinson’s Disease
Medications used in the treatment of Parkinson’s disease, such as levodopa, amantadine, and pramipexole, have been found to potentially increase the occurrence of nightmares in some individuals. Parkinson’s disease is a neurological disorder characterized by the loss of dopamine-producing cells in the brain. These medications aim to improve dopamine function to alleviate symptoms, but they can also affect the sleep-wake cycle and dream patterns. Levodopa, in particular, is converted to dopamine in the brain and can cause fluctuations in dopamine levels, leading to vivid and unsettling dreams. Amantadine, commonly used to reduce Parkinson’s disease symptoms, can alter neurotransmitter activity and disrupt normal sleep patterns, potentially contributing to the occurrence of nightmares. Pramipexole, a dopamine agonist, binds to dopamine receptors in the brain and can also influence dream content. It’s important for individuals taking Parkinson’s disease medications to be aware of the possible risk of nightmares and discuss any concerns with their healthcare provider. If nightmares persist and significantly impact quality of life, seeking guidance from a sleep specialist or therapist may be beneficial in managing sleep disturbances. Sleep disorders and nightmares can often have a significant impact on daily functioning, so taking proactive steps to address these issues is crucial.
4. Cholesterol-lowering Drugs
Cholesterol-lowering drugs, also known as statins, have been found to potentially contribute to the occurrence of nightmares in some individuals. Although the exact mechanism is not fully understood, studies have suggested a correlation between statin use and an increase in vivid and disturbing dreams. Statins work by inhibiting an enzyme involved in cholesterol production, but they may also affect other pathways in the brain, leading to alterations in neurotransmitter function and sleep patterns.
One theory is that statins can disrupt the balance of serotonin, a neurotransmitter involved in regulating mood and sleep. Since serotonin plays a crucial role in sleep-wake cycles and dreaming, any disruption in its levels can potentially trigger nightmares. Another hypothesis is that statins may affect other neurotransmitters, such as dopamine or noradrenaline, which could impact sleep quality and contribute to unsettling dreams.
It’s important to note that not everyone who takes cholesterol-lowering drugs will experience nightmares, and the occurrence of this side effect varies from person to person. Some individuals may be more susceptible to the effects of statins on sleep and dreaming, while others may not be affected at all.
If you are taking cholesterol-lowering drugs and experiencing disturbing nightmares, it is essential to discuss this with your healthcare provider. They can evaluate whether the medication is causing the nightmares or if there may be other underlying factors contributing to the phenomenon. Your healthcare provider may consider adjusting the dosage or exploring alternative medications to manage your cholesterol levels if the nightmares are significantly affecting your sleep and well-being.
Additionally, addressing lifestyle factors such as stress, sleep hygiene, and overall mental well-being may also help minimize the impact of nightmares. If stress is a significant factor contributing to the nightmares, you may find it helpful to explore stress management techniques and seek support from a healthcare professional specializing in stress management. This can provide insights into stress-induced nightmares and offer strategies for better sleep and overall mental health.
5. ADHD Medications
ADHD medications, such as Ritalin and Adderall, are commonly prescribed to help manage symptoms of attention-deficit hyperactivity disorder. However, it’s worth noting that these medications may have the potential to induce nightmares in some individuals. While the exact cause of this side effect is not fully understood, there are a few theories as to why ADHD medications might trigger intense dreams.
One possible explanation is the impact of these medications on neurotransmitters in the brain. ADHD medications, particularly stimulants like Ritalin and Adderall, work by increasing the levels of dopamine and norepinephrine, which are neurotransmitters involved in regulating attention and focus.
The increase in neurotransmitter activity, particularly dopamine, may disrupt normal sleep patterns and affect REM (rapid eye movement) sleep, which is the stage of sleep associated with dreaming. This disruption can lead to more vivid and intense dreams, including nightmares.
Additionally, the stimulating effects of ADHD medications themselves can contribute to the occurrence of nightmares. These medications can increase heart rate and blood pressure, which may heighten arousal during sleep and influence the content of dreams.
It is crucial for individuals taking ADHD medications to discuss any concerns or side effects, including nightmares, with their healthcare provider. They can provide guidance on managing these side effects, such as adjusting the dosage or trying alternative medications. It’s important to find the right balance between managing ADHD symptoms effectively while minimizing any potential disruption to sleep and dreams. Remember, every individual’s experience may differ, and open communication with a healthcare professional is key to finding the best approach for each person’s unique needs.
How Medications Can Trigger Nightmares
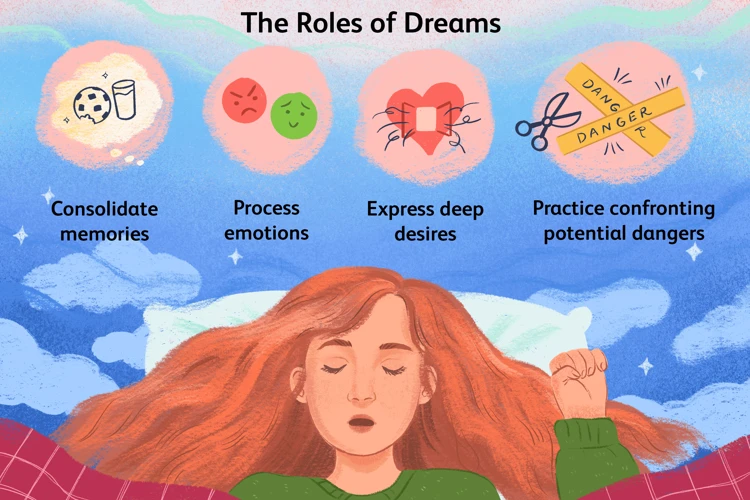
Medications can trigger nightmares through various mechanisms that affect brain chemistry and sleep patterns. Understanding these mechanisms can provide insights into why certain drugs have the potential to induce vivid and unsettling dreams.
Neurochemical Imbalance: Medications that alter neurotransmitter levels in the brain, such as antidepressants and Parkinson’s disease drugs, can disrupt the delicate balance of chemicals responsible for regulating mood and sleep. For example, antidepressants, which increase serotonin levels, may inadvertently lead to an overstimulation of serotonin receptors during REM sleep, contributing to the occurrence of nightmares.
Disruption of Sleep Patterns: Certain medications, including beta blockers and stimulants, can interfere with normal sleep architecture, causing disturbances in the REM (rapid eye movement) phase. REM sleep is when most dreams occur, and any disruption to this important sleep stage can increase the likelihood of experiencing nightmares. Additionally, medications that affect sleep duration or quality may lead to fragmented sleep, enhancing the intensity and vividness of dreams.
Side Effects on the Central Nervous System: Some drugs impact the central nervous system, altering brain activity and neurotransmitter function. This disruption can influence the content and intensity of dreams. Cholesterol-lowering drugs like statins, despite their unclear mechanism, are thought to potentially affect brain function, including sleep regulation, which may contribute to the occurrence of nightmares.
It’s worth mentioning that individual responses to medications can vary, and not everyone will experience nightmares as a side effect. Factors such as dosage, duration of medication use, and personal susceptibility can influence the likelihood of experiencing medication-induced nightmares. If you are concerned about nightmares caused by medications, discussing your symptoms and concerns with your healthcare provider is crucial in determining the most appropriate course of action.
1. Neurochemical Imbalance
Neurochemical imbalance refers to an alteration in the levels or activity of neurotransmitters in the brain, which can contribute to the occurrence of nightmares. Neurotransmitters, such as serotonin, dopamine, and norepinephrine, play a crucial role in regulating various brain functions, including sleep and dreaming.
When there is an imbalance in these neurotransmitters, it can disrupt the normal sleep-wake cycle and lead to vivid and disturbing dreams. For example, a decrease in serotonin levels has been linked to an increase in nightmares. This is why certain medications, such as antidepressants that modulate serotonin levels, can sometimes trigger nightmares as a side effect.
Similarly, an increase in dopamine activity in the brain has also been associated with the occurrence of nightmares. Medications that affect dopamine levels, such as those used to manage Parkinson’s disease, may disrupt the delicate balance of neurotransmitters and contribute to the development of intense dreams.
Norepinephrine, a neurotransmitter involved in the body’s stress response, has been implicated in nightmares. High levels of stress and anxiety, which can alter norepinephrine activity, have been linked to an increased likelihood of experiencing nightmares. In some cases, medications that impact norepinephrine levels, like certain antidepressants or ADHD medications, may inadvertently contribute to nightmare occurrence.
Understanding and addressing neurochemical imbalances is essential in managing medication-related nightmares. By working closely with healthcare providers and possibly adjusting medication dosage or exploring alternative treatments, individuals may be able to restore the delicate balance of neurotransmitters in the brain and reduce the occurrence of nightmares.
In the next section, we will explore another possible mechanism by which medications can trigger nightmares: the disruption of sleep patterns. If you’re interested in learning more about this topic, click here to read our article on sleep disorders and nightmares.
2. Disruption of Sleep Patterns
Disruption of sleep patterns is another way in which medications can trigger nightmares. Sleep is a complex process consisting of multiple stages, including rapid eye movement (REM) sleep, during which most dreaming occurs. When medications interfere with the normal sleep cycle, it can lead to an increased occurrence of nightmares.
Certain medications, such as antidepressants and beta blockers, mentioned earlier, have the potential to disrupt REM sleep. Antidepressants, particularly SSRIs, have been shown to suppress REM sleep and increase the time spent in non-REM sleep stages. This altered sleep architecture can result in more intense and vivid dreams during the REM period.
Additionally, beta blockers, usually prescribed for heart conditions, may impact sleep patterns by reducing the release of adrenaline and slowing down heart rate. These physiological changes can interfere with the natural sleep cycle and increase the likelihood of experiencing nightmares.
Medications used to treat Parkinson’s disease, such as levodopa, have been known to disrupt sleep patterns. These medications can cause sleep fragmentation, meaning individuals may wake up more frequently during the night, preventing them from reaching deep, restorative sleep. As a result, dreams, including nightmares, may occur more frequently during the periods of REM sleep that do happen.
Interestingly, disruptions in sleep patterns can also contribute to the development of stress-related nightmares. When the quality of sleep is compromised, the likelihood of experiencing nightmares associated with stress and anxiety increases. To learn more about the connection between stress and nightmares, you can read our article here.
Medications that disrupt sleep patterns can contribute to the occurrence of nightmares. By affecting REM sleep or causing sleep fragmentation, these medications alter the normal sleep architecture and increase the likelihood of vivid and unsettling dreams. It is important to discuss any sleep disturbances or nightmares with your healthcare provider, as they can provide guidance and potentially make adjustments to your medication regimen to minimize this side effect.
3. Side Effects on the Central Nervous System
Side effects on the central nervous system can contribute to the occurrence of nightmares in individuals taking certain medications. In particular, medications such as beta blockers and some Parkinson’s disease medications have been associated with this phenomenon. Beta blockers work by blocking the effects of adrenaline, which can affect the balance of neurotransmitters in the brain and disrupt sleep patterns. This disruption in the central nervous system can lead to more vivid and disturbing dreams. Similarly, medications used to manage Parkinson’s disease, such as levodopa, amantadine, and pramipexole, can impact dopamine levels in the brain. Disruptions in dopamine levels can influence the sleep-wake cycle and REM sleep, potentially leading to an increase in nightmares. Understanding the specific mechanisms through which these medications affect the central nervous system can provide insight into the occurrence of nightmares and guide healthcare providers in managing and mitigating this side effect. If you want to explore further the impact of trauma on nightmares, you can read our article on uncovering the impact of trauma on nightmares.
Strategies to Minimize Nightmares Caused by Medications
Open and honest communication with your healthcare provider is essential when experiencing nightmares caused by medications. They can review your medication regimen and determine if any adjustments need to be made. Your doctor may be able to switch you to a different medication that is less likely to cause nightmares or adjust your dosage to minimize the side effects.
In some cases, adjusting the dosage or timing of your medication may help reduce nightmares. Your healthcare provider may suggest taking certain medications in the morning instead of at night or vice versa. By altering the timing, you may be able to minimize the impact on your sleep cycle and decrease the likelihood of nightmares.
If nightmares persist despite dosage adjustments, your doctor may consider exploring alternative medications or treatments. They can assess whether there are alternative drugs that can effectively treat your condition without causing nightmares. It’s important to never make changes to your medication regimen without consulting your healthcare provider first.
Maintaining good sleep hygiene can help improve the quality of your sleep and potentially minimize nightmares. Establish a relaxing bedtime routine, create a peaceful sleep environment, avoid stimulating activities before bed, and prioritize getting enough sleep each night. These practices can contribute to better overall sleep and potentially reduce the occurrence of nightmares.
Working with a therapist or counselor experienced in sleep disorders can be beneficial for managing nightmares caused by medications. They can help you develop coping strategies, address any underlying anxiety or stress that may contribute to nightmares, and provide guidance on relaxation techniques that promote better sleep. Cognitive-behavioral therapy for insomnia (CBT-I) may also be an option to explore.
Remember, everyone’s experience with medications and nightmares is unique, so it’s crucial to work closely with your healthcare provider to find the most appropriate strategies for your specific situation. By taking proactive steps and utilizing the support of medical professionals, you can minimize the impact of nightmares caused by medications and improve your overall sleep quality.
1. Communicate with Your Healthcare Provider
When experiencing nightmares as a side effect of medication, it is crucial to communicate openly and honestly with your healthcare provider. Your healthcare provider plays a vital role in managing and monitoring your medications. Discussing the issue of nightmares with them can help you understand whether your medication could be the cause and if there are any alternative options available. During your conversation, consider sharing details about the frequency, intensity, and content of your nightmares. Additionally, it is essential to mention any other side effects you may be experiencing. The information you provide will assist your healthcare provider in determining the best course of action moving forward. Remember, open communication is key to finding a solution that works best for you and your specific situation.
2. Adjust Dosage or Timing
When it comes to minimizing nightmares caused by medications, one strategy that can be effective is adjusting the dosage or timing of the medication. In some cases, the dosage of the medication may be too high for an individual, leading to an increased likelihood of experiencing nightmares. By working closely with your healthcare provider, you can discuss the possibility of adjusting the dosage to find the right balance that reduces the occurrence of nightmares.
Timing of medication administration can also play a role in nightmare occurrence. Some medications may have a greater impact on sleep and dream activity depending on when they are taken. For example, taking a medication that tends to cause nightmares right before bed may increase the likelihood of experiencing vivid dreams during the night. By adjusting the timing of medication ingestion, it may be possible to minimize the potential for nightmares. Your healthcare provider can provide guidance on the optimal timing that minimizes the risk of disturbing dreams.
It’s important to note that any adjustments to dosage or timing should always be done in consultation with your healthcare provider. They have the expertise to evaluate your individual situation and provide personalized recommendations. It’s crucial to follow their guidance and closely monitor the effects of any adjustments made to ensure both the desired therapeutic benefits and a reduction in nightmares.
3. Explore Alternative Medications or Treatments
When nightmares persist and become a significant source of distress, exploring alternative medications or treatments may be a viable option. Discussing your concerns with your healthcare provider is essential in determining the best course of action. They can evaluate your individual situation and consider alternative medications that are less likely to cause nightmares. For example, if you are taking an antidepressant that is causing vivid dreams, your doctor might suggest switching to a different class of antidepressants or exploring non-pharmaceutical approaches like therapy or counseling. Additionally, alternative treatments such as cognitive-behavioral therapy for insomnia (CBT-I) or relaxation techniques may help address the underlying causes of nightmares and improve overall sleep quality. It’s important to remember that finding the right medication or treatment may require some trial and error, as individual responses can vary. Patience and open communication with your healthcare provider are key to exploring alternative options that can minimize nightmares while effectively managing your health condition.
4. Practice Good Sleep Hygiene
Maintaining good sleep hygiene is crucial in minimizing nightmares caused by medications. Here are some strategies to promote better sleep and reduce the occurrence of unsettling dreams:
1. Create a Relaxing Bedtime Routine: Establish a calming routine before bed to signal to your body that it’s time to sleep. This can include engaging in relaxing activities such as reading a book, taking a warm bath, or practicing meditation or deep breathing exercises.
2. Ensure a Comfortable Sleep Environment: Make sure your bedroom is conducive to sleep. Keep the room dark, quiet, and at a comfortable temperature. Use comfortable bedding and a supportive mattress that suits your preferences.
3. Avoid Stimulants and Heavy Meals: Avoid consuming stimulants like caffeine or nicotine close to bedtime, as they can interfere with sleep. Additionally, refrain from consuming heavy or spicy meals late in the evening, as they can cause discomfort and disrupt sleep.
4. Establish a Consistent Sleep Schedule: Try to go to bed and wake up at the same time each day, even on weekends. This helps regulate your body’s internal clock and promotes better sleep quality.
5. Create a Sleep-Friendly Environment: Make your bedroom a dedicated space for sleep and relaxation. Avoid using electronic devices, such as smartphones or tablets, in bed as the blue light emitted by these devices can interfere with the production of melatonin, a hormone that regulates sleep.
6. Exercise Regularly: Engage in regular physical activity during the day, as it can help promote better sleep. However, avoid vigorous exercise too close to bedtime, as it may increase alertness and make it more difficult to fall asleep.
7. Manage Stress: Practice stress management techniques such as mindfulness, relaxation exercises, or journaling to help reduce stress levels before bed. High levels of stress can contribute to vivid and unsettling dreams.
By incorporating these practices into your daily routine, you can create a sleep-friendly environment and promote better sleep quality, which in turn can help minimize the occurrence of nightmares caused by medications. Remember to consult with your healthcare provider for personalized advice and guidance if you continue to experience distressing dreams.
5. Seek Therapy or Counseling
If nightmares persist or become significantly distressing despite trying other strategies, seeking therapy or counseling can be an effective approach to address and mitigate the impact of these unsettling dreams. Therapy can help individuals explore and process the emotional and psychological factors that may contribute to the frequency or intensity of nightmares.
One therapeutic modality that has shown promise in treating nightmares is cognitive-behavioral therapy for nightmares (CBT-N). CBT-N focuses on identifying and challenging negative thought patterns and beliefs related to nightmares. Therapists may use techniques such as imagery rehearsal therapy (IRT), where individuals practice mentally rewriting the content of their dreams to create more positive and less frightening scenarios.
Additionally, trauma-focused therapy may be beneficial for individuals who have experienced past trauma, as trauma can often manifest in nightmares. Therapies like Eye Movement Desensitization and Reprocessing (EMDR) or narrative exposure therapy (NET) can assist in processing and resolving traumatic experiences, potentially reducing the frequency and intensity of nightmares.
Counseling sessions can also provide a safe and supportive space for individuals to discuss their fears, anxieties, and concerns related to nightmares. Therapists can offer guidance on stress management techniques, relaxation exercises, and coping strategies to help individuals better navigate the emotional impact of nightmares.
It’s important to note that therapy or counseling should be pursued in conjunction with, and not as a replacement for, any necessary medical or pharmacological interventions. Collaborating with healthcare providers and mental health professionals can ensure a comprehensive approach to addressing nightmares and their underlying causes.
Conclusion
In conclusion, it is evident that there is a link between certain medications and nightmares. From antidepressants and beta blockers to medications for Parkinson’s disease, cholesterol-lowering drugs, and ADHD medications, these commonly prescribed drugs have been associated with an increased risk of vivid and unsettling dreams. While the exact mechanisms vary, they may involve neurochemical imbalances, disruptions in sleep patterns, and side effects on the central nervous system.
However, it is essential to remember that not everyone will experience nightmares as a side effect of these medications. If you are concerned about the occurrence of disturbing dreams, it is crucial to communicate with your healthcare provider. They can evaluate your specific situation, consider adjusting the dosage or timing of your medication, explore alternative medications or treatments, and provide guidance on practicing good sleep hygiene.
Seeking therapy or counseling may also be beneficial in managing nightmares caused by medications. A mental health professional can help you cope with the emotional impact of recurring nightmares and provide strategies to address stress and anxiety, which may contribute to their occurrence.
It’s important to prioritize your mental and emotional well-being and take proactive steps to minimize the impact of nightmares on your quality of life. By working closely with your healthcare provider and implementing effective strategies, you can find relief and achieve restful nights of sleep devoid of haunting dreams.
Frequently Asked Questions
1. Can nightmares be a side effect of antidepressant medication?
Yes, some antidepressant medications, particularly selective serotonin reuptake inhibitors (SSRIs), have been associated with an increased risk of nightmares as a side effect.
2. Do beta blockers have the potential to cause nightmares?
While the exact relationship is not fully understood, beta blockers have been reported to cause nightmares in certain individuals, potentially due to their impact on the central nervous system and disruption of REM sleep.
3. Can medications used for Parkinson’s disease trigger nightmares?
Yes, medication used to manage Parkinson’s disease, such as levodopa, amantadine, and pramipexole, have been linked to an increased risk of nightmares, possibly due to their impact on dopamine levels in the brain.
4. Do cholesterol-lowering drugs have the potential to cause nightmares?
Yes, some cholesterol-lowering drugs, known as statins, have been associated with nightmares as a potential side effect. The precise mechanism behind this is not yet fully understood.
5. Can ADHD medications lead to nightmares?
Stimulant medications commonly prescribed for ADHD, such as Ritalin and Adderall, have been reported to trigger nightmares in some individuals. The exact cause is not known, but it is believed to be related to the impact of these medications on neurotransmitters in the brain.
6. How do antidepressants cause nightmares?
The exact mechanism is not entirely clear, but it is thought that the alteration of serotonin levels in the brain, caused by antidepressants like SSRIs, may contribute to the occurrence of nightmares.
7. Are nightmares a common side effect of beta blockers?
Nightmares are not a commonly reported side effect of beta blockers, but they have been reported in some individuals. The frequency of nightmares as a side effect can vary.
8. Should I be concerned if I experience nightmares while taking medication for Parkinson’s disease?
If you are experiencing nightmares after starting medication for Parkinson’s disease, it is important to discuss these symptoms with your healthcare provider to determine the best course of action. They may be able to adjust your medication regimen or provide alternative treatment options.
9. Are nightmares experienced by all individuals taking cholesterol-lowering drugs?
No, not everyone who takes cholesterol-lowering drugs will experience nightmares. However, it is still important to be aware of the potential side effects and speak with your healthcare provider if you have concerns.
10. Can adjusting the dosage or timing of medications help alleviate nightmares?
Adjusting the dosage or timing of medications can sometimes help minimize nightmares. It is advisable to discuss any concerns with your healthcare provider, who can provide guidance on potential adjustments.








