If you’re a parent struggling with the challenge of bedwetting in your child, you’re not alone. Many children go through this phase, and addressing it can feel overwhelming. But fear not! This comprehensive guide is here to provide practical tips and solutions to help you and your child overcome bedwetting and achieve dry nights. From understanding the causes of bedwetting to creating a supportive environment and exploring practical strategies, this article will guide you step-by-step towards finding a solution that works for your family. So let’s dive in and empower you with the knowledge and tools you need to address bedwetting effectively.
Understanding Bedwetting

Bedwetting, also known as nocturnal enuresis, is a common condition in which a child involuntarily urinates during their sleep. It is important to note that bedwetting is not a deliberate act of defiance or laziness on the part of the child. Instead, it is considered a developmental issue that most children outgrow over time. Bedwetting can be an embarrassing and frustrating experience for both the child and their parents, but it is essential to approach it with empathy and understanding.
There are several factors that can contribute to bedwetting in children. One common cause is delayed maturation of the bladder, where the bladder is not yet able to hold urine for an extended period during sleep. This can be a result of the child’s physiology or hereditary factors. Another common cause is deep sleep patterns, where the child fails to wake up when their bladder is full.
Additionally, emotional stress, such as adjusting to a new school or family situation, can also trigger bedwetting in some children. Teenagers may experience bedwetting due to hormonal changes or emotional factors. Understanding these potential causes can help parents and caregivers approach the issue of bedwetting with patience and compassion.
Impact of Diet and Fluid Intake
While it is a common belief that certain foods or beverages directly cause bedwetting, there is limited scientific evidence to support this claim. However, it is generally recommended to avoid caffeinated beverages and large fluid intakes before bedtime. Caffeine acts as a diuretic, increasing urine production, and consuming excessive fluids close to bedtime can overload the bladder, contributing to bedwetting episodes. However, it is important to ensure that the child remains adequately hydrated throughout the day by encouraging regular fluid intake.
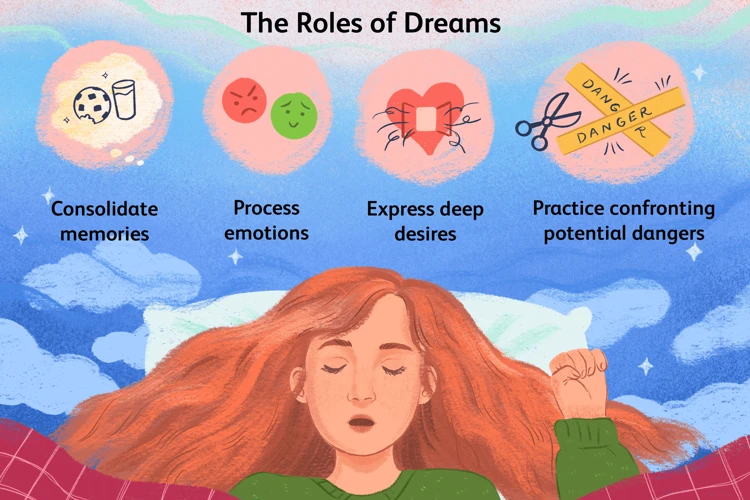
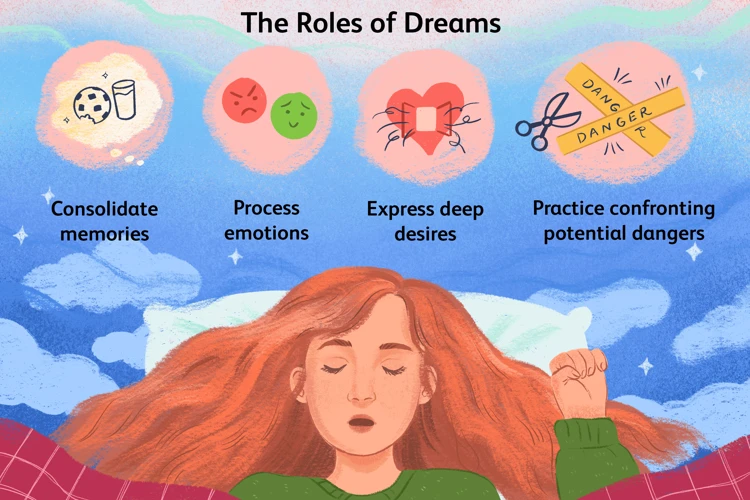
Link between Bedwetting and Dreams
Some studies suggest a potential link between bedwetting and dreams. It is believed that the brain’s failure to distinguish between dreams and reality during sleep can contribute to bedwetting episodes in some children. However, more research is needed to fully understand this connection. If you want to learn more about the potential link between dreams and bedwetting, you can read our article on dreams and bedwetting.
Being aware of the causes and factors contributing to bedwetting is the first step towards addressing this issue effectively. The next section will focus on how to talk to your child and create a supportive environment to help them overcome bedwetting with confidence.
What is Bedwetting?
Bedwetting, also known as nocturnal enuresis, refers to the involuntary release of urine during sleep in children who are old enough to control their bladder during the day. It is considered a common developmental issue that affects many children. Bedwetting can occur at any age but is more prevalent in younger children.
It is important to understand that bedwetting is not within the child’s control and should not be seen as intentional or a sign of laziness. Most children will naturally outgrow bedwetting as they mature physically and develop better bladder control. However, it can still be a source of embarrassment and distress for both the child and their parents.
There are two main types of bedwetting: primary and secondary. Primary bedwetting refers to when a child has never achieved consistent nighttime dryness, while secondary bedwetting occurs when a child begins to wet the bed after a period of being consistently dry at night.
Primary bedwetting is the most common type and is typically related to developmental factors such as a small bladder capacity or delayed maturation of bladder control. Secondary bedwetting, on the other hand, can be triggered by various factors such as emotional stress, urinary tract infections, constipation, or medical conditions that affect the urinary system. If your child has been consistently dry at night and suddenly starts bedwetting again, it is recommended to consult a healthcare professional to rule out any underlying medical causes.
Understanding the nature of bedwetting and its different forms is crucial in developing an appropriate approach to address the issue. In the next section, we will discuss the common causes of bedwetting in children and how they can impact nighttime dryness. If you’re curious about the potential connection between diet and bedwetting, you can read more in our article on foods and bedwetting.
Common Causes of Bedwetting
When it comes to bedwetting, there are several common causes that can contribute to this issue. Understanding these causes can help parents and caregivers better support their child through this phase. Here are some of the common causes of bedwetting:
1. Delayed Bladder Development: Some children may experience delayed maturation of the bladder, where the bladder is not yet able to hold urine for an extended period during sleep. This can be a result of the child’s physiology or hereditary factors.
2. Deep Sleep Patterns: Children who have deep sleep patterns may fail to awaken when their bladder is full, leading to bedwetting. These deep sleep patterns can be a normal part of a child’s sleep cycle or may be influenced by factors such as fatigue or certain medications.
3. Emotional Factors: Emotional stressors such as anxiety, fear, or undergoing significant life changes (e.g., starting a new school, moving houses) can contribute to bedwetting in some children. Emotional struggles can disrupt the normal sleep pattern, making it difficult for the child to recognize a full bladder.
4. Hormonal Imbalance: Some children may experience a hormonal imbalance that affects the body’s production of an antidiuretic hormone called vasopressin. This hormone helps regulate urine production, and a deficiency may lead to increased urine production during the night.
5. Constipation: Chronic constipation can put pressure on the bladder, leading to an increased risk of bedwetting. Encouraging a healthy and regular bowel movement can help alleviate this issue.
It’s important to remember that bedwetting is often a temporary phase that many children outgrow as they develop. However, if bedwetting persists or causes significant distress, it may be beneficial to seek medical advice. The next section will delve into how to approach the conversation with your child and create a supportive environment to help them overcome bedwetting.
Talking to Your Child

When addressing the issue of bedwetting with your child, it’s essential to approach the conversation with sensitivity and understanding. Here are some tips to consider:
- Choose the right time and place: Find a calm and private setting where your child feels comfortable discussing sensitive topics.
- Use age-appropriate language: Explain bedwetting in a way that your child can understand. Avoid using negative or accusatory language that may make them feel ashamed or guilty.
- Show empathy: Let your child know that bedwetting is a common issue that many children experience. Reassure them that it’s not their fault.
- Encourage open communication: Create an environment where your child feels safe to share their feelings, concerns, and experiences related to bedwetting.
It’s crucial to approach the topic of bedwetting with sensitivity and understanding. Here are a few key points to keep in mind:
- Avoid punishments or negative reinforcement: Bedwetting is not something your child can control, so it’s important not to blame or punish them for it.
- Provide emotional support: Let your child know that you are there to support them and that bedwetting does not impact your love or opinion of them.
- Normalize the experience: Share stories of others who have overcome bedwetting or talk about well-known figures who also experienced bedwetting as children.
- Involve your child in the solution: Encourage your child to actively participate in finding solutions and remind them that bedwetting is a temporary issue that can be managed.
By approaching the conversation about bedwetting with empathy and understanding, you can help your child feel comfortable discussing their experiences and open up opportunities for finding effective solutions together. The next section will focus on creating a supportive environment to address bedwetting.
Approaching the Conversation
Approaching the conversation about bedwetting with your child requires sensitivity and understanding. Here are some practical tips to help you navigate this discussion:
1. Choose the right time and place: Find a quiet and comfortable setting where you can have a private conversation with your child. Avoid discussing the topic in front of other family members or during a stressful moment.
2. Use age-appropriate language: Tailor your language to your child’s age and level of understanding. Explain bedwetting in a simple and gentle manner, emphasizing that it is a common issue that many children experience.
3. Share your own experiences: If you or someone in the family experienced bedwetting as a child, it can be helpful to share your own story. This can reassure your child and let them know that they are not alone.
4. Focus on empathy and reassurance: Let your child know that bedwetting is not their fault and that you understand how it may make them feel. Reassure them that you are there to support and help them overcome this challenge.
5. Encourage open communication: Let your child know that they can come to you with any concerns or questions about bedwetting. Emphasize that you are a team working together to find a solution.
6. Acknowledge emotions: Validate any emotions your child may be experiencing, such as embarrassment or frustration. Assure them that it is normal to feel this way but that you are there to support them.
7. Set realistic expectations: Explain that it may take time to overcome bedwetting and that setbacks can happen. Encourage them to stay positive and remind them of their progress along the way.
Remember, every child is unique, and their reaction to the conversation may vary. Be patient, understanding, and ready to adapt your approach to meet your child’s needs. The next section will focus on creating a supportive environment at home to help your child manage bedwetting successfully.
Sensitivity and Understanding
When it comes to addressing bedwetting, approaching the topic with sensitivity and understanding is crucial. Bedwetting can be a sensitive issue for children, as they may feel embarrassed or ashamed. To create a supportive environment, consider the following strategies:
1. Show empathy and reassurance: Let your child know that bedwetting is a common issue that many children experience and that it is not their fault. Reassure them that they are not alone and that you are there to support them throughout the process.
2. Open up communication: Encourage your child to share their feelings and concerns about bedwetting. Create a safe space where they feel comfortable discussing their experiences. Listen actively and validate their emotions, making sure they know they can confide in you without judgment.
3. Avoid blame or punishment: It is essential not to blame or shame your child for bedwetting incidents. Punishment can create anxiety and make the issue worse. Instead, focus on positive reinforcement and motivation.
4. Highlight achievements: Celebrate small victories and progress. If your child has a dry night or shows improvements in managing bedwetting, acknowledge and praise their efforts. This positive reinforcement can boost their confidence and encourage them along the way.
5. Involve the child in problem-solving: Empower your child by involving them in finding solutions. Discuss different strategies together and let them have a say in implementing those strategies. This involvement will give them a sense of control and ownership over their progress.
Remember that each child is unique, and their emotional response to bedwetting may vary. Tailor your approach based on your child’s personality and needs. By showing sensitivity and understanding, you can build a strong foundation of support and trust, helping your child navigate their bedwetting journey with confidence and resilience.
In the next section, we will explore practical tips for creating a supportive environment and implementing strategies to address bedwetting effectively.
Creating a Supportive Environment
Creating a supportive environment is crucial when addressing bedwetting in children. By establishing a consistent routine and providing emotional support, parents can help their child feel more confident and secure. Here are some practical strategies to create a supportive environment:
Implementing a structured bedtime routine can help establish a sense of stability and predictability for the child. This routine should include activities such as brushing teeth, using the bathroom before bed, and reading a bedtime story. Consistency is key, as it helps the child’s body and mind prepare for sleep. Try to create a calm and relaxing environment in the child’s bedroom, with dim lighting and minimal distractions.
Reassure your child that bedwetting is a common issue and that they are not alone. Express empathy and understanding, emphasizing that bedwetting is a temporary phase that can be overcome. Avoid negative comments or punishments, as they can negatively impact the child’s self-esteem. Instead, focus on encouraging and praising their efforts, especially when they have dry nights.
While it’s important to ensure that the child remains hydrated throughout the day, it’s advisable to limit their fluid intake in the evening, especially closer to bedtime. Encourage them to drink plenty of fluids earlier in the day and then gradually reduce the amount as bedtime approaches. This can help minimize the volume of urine produced during the night and reduce the likelihood of bedwetting episodes.
Involving the Child in the Process
Empower your child by involving them in the process of overcoming bedwetting. Encourage them to participate in activities such as tracking dry nights on a calendar or helping choose special bedding or pajamas that make them feel confident. This involvement can instill a sense of ownership and motivation to actively work towards dry nights.
By implementing these strategies, parents can create a supportive and understanding environment that promotes a positive mindset in their child. The next section will explore practical solutions and strategies that can complement the supportive environment and aid in overcoming bedwetting.
Bedtime Routine and Structure
Creating a consistent bedtime routine and structure is crucial when addressing bedwetting in children. Having a predictable routine helps signal to the child’s body that it is time for sleep and can potentially improve bladder control during the night.
Establish a Regular Bedtime: Set a consistent bedtime for your child and stick to it as much as possible. This helps regulate their sleep patterns and can contribute to better bladder control. Ensure that the bedtime is age-appropriate and allows for sufficient sleep duration.
Create a Calm and Relaxing Environment: Make the bedroom a soothing and comfortable space for your child. Dim the lights, use soft colors, and remove any distractions that may interfere with their sleep. A calm environment can promote relaxation and help your child fall asleep more easily.
Encourage Bathroom Breaks: Encourage your child to empty their bladder before bedtime. This can help reduce the amount of urine in their bladder and potentially minimize the chance of bedwetting during the night. Make it a part of their bedtime routine.
Limit Fluid Intake Before Bed: It is important to strike a balance between adequate hydration and limiting fluid intake before bedtime. Encourage your child to drink enough fluids throughout the day, but start gradually reducing their intake in the evening. Avoid giving them large amounts of fluids close to bedtime to lessen the chances of bedwetting.
Implement a Bedwetting Alarm: Bedwetting alarms can be a helpful tool in promoting bladder control. These devices are designed to detect moisture and trigger an alarm to wake the child up as soon as bedwetting occurs. This can help train their bladder to recognize the sensation of a full bladder and eventually reduce or eliminate bedwetting episodes.
By implementing a consistent bedtime routine and structure, you can help regulate your child’s sleep patterns and potentially improve their bladder control. The next section will discuss the importance of encouragement and reassurance in addressing bedwetting and creating a supportive environment for your child.
Encouragement and Reassurance
Encouragement and reassurance play a crucial role in supporting a child who is experiencing bedwetting. It is important for parents and caregivers to maintain a positive and understanding attitude throughout the process. Here are some practical tips for providing encouragement and reassurance:
1. Open Communication: Create an open and honest environment where your child feels comfortable discussing their bedwetting. Encourage them to share their thoughts and feelings without fear of judgment or criticism. Let them know that bedwetting is a common issue and that they are not alone.
2. Praise Progress: Celebrate small victories and acknowledge any progress made towards dry nights. Offer praise and rewards when your child has a dry night or shows effort in managing their bedwetting. This positive reinforcement can boost their confidence and motivation.
3. Emphasize It’s Not Their Fault: Reassure your child that bedwetting is not their fault. Remind them that it is a normal part of growing up and that it will eventually resolve itself. Help them understand that their worth is not determined by their ability to stay dry.
4. Manage Frustration: It is natural for both children and parents to feel frustrated or disappointed about bedwetting incidents. However, it is crucial to avoid expressing anger or blame towards the child. Instead, remain patient and understanding, providing comfort and support.
5. Normalize Bedwetting: Talk to your child about how many other children go through the same experience. Share stories or experiences of family members or friends who have overcome bedwetting to inspire hope and alleviate any feelings of embarrassment or isolation.
6. Offer Reassurance: Reassure your child that bedwetting is temporary and that they will eventually outgrow it. Let them know that you are there to support them every step of the way. Remind them of their other achievements and talents to boost their self-esteem.
Remember, providing encouragement and reassurance is an ongoing process. It may take time for your child to feel confident and secure, so be patient and understanding. The next section will explore practical solutions and strategies to help manage bedwetting effectively.
Limiting Fluid Intake Before Bed
When addressing bedwetting in children, it is essential to consider limiting fluid intake before bed as an effective strategy. While it is important for children to stay hydrated throughout the day, managing their fluid intake closer to bedtime can help reduce the likelihood of bedwetting episodes. Here are some practical tips to implement this approach:
- Establish a routine: Create a consistent bedtime routine that includes going to the bathroom before getting into bed. This helps empty the bladder and reduces the chances of needing to urinate during the night.
- Encourage daytime fluid intake: Make sure your child consumes an adequate amount of fluids throughout the day to maintain hydration. This way, they won’t feel overly thirsty before bedtime, which may lead to excessive fluid intake.
- Timing is key: Limit the consumption of fluids, especially those containing caffeine or artificial sweeteners, in the hours leading up to bedtime. It is advisable to avoid these types of beverages altogether, as they can act as diuretics, increasing urine production.
- Offer a final drink: If your child feels thirsty before bed, offer a small drink of water rather than a large quantity. This allows them to quench their thirst without overloading the bladder.
- Encourage bathroom breaks: Remind your child to use the bathroom one last time before getting into bed. This helps ensure their bladder is as empty as possible before sleep.
Implementing these strategies can help reduce the frequency of bedwetting episodes by managing fluid intake in a practical manner. However, it is important to note that every child is unique, and what works for one child may not work for another. The next section will explore additional practical solutions and strategies, such as bedwetting alarms and protective bedding, to further support your efforts in addressing bedwetting effectively.
Practical Solutions and Strategies
When it comes to addressing bedwetting in children, there are various practical solutions and strategies that can be implemented to help manage and eventually overcome the issue.
Bedwetting alarms are devices that can be placed on the child’s undergarments or on the bed itself. These alarms are designed to detect moisture and sound an alarm, waking the child up as soon as they begin to wet the bed. Over time, this helps to condition the child to wake up and use the toilet when their bladder is full, eventually training their body to achieve dry nights. Bedwetting alarms have proven to be an effective intervention for many children.
Investing in protective bedding and mattress covers can go a long way in managing bedwetting incidents. Waterproof mattress covers create a barrier between the child and the mattress, protecting it from moisture and potential damage. It is advisable to have multiple sets of bedding on hand for quick and easy changes during the night to minimize disruptions and discomfort for the child.
Reinforcing good toilet training techniques during the day can also support nighttime bladder control. Encourage your child to use the toilet regularly throughout the day and establish a routine. Encourage them to empty their bladder before bedtime and ensure they have ample time to do so. Additionally, providing positive reinforcement, such as praise or small rewards, for successful trips to the bathroom can motivate and empower your child in their journey to achieving dry nights.
Creating a Bedwetting Diary
Keeping a bedwetting diary can be a helpful strategy to understand patterns and triggers associated with bedwetting incidents. In the diary, record information such as fluid intake, bedtime routines, and any stressful events throughout the day. This can assist in identifying potential triggers and tailoring strategies to address them more effectively.
Using Absorbent Underwear
Absorbent underwear provides an added layer of protection during the night, helping to minimize the discomfort and embarrassment associated with bedwetting episodes. These specially designed undergarments can absorb large amounts of urine, keeping the child dry and comfortable throughout the night. Using absorbent underwear can boost your child’s confidence and reduce anxiety related to bedwetting.
By implementing these practical solutions and strategies, you can provide your child with the necessary tools and support to manage bedwetting effectively. However, it is important to keep in mind that each child is unique, and what works for one may not work for another. Stay patient, supportive, and open to trying different approaches until you find what best suits your child’s needs.
Bedwetting Alarms
Bedwetting alarms are devices designed to alert both the child and their parents when the child starts to wet the bed. These alarms can be highly effective in helping children become more aware of their bladder sensations and develop the ability to wake up and use the bathroom independently.
How do bedwetting alarms work? Typically, these alarms consist of a moisture sensor that is placed in the child’s underwear or on a special bed pad. When the sensor detects urine, it triggers an alarm, which can be auditory, vibratory, or a combination of both. The alarm wakes up the child, allowing them to stop urinating and finish in the bathroom.
Using bedwetting alarms requires consistency and commitment. Here are some key points to consider when using these devices:
- Choose the right alarm: There are various types of bedwetting alarms available in the market. Consider factors such as comfort, ease of use, and alarm type preference (auditory, vibratory, or both) when selecting the right one for your child.
- Introduce the alarm gradually: Help your child become familiar with the alarm by letting them practice wearing it during the day before using it at night. This can help reduce any anxiety or resistance they may have.
- Establish a routine: Set a consistent time each night to use the bedwetting alarm. This reinforces the idea that using the alarm is part of their bedtime routine and helps create a sense of structure.
- Involve your child in the process: Encourage your child to take an active role in using the alarm. Let them assist in attaching the sensor to their underwear or bed pad and involve them in the process of resetting and cleaning the alarm after each use.
- Track progress and offer rewards: Keep a record of dry nights and provide positive reinforcement for each successful night. This can include verbal praise, small treats, or a reward system to motivate your child and build their confidence.
- Be patient: It takes time for children to respond to bedwetting alarms. Consistency, patience, and encouragement are key throughout the process. Remember that progress may be gradual, but most children eventually achieve dry nights with the help of alarms.
Bedwetting alarms can be an effective tool in helping your child overcome bedwetting. However, it is important to note that they may not work for every child. If you’re unsure about using bedwetting alarms or if your child is not responding to this method, it may be beneficial to seek professional guidance or explore other practical solutions and strategies.
Protective Bedding and Mattress Covers
When it comes to managing bedwetting, having protective bedding and mattress covers can make a significant difference in maintaining cleanliness and preventing damage to the mattress. Here are some options and considerations to keep in mind:
1. Waterproof Mattress Protectors: Investing in a waterproof mattress protector is essential. These protectors create a barrier between the mattress and any moisture, preventing it from seeping through and causing stains or odors. Look for a mattress protector that is specifically designed for bedwetting and has a soft, breathable fabric to ensure comfort.
2. Waterproof Fitted Sheets: In addition to a mattress protector, you can also consider using waterproof fitted sheets. These sheets have a waterproof layer built into them, providing an extra layer of protection against any accidental bedwetting. They are easy to clean and can be swapped out when needed while keeping the mattress underneath safe and dry.
3. Absorbent Bed Pads: Bed pads are another useful tool to have. These pads are placed on top of the fitted sheet and provide an additional layer of absorbency. They are particularly helpful during the transition period when the child is working towards achieving dry nights. Bed pads can quickly absorb any urine and prevent it from reaching the mattress.
4. Layering with Multiple Bedding: One effective strategy is to layer the bedding to minimize disruptions during the night. Start with a waterproof mattress protector, followed by a fitted sheet, and then another layer of waterproof sheet or a bed pad. This way, if there is an accident during the night, you can easily remove the top layer and have a clean layer ready for your child to go back to sleep quickly.
5. Quick and Easy Cleaning: It is essential to choose bedding and mattress covers that are machine washable for quick and easy cleaning. Look for products labeled as machine washable and follow the instructions provided. This will make the cleanup process much more convenient for both you and your child.
By incorporating these protective bedding options and mattress covers into your child’s bed, you can effectively manage bedwetting and minimize the stress associated with nighttime accidents. The next section will explore techniques for introducing toilet training and helping your child develop healthy bladder habits.
Introducing Toilet Training Techniques
When it comes to addressing bedwetting in children, one effective approach is to introduce toilet training techniques. While some children may have already undergone toilet training during their toddler years, revisiting these techniques can be helpful in managing bedwetting. Here are some practical strategies to consider:
1. Establish a Regular Toilet Routine: Encourage your child to use the bathroom before bedtime and as soon as they wake up in the morning. Creating a consistent routine helps train their bladder to empty at specific times.
2. Encourage Fluid Intake During the Day: Ensure that your child drinks an adequate amount of fluids during the day. This helps strengthen their bladder muscles and can reduce the tendency to produce excessive urine at night.
3. Use a Bedwetting Alarm: Bedwetting alarms are devices that detect moisture and release a sound or vibration to wake the child when they start to wet the bed. These alarms can be effective in conditioning the child to wake up when their bladder is full, eventually leading to dry nights.
4. Implement a Reward System: Positive reinforcement can play a significant role in motivating your child during their toilet training journey. Consider using a reward system where they receive small incentives or praise for dry nights.
5. Monitor Liquid Intake Before Bedtime: Limiting your child’s fluid intake in the evening, especially within a couple of hours before bedtime, can help reduce the volume of urine produced and lessen the chances of bedwetting.
6. Encourage Self-Help Strategies: Teach your child strategies to help manage bedwetting independently. For example, they can practice waking themselves up to use the bathroom or changing their sheets if an accident occurs.
7. Use Protective Bedding: Investing in waterproof mattress covers and absorbent bed pads can minimize the impact of bedwetting accidents on the mattress and sheets, making cleanup easier and more manageable.
It is important to remember that each child is unique, and what works for one may not work for another. Be patient, understanding, and supportive throughout the toilet training process. Celebrate small victories and reassure your child that bedwetting is a common issue that can be overcome with time and practice. With consistency and the right techniques, you can help your child gradually achieve dry nights and gain confidence in managing bedwetting.
Seeking Professional Guidance
In some cases, bedwetting may persist despite implementing various strategies at home. If you find that your child’s bedwetting continues or if it is causing significant distress for your child, it may be time to seek professional guidance. Consulting a pediatrician is recommended to rule out any underlying medical conditions that could be contributing to the bedwetting. The pediatrician will evaluate your child’s overall health and may conduct tests to identify any physiological factors that need to be addressed. They can provide expert advice tailored to your child’s specific situation, offer reassurance, and help you develop a customized plan to address the bedwetting.
In some cases, additional interventions may be necessary to overcome bedwetting. Your pediatrician may recommend specialized therapies or treatments based on your child’s individual needs. These may include:
1. Behavioral Therapy: Behavioral therapy techniques, such as bladder training and moisture alarms, can help your child develop better control over their bladder and recognize the sensations of a full bladder during sleep.
2. Medications: In certain situations, medications may be prescribed to help reduce nighttime urine production or increase bladder capacity. These medications should only be used under the guidance and supervision of a healthcare professional.
3. Psychological Support: If emotional factors are contributing to the bedwetting, your pediatrician may recommend counseling or therapy to address any underlying issues and provide emotional support to your child.
Remember, seeking professional guidance does not mean you have failed or that your child’s bedwetting is abnormal. It simply means you are taking an extra step to ensure the well-being of your child and explore all available options to address the bedwetting effectively.
By working together with a pediatrician and potentially exploring specialized therapies or treatments, you can gain the support and expertise needed to assist your child in overcoming bedwetting and promoting healthy sleep patterns.
As we conclude this article, let’s summarize the key points discussed and provide a sense of closure.
Consulting a Pediatrician
When it comes to dealing with bedwetting, consulting a pediatrician can be a valuable step in understanding and addressing the issue. A pediatrician is a medical professional who specializes in the health and well-being of children. They have the expertise to evaluate your child’s specific situation and provide guidance and support tailored to their needs.
During a consultation with a pediatrician, they will typically start by taking a detailed medical history and asking specific questions about your child’s bedwetting patterns and any underlying factors that may contribute to it. This initial assessment helps the pediatrician determine the best course of action to address the bedwetting.
Physical examination: In some cases, a physical examination may be conducted to assess for any underlying medical conditions that could be contributing to the bedwetting. This examination may include checking the child’s abdomen and genitals for any abnormalities.
Urinalysis: A urinalysis, which involves analyzing a urine sample, may be requested by the pediatrician. This helps rule out any signs of infection, diabetes, or other related conditions that could be causing or worsening the bedwetting.
Behavioral and lifestyle assessment: The pediatrician will likely delve into different aspects of the child’s life, such as their daily routines, sleep patterns, and emotional well-being. Understanding these factors can help identify any behavioral or lifestyle modifications that may aid in managing bedwetting.
Based on the assessment findings, the pediatrician may recommend specific interventions or treatments tailored to your child’s needs. These may include:
1. Bedwetting alarms: These alarms can be effective in conditioning the child to wake up when their bladder is full. They consist of a moisture sensor that alerts the child with an alarm or vibration to prompt them to go to the bathroom.
2. Medications: In some cases, the pediatrician may prescribe medications to help reduce the frequency of bedwetting episodes. These medications work by either decreasing urine production or increasing bladder capacity.
3. Behavioral therapy: The pediatrician may recommend specific behavioral techniques, such as bladder training exercises or implementing a reward system, to help motivate and encourage the child towards dry nights.
4. Referrals to specialists: In more complex cases or when underlying medical conditions are suspected, the pediatrician may refer your child to a specialist, such as a urologist or a psychologist, for further evaluation and treatment.
Remember, consulting a pediatrician is an important step in addressing bedwetting, as they can provide professional guidance, rule out underlying medical conditions, and recommend appropriate interventions. Working closely with your child’s healthcare provider can significantly improve the chances of success in managing bedwetting and supporting your child on their journey towards dry nights.
Specialized Therapies and Treatments
Specialized therapies and treatments can be effective in addressing bedwetting in children when other approaches have not been successful. Here are some options to consider:
1. Behavioral Therapy: Behavioral therapy aims to modify specific behaviors and habits associated with bedwetting. One common technique is bladder training, where the child is encouraged to gradually increase the duration between bathroom visits during the day. This helps improve bladder capacity and control. Another approach is moisture alarms, which consist of a sensor that detects urine and triggers an alarm to wake the child when wetting occurs. Over time, this can help condition the child to recognize the sensation of a full bladder and wake up to use the toilet.
2. Medications: In some cases, healthcare professionals may recommend medication to manage bedwetting. Desmopressin is a synthetic hormone that reduces urine production and can be taken orally or via nasal spray. This medication is usually used for short periods or during specific situations, such as sleepovers or vacations. It is important to note that medication should be used under the guidance of a healthcare professional and is not a long-term solution.
3. Alternative Therapies: Some alternative therapies, such as acupuncture or hypnosis, have been suggested as potential treatments for bedwetting. However, their effectiveness is still under investigation, and more research is needed to determine their true efficacy.
4. Psychological Support: Bedwetting can have a significant emotional impact on a child, leading to embarrassment, anxiety, and low self-esteem. In such cases, seeking psychological support from a therapist or counselor can help the child cope with these feelings and develop strategies to manage the emotional aspects of bedwetting.
It is important to remember that each child is unique, and what works for one may not work for another. Specialized therapies and treatments should always be approached in consultation with a healthcare professional experienced in treating bedwetting. They can help evaluate the underlying causes of bedwetting, assess the child’s individual circumstances and recommend appropriate treatment options.
By exploring specialized therapies and treatments, parents can find additional tools to support their child in overcoming bedwetting and achieving dry nights. However, it is crucial to approach these options with realistic expectations and a focus on the individual needs of the child.
Conclusion
In conclusion, bedwetting is a common condition that many children experience, and it’s important for parents and caregivers to approach it with understanding and patience. Understanding the causes of bedwetting, such as delayed bladder maturation, deep sleep patterns, and emotional stress, can help us create a supportive environment for our children. By establishing a consistent bedtime routine, offering encouragement and reassurance, and limiting fluid intake before bed, we can help reduce the frequency of bedwetting episodes. Additionally, practical solutions like bedwetting alarms, protective bedding, and introducing toilet training techniques can also be effective strategies. If bedwetting persists or causes significant distress, it’s advisable to consult a pediatrician who can provide further guidance and potentially recommend specialized therapies or treatments. Remember, every child is unique, and finding the right approach may require some trial and error. With time, patience, and support, most children overcome bedwetting and achieve dry nights.
Frequently Asked Questions
FAQs about Bedwetting
1. Is bedwetting a sign of a serious medical problem?
No, bedwetting is typically not a sign of a serious medical problem. It is often a normal part of a child’s development and most children outgrow it over time.
2. Should I wake my child up during the night to use the toilet?
Waking your child up during the night to use the toilet is not recommended, as it may disrupt their sleep pattern and can be counterproductive. It is best to focus on creating a supportive environment and implementing practical solutions to address bedwetting.
3. Is bedwetting more common in boys or girls?
Bedwetting is slightly more common in boys than girls. However, it can affect children of any gender.
4. Can stress or emotional factors contribute to bedwetting?
Yes, stress or emotional factors such as adjusting to a new school or family situation can contribute to bedwetting in some children. Creating a supportive and understanding environment can help alleviate the impact of stress on bedwetting.
5. Are there any medications that can help with bedwetting?
In some cases, a pediatrician may prescribe medications to help with bedwetting. However, they are typically considered a last resort when other strategies have been ineffective, and their use should be discussed with a healthcare professional.
6. Can my child participate in sleepovers or camps despite bedwetting?
Absolutely! It is important to encourage your child to participate in social activities, even if they experience bedwetting. Discuss the situation with the host or camp counselor beforehand, and provide any necessary protective bedding or supplies.
7. Is there a specific age when bedwetting should stop?
There is no specific age when bedwetting should stop, as it varies from child to child. However, most children outgrow bedwetting by the age of 7. If bedwetting continues beyond this age or causes significant distress, consulting a healthcare professional is recommended.
8. Can bedwetting be genetic?
There is evidence to suggest that bedwetting can have a genetic component. If one or both parents experienced bedwetting as children, the chances of their own children experiencing it are increased.
9. Are there any natural remedies or alternative therapies for bedwetting?
While there are no proven natural remedies to cure bedwetting, some parents have reported success with methods such as herbal supplements or acupuncture. It is essential to consult with a healthcare professional before considering any alternative therapies.
10. How long should I wait before seeking professional help for bedwetting?
If your child is over the age of 7 and is still experiencing bedwetting or if it is causing significant distress, it is advisable to consult a pediatrician or healthcare professional for an evaluation and guidance.








