Insomnia and depression, two seemingly unrelated conditions, often go hand in hand, leaving individuals trapped in a vicious cycle of sleeplessness and emotional distress. The relentless inability to sleep can significantly impact mental health, exacerbating existing symptoms of depression and increasing the risk of developing a depressive disorder. Likewise, depression can disrupt sleep patterns, further intensifying insomnia. This intricate interplay between insomnia and depression has captured the attention of researchers, who are striving to unravel the link between the two and develop effective treatments. Understanding the complex relationship between insomnia and depression is crucial in order to provide comprehensive care and support for those affected by these debilitating conditions. So, let’s explore the profound link between insomnia and depression, shedding light on the causes, symptoms, interconnection, and potential treatment approaches to alleviate the burden of these intertwined afflictions.
The Definition and Causes of Insomnia
Insomnia, often referred to as a sleep disorder, is characterized by persistent difficulty falling asleep or staying asleep, despite having the opportunity to do so. It is a condition that affects a significant portion of the population and can lead to a wide range of physical and mental health issues. There are two main types of insomnia: acute and chronic. Acute insomnia is short-term and typically occurs in response to a specific event or circumstance, such as jet lag or a stressful life event. On the other hand, chronic insomnia is more long-term, lasting for at least three nights a week for three months or more. So, what causes insomnia? Well, there are several common triggers. Stress, anxiety, and depression are all known culprits that can disrupt the sleep-wake cycle. Other factors include poor sleep hygiene, such as irregular sleep schedules or engaging in stimulating activities before bedtime. Additionally, certain medical conditions, medications, and lifestyle choices, such as excessive caffeine intake or smoking, can contribute to the development of insomnia. Managing stress, maintaining a healthy diet, and exploring natural remedies for insomnia can all play a role in improving sleep quality and mitigating the impact of this sleep disorder. (Link: explore-insomnia-stress)
1. Types of Insomnia
There are two main types of insomnia: acute and chronic. Acute insomnia is typically short-term and occurs in response to a specific event or circumstance. It can be caused by various factors such as environmental changes, jet lag, or temporary stressors. This type of insomnia often resolves on its own once the underlying cause is addressed. On the other hand, chronic insomnia is a more long-term condition that lasts for at least three nights a week for three months or more. It can be caused by psychological factors like anxiety, depression, or chronic stress, as well as underlying medical conditions such as sleep apnea or restless legs syndrome. Chronic insomnia requires proper diagnosis and treatment to improve sleep patterns and overall well-being. It is essential to address the underlying causes of insomnia to effectively manage and treat the condition. Exploring strategies such as maintaining a healthy diet (diet-managing-insomnia) and considering natural remedies for insomnia (natural-remedies-insomnia) can also be helpful in improving sleep quality.
2. Common Causes of Insomnia
There are various common causes of insomnia that can significantly disrupt an individual’s sleep patterns. Understanding these causes is crucial in order to address and alleviate the symptoms of insomnia. One prevalent cause is stress, which can activate the body’s ‘fight or flight’ response, leading to hyperarousal and difficulty falling asleep. Additionally, anxiety disorders, such as generalized anxiety disorder or post-traumatic stress disorder, can contribute to insomnia. Depression is another factor that often accompanies insomnia, as the overwhelming sense of sadness and hopelessness can make it challenging to find restful sleep. Certain lifestyle factors can also play a role in the development of insomnia. Poor sleep hygiene, including irregular sleep schedules, excessive use of electronic devices before bedtime, and a disruptive sleep environment, can all contribute to difficulty falling asleep. Consuming stimulants like caffeine or nicotine close to bedtime can also disrupt sleep patterns. Medical conditions such as chronic pain, respiratory problems, or hormonal imbalances may interfere with sleep. Medications or substances that have stimulating effects can also cause insomnia as a side effect. It is important to identify and address these common causes of insomnia in order to develop appropriate treatment plans and support individuals in achieving restful and restorative sleep. (Link: diet-managing-insomnia)
3. Impact of Insomnia on Mental Health
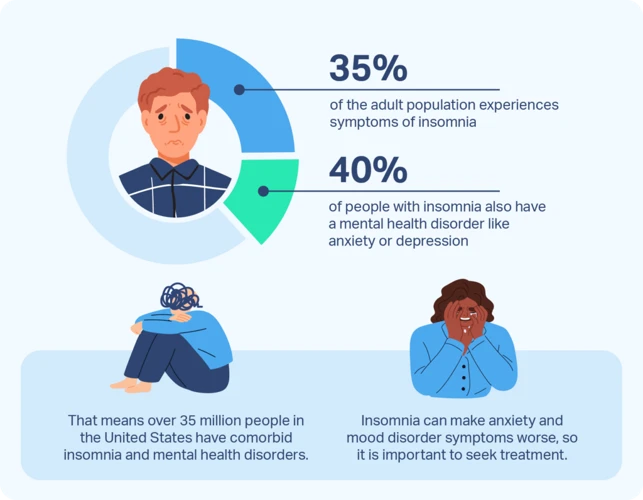
Insomnia not only affects our physical well-being but also has a significant impact on our mental health. The lack of quality sleep can exacerbate existing mental health conditions and contribute to the development of new ones.
One of the primary effects of insomnia on mental health is the increased risk of developing depression. Numerous studies have shown a strong association between insomnia and depression, with individuals suffering from insomnia being two to three times more likely to develop depression than those who sleep well. The disrupted sleep patterns can disrupt the brain’s chemistry and contribute to the dysregulation of mood-regulating neurotransmitters.
Insomnia also intensifies symptoms of anxiety. Sleep deprivation impairs our ability to regulate emotions and increases our sensitivity to stressors, making us more prone to heightened anxiety levels. The constant fatigue and irritability caused by insomnia can further fuel feelings of restlessness and unease.
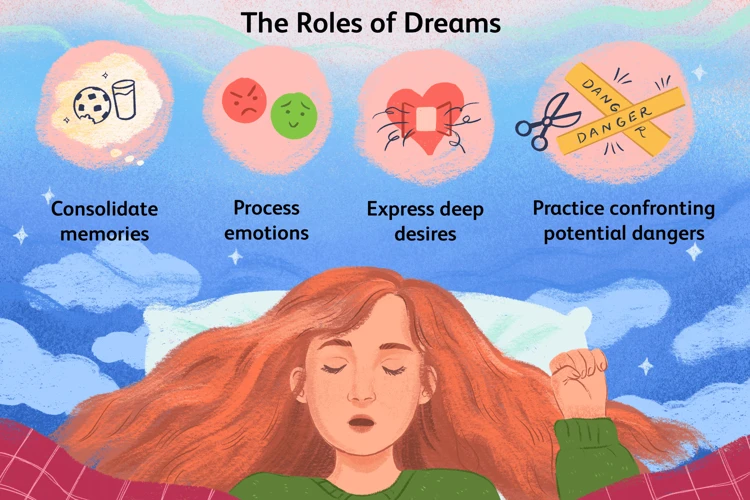
Additionally, insomnia can impact cognitive function and impair our ability to concentrate, remember things, and make decisions. The brain’s ability to process information and consolidate memories relies on adequate sleep, and the lack thereof can hinder these processes. This cognitive impairment can interfere with daily functioning and exacerbate feelings of frustration and low self-esteem.
Insomnia can lead to a vicious cycle of poor mental health and sleeplessness. The distress caused by insomnia can trigger negative thoughts and rumination, making it difficult to quiet the mind and fall asleep. This perpetuates the cycle, making it even more challenging to overcome insomnia and address underlying mental health issues.
To break free from this cycle, it is crucial to recognize the impact of insomnia on mental health and seek appropriate treatment and support. Prioritizing good sleep hygiene, adopting relaxation techniques, and engaging in stress-reducing activities can all contribute to improving sleep quality and alleviating the detrimental effects of insomnia on mental health.
The Definition and Symptoms of Depression
Depression, also known as major depressive disorder (MDD), is a mood disorder characterized by persistent feelings of sadness, hopelessness, and a loss of interest or pleasure in activities. It goes beyond the normal ups and downs of life and can significantly impact a person’s daily functioning and overall well-being. The symptoms of depression can vary from person to person but generally include persistent feelings of sadness or emptiness, decreased energy and fatigue, changes in appetite and weight, difficulty concentrating, feelings of guilt or worthlessness, sleep disturbances such as insomnia or excessive sleep, and thoughts of death or suicide. It is important to note that not everyone experiences the same symptoms, and the severity and duration of symptoms can also vary. The diagnosis of depression is made by a healthcare professional based on a thorough evaluation of the individual’s symptoms, medical history, and any associated factors. Recognizing the signs and symptoms of depression is crucial in order to seek appropriate treatment and support for those affected.
1. Major Depressive Disorder (MDD)
Major Depressive Disorder (MDD) is a common form of depression that affects millions of people worldwide. It is a debilitating mental health condition characterized by persistent feelings of sadness, hopelessness, and a loss of interest or pleasure in activities. MDD often interferes with daily functioning and can significantly impact a person’s overall quality of life. The exact causes of MDD are not fully understood, but a combination of genetic, biological, environmental, and psychological factors is believed to contribute to its development. Some individuals may be more genetically predisposed to MDD, while others may experience an imbalance in certain neurotransmitters, such as serotonin or dopamine. Traumatic life events, chronic stress, a history of abuse or neglect, and certain medical conditions can also increase the risk of developing MDD. It’s important to note that MDD is different from experiencing occasional sadness or grief, as it is a persistent and chronic condition that requires professional intervention and treatment. (Link: depression-treatment-options)
2. Symptoms of Depression
Depression, a mood disorder that affects millions of people worldwide, is characterized by persistent feelings of sadness, hopelessness, and a lack of interest or pleasure in activities. The symptoms of depression can vary from person to person, but there are common signs to look out for. Persistent feelings of sadness or emptiness, loss of interest in previously enjoyed activities, and a significant decrease or increase in appetite are all indicative of depression. Fatigue, decreased energy, and difficulty concentrating or making decisions are commonly reported. Individuals with depression may also experience feelings of guilt or worthlessness and have recurrent thoughts of death or suicide. Changes in sleep patterns, such as insomnia or excessive sleeping, can also be a symptom of depression. Physical symptoms, such as headaches, digestive issues, or chronic pain, may also accompany depression. It is important to note that not everyone with depression experiences all of these symptoms, and the severity can vary. If you or someone you know is experiencing prolonged and distressing symptoms of depression, it is essential to seek professional help for diagnosis and treatment.
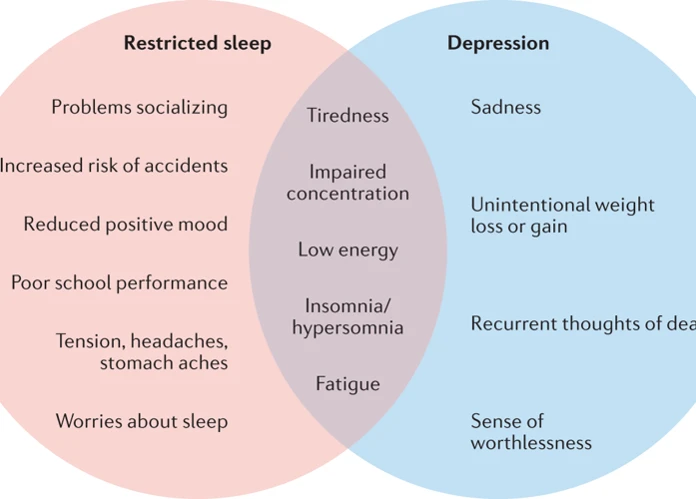
The Interconnection Between Insomnia and Depression
Insomnia and depression are intricately interconnected, with each condition exacerbating the other in a bidirectional relationship. Firstly, insomnia can act as a risk factor for the development of depression. The relentless struggle to fall asleep or stay asleep can lead to feelings of frustration, irritability, and daytime fatigue. These symptoms, in turn, can contribute to the onset or worsening of depressive symptoms. Chronic sleep deprivation disrupts the balance of neurotransmitters in the brain, such as serotonin and dopamine, which are crucial for regulating mood. This imbalance can further contribute to the development of depressive symptoms.
Similarly, depression can also cause or worsen insomnia. The emotional distress associated with depression, including feelings of sadness, hopelessness, and anxiety, can make it difficult for individuals to relax and fall asleep. Individuals with depression often experience intrusive thoughts, excessive worrying, and rumination, which can keep the mind in an agitated state, hindering the ability to achieve restful sleep. Additionally, changes in sleep architecture, such as reduced REM sleep, may be seen in individuals with depression, further contributing to the insomnia symptoms. The interconnection between insomnia and depression highlights the importance of addressing both conditions simultaneously in order to effectively manage and improve overall well-being.
1. Bidirectional Relationship
The relationship between insomnia and depression is bidirectional, meaning that each condition can contribute to and exacerbate the other. Individuals with insomnia are more likely to experience symptoms of depression, and those with depression are at a higher risk of developing insomnia. This bidirectional relationship creates a cycle of sleep disruption and emotional distress. Insomnia can lead to feelings of fatigue, irritability, and difficulty concentrating, which are common symptoms of depression. Additionally, the chronic sleep deprivation associated with insomnia can impair cognitive function and decrease the ability to regulate emotions effectively. This, in turn, can further contribute to the development or worsening of depressive symptoms. On the other hand, depression itself can disrupt sleep patterns and lead to insomnia. The negative thoughts, anxiety, and rumination often associated with depression can interfere with falling asleep or staying asleep throughout the night. This bidirectional relationship highlights the interconnectedness of these two conditions and emphasizes the importance of addressing both insomnia and depression in treatment approaches to achieve lasting improvements in mental well-being.
2. Insomnia as a Risk Factor for Depression
Insomnia, with its disruptive effects on sleep patterns and the body’s natural circadian rhythm, can act as a significant risk factor for depression. The link between insomnia and depression is bidirectional, with each condition contributing to the development and exacerbation of the other. When individuals experience chronic insomnia, it creates a state of chronic hyperarousal and heightened activity in the brain, resulting in increased vulnerability to negative emotions and a reduced ability to regulate mood. Sleep deprivation caused by insomnia also leads to impaired cognitive function and emotional regulation, making it more difficult to cope with stressors and increasing the likelihood of developing depression. Additionally, the persistent fatigue and exhaustion experienced by individuals with insomnia can lead to feelings of hopelessness, sadness, and a loss of interest in activities, all of which are symptoms commonly associated with depression. Addressing and treating insomnia is crucial in preventing the onset and progression of depression. By improving sleep quality and duration, individuals experiencing insomnia can reduce the risk of developing depression and enhance overall mental well-being.
3. Depression as a Cause of Insomnia
Depression, a mental health disorder characterized by persistent feelings of sadness, hopelessness, and a loss of interest in activities, can contribute significantly to the development and exacerbation of insomnia. Individuals with depression often experience disturbances in their sleep patterns, including difficulty falling asleep, staying asleep, or early morning awakenings. These sleep disturbances are believed to be caused by various factors. One possible mechanism is the dysregulation of neurotransmitters, such as serotonin and norepinephrine, which play a crucial role in regulating sleep-wake cycles and mood. When these neurotransmitters are imbalanced, it can disrupt the normal sleep architecture and lead to insomnia. Additionally, the emotional and cognitive symptoms associated with depression, such as rumination, excessive worry, and negative thinking patterns, can also contribute to sleep difficulties. Racing thoughts and an inability to calm the mind make it challenging to relax and fall asleep. Individuals with depression may experience heightened physiological arousal, including increased heart rate and elevated levels of stress hormones like cortisol, which can further interfere with sleep quality. Recognizing the role of depression as a cause of insomnia is vital in ensuring appropriate treatment and management approaches that address both conditions holistically. It is crucial to seek professional help to effectively tackle the underlying causes and provide relief from the intertwined symptoms of depression and insomnia.
The Impact of Insomnia on Depression Severity
Insomnia not only coexists with depression but also plays a significant role in exacerbating its severity. The impact of insomnia on depression is far-reaching and can worsen various aspects of mental well-being. One way in which insomnia affects depression severity is by disrupting emotional regulation. Sleep deprivation impairs the brain’s ability to regulate emotions, resulting in heightened emotional sensitivity and reactivity. This can lead to intensified feelings of sadness, irritability, and hopelessness, all key symptoms of depression. Additionally, insomnia contributes to increased rumination and negative thinking patterns. When individuals are unable to sleep, their minds often wander to distressing thoughts and worries, causing a spiral of negative thinking and self-criticism. This rumination can prolong depressive episodes and make it more challenging to break free from the grip of depression. The combination of sleep deprivation, emotional dysregulation, and negative thinking creates a vicious cycle, where insomnia intensifies depression, and depression perpetuates insomnia. This complex interplay highlights the importance of addressing both conditions simultaneously to effectively manage and alleviate the severity of depression.
1. Sleep Deprivation and Emotional Regulation
Sleep deprivation can have a profound impact on emotional regulation. When individuals do not obtain enough sleep, it impairs their ability to regulate emotions effectively. This can result in heightened irritability, difficulty managing stress, and increased emotional reactivity. A lack of sleep disrupts the prefrontal cortex, which is responsible for regulating emotions and decision-making. This impairment can lead to an intensified emotional response to everyday situations, making individuals more vulnerable to negative emotions such as anger, sadness, and anxiety. Sleep deprivation can also weaken the connection between the prefrontal cortex and the amygdala, which is involved in processing emotions. As a result, individuals experiencing sleep deprivation may find it more challenging to interpret and respond to emotional cues accurately. This can further contribute to emotional difficulties and potentially worsen symptoms of depression. Prioritizing good sleep hygiene and ensuring an adequate amount of sleep can play a crucial role in promoting emotional well-being and supporting mental health.
2. Increased Rumination and Negative Thinking
When insomnia and depression coexist, they create a dangerous synergy that amplifies negative thinking patterns and rumination. Insufficient sleep can impair cognitive functioning and emotional regulation, making it difficult for individuals to effectively process and manage their thoughts and emotions. This can result in an increased tendency to ruminate, dwelling on negative thoughts and experiences. The lack of restorative sleep prevents the brain from effectively consolidating memories and processing emotions, leading to a heightened focus on negative events or feelings.
Rumination, which is the repetitive and obsessive focus on negative thoughts, can intensify existing depressive symptoms. It traps individuals in a cycle of negative thinking, where they analyze and replay distressing events or situations, further deepening their feelings of sadness, hopelessness, and despair. This rumination can inhibit problem-solving abilities and hinder the development of adaptive coping strategies.
The negative thinking patterns associated with both insomnia and depression can create a distorted perception of reality, making it challenging to see positive aspects of life or find solutions to problems. These persistent negative thoughts can perpetuate feelings of worthlessness, self-blame, and guilt, fueling the depressive cycle.
It is crucial to address and manage both insomnia and depression together to break free from this detrimental cycle of negative thinking and rumination. By implementing effective treatment approaches that target both conditions, such as cognitive behavioral therapy for insomnia (CBT-I) and medication management, individuals can improve their sleep quality and mental well-being, ultimately reducing rumination and negative thinking.
Treatment Approaches for Insomnia and Depression
Treatment approaches for insomnia and depression aim to address both conditions simultaneously, recognizing the intricate relationship between them. One widely recommended treatment is Cognitive Behavioral Therapy for Insomnia (CBT-I). This therapy focuses on identifying and modifying the negative thought patterns and behaviors that contribute to insomnia. CBT-I typically involves techniques such as sleep restriction, stimulus control, relaxation training, and cognitive restructuring. It helps individuals develop healthy sleep habits, improve sleep hygiene, and reframe negative thoughts about sleep. In addition to CBT-I, medications may be prescribed to manage both insomnia and depression. Some antidepressant medications, such as selective serotonin reuptake inhibitors (SSRIs), have shown effectiveness in treating both conditions. These medications can regulate mood, improve sleep quality, and reduce symptoms of depression. However, it’s important to note that medication should be prescribed and monitored by a medical professional. It is also crucial to address lifestyle factors that contribute to both insomnia and depression. Exercise, stress management techniques, and a nutritious diet can all have a positive impact on sleep and mental health. Additionally, natural remedies such as herbal supplements or relaxation techniques can complement existing treatments. (Link: natural-remedies-insomnia) Taking a comprehensive approach that combines therapy, medication, and lifestyle modifications is often the most effective strategy for addressing both insomnia and depression. It is important to consult with healthcare professionals to determine the best treatment plan tailored to individual needs.
1. Cognitive Behavioral Therapy for Insomnia (CBT-I)
Cognitive Behavioral Therapy for Insomnia (CBT-I) is a highly effective treatment approach that focuses on identifying and addressing the underlying thoughts, behaviors, and emotions that contribute to insomnia. Unlike traditional therapy, CBT-I specifically targets sleep-related issues and aims to improve sleep quality without the need for medication. This therapeutic technique typically involves several components:
1. Sleep Education: CBT-I begins with a thorough understanding of normal sleep patterns and the factors that can disrupt them. This education helps individuals identify misconceptions about sleep and set realistic expectations for their sleep patterns.
2. Sleep Restriction: This component involves establishing a consistent sleep schedule by limiting the time spent in bed to the actual amount of time a person is able to sleep. By creating a sleep window that matches their individual sleep needs, individuals develop a stronger association between their bed and sleep.
3. Stimulus Control: This technique involves creating an optimal sleep environment that promotes relaxation and sleep. It includes recommendations such as maintaining a quiet and comfortable bedroom, avoiding stimulating activities in bed, and using the bed only for sleep and intimacy.
4. Cognitive Restructuring: This aspect of CBT-I focuses on identifying and challenging negative thoughts and beliefs about sleep. By replacing negative thoughts with more positive and realistic ones, individuals can reduce anxiety and cultivate a more positive mindset about sleep.
5. Relaxation Techniques: CBT-I often incorporates relaxation exercises like deep breathing, progressive muscle relaxation, and mindfulness meditation. These techniques help individuals manage stress and promote a calm state of mind before bedtime.
CBT-I is typically conducted over several sessions with a trained therapist, although self-help resources and online programs are also available. Combining CBT-I with other treatment approaches, such as medication or lifestyle modifications, may further enhance its effectiveness in managing insomnia and improving sleep quality. CBT-I provides individuals with practical tools and strategies to address the underlying causes of insomnia and achieve long-lasting improvements in their sleep patterns.
2. Medications for Insomnia and Depression
When it comes to treating both insomnia and depression, medication can be a valuable tool in managing symptoms. There are various types of medications that are commonly prescribed for these conditions. For insomnia, doctors may recommend the use of sedative-hypnotics, which help promote sleep by slowing down brain activity. These medications, such as benzodiazepines and non-benzodiazepines, can help individuals fall asleep faster and stay asleep throughout the night. However, they should be used with caution as they can lead to dependency and may have potential side effects. Another option for treating insomnia is using melatonin supplements, which can help regulate the sleep-wake cycle. Melatonin is a hormone that is naturally produced by the body to signal the onset of sleep. Taking melatonin supplements can help individuals fall asleep more easily and improve overall sleep quality.
In terms of depression, there are different classes of antidepressant medications that may be prescribed. Selective serotonin reuptake inhibitors (SSRIs) are among the most commonly prescribed antidepressants. They work by increasing the levels of serotonin, a neurotransmitter that is associated with mood regulation, in the brain. Other types of antidepressants include serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), and monoamine oxidase inhibitors (MAOIs). Each class of medication works on different neurotransmitters in the brain to alleviate symptoms of depression. It’s important to note that medication is not a one-size-fits-all solution, and finding the right medication and dosage may require some trial and error. Consulting with a healthcare professional who can properly assess and diagnose the individual’s condition is crucial in determining the most appropriate medication regimen. Additionally, medication is often used in conjunction with other treatment approaches, such as therapy or lifestyle modifications, to provide a comprehensive and holistic approach to managing insomnia and depression.
Conclusion
In conclusion, the link between insomnia and depression is complex and multifaceted. Insomnia can contribute to the development and severity of depression, while depression can worsen sleep disturbances. The bidirectional relationship between these two conditions highlights the importance of addressing both simultaneously in treatment plans. It is crucial for healthcare professionals to recognize and address insomnia as a potential risk factor for depression, and vice versa. Cognitive Behavioral Therapy for Insomnia (CBT-I) has shown promising results in improving sleep patterns and reducing symptoms of depression. Medications may also be prescribed to target both insomnia and depression. However, it is essential to approach treatment holistically, addressing underlying causes, lifestyle factors, and promoting healthy sleep habits. Future research and advancements in understanding this intricate link will help enhance prevention and management strategies, bringing relief to individuals battling the detrimental effects of insomnia and depression. By recognizing and addressing the connection between these two conditions, we can pave the way for improved sleep, better mental health, and enhanced overall well-being.
Frequently Asked Questions
1. Can insomnia be caused by stress?
Yes, stress is a common cause of insomnia. When we experience high levels of stress, it can be difficult to relax and quiet our minds, making it harder to fall asleep and stay asleep.
2. Does insomnia affect both sleep quality and quantity?
Yes, insomnia can impact both the quality and quantity of sleep. People with insomnia often experience difficulty falling asleep, waking up frequently during the night, or waking up too early and not being able to go back to sleep.
3. Can insomnia be a symptom of an underlying medical condition?
Yes, insomnia can sometimes be a symptom of an underlying medical condition, such as anxiety, depression, sleep apnea, or chronic pain. It is important to consult with a healthcare professional to determine the underlying cause and receive appropriate treatment.
4. Does insomnia only affect adults?
No, insomnia can affect individuals of all ages, including children and teenagers. However, the underlying causes and treatment approaches may vary depending on the age group.
5. Can certain medications contribute to the development of insomnia?
Yes, certain medications, such as antidepressants, stimulants, and medications for asthma or allergies, can interfere with sleep and contribute to the development of insomnia. If you suspect your medication is causing insomnia, consult with your healthcare provider for possible alternatives.
6. Does alcohol consumption affect sleep and contribute to insomnia?
Yes, while alcohol may initially make you feel drowsy, it can disrupt the normal sleep cycle and lead to fragmented and poor-quality sleep. Regular alcohol consumption can contribute to the development of insomnia.
7. Is it possible to overcome insomnia without medication?
Yes, it is possible to overcome insomnia without medication. Cognitive Behavioral Therapy for Insomnia (CBT-I) is a highly effective non-medication approach that focuses on changing thoughts and behaviors that contribute to sleep difficulties.
8. Can insomnia be a result of poor sleep habits?
Yes, poor sleep habits, such as irregular sleep schedules, excessive napping during the day, or engaging in stimulating activities close to bedtime, can contribute to the development of insomnia. Establishing a consistent sleep routine can help improve sleep quality.
9. Is chronic insomnia a serious condition?
Yes, chronic insomnia is considered a serious condition as it can significantly impact physical and mental health. It can lead to daytime fatigue, difficulty concentrating, mood disturbances, and an increased risk of developing other medical conditions.
10. Can insomnia be cured?
While insomnia can be challenging to overcome completely, it can be effectively managed and improved with the right treatment approaches. Identifying and addressing the underlying causes, adopting healthy sleep habits, and utilizing appropriate therapies can help individuals experience better sleep quality and reduce the impact of insomnia on their daily lives.