Did you ever find yourself waking up in the middle of the night, completely paralyzed, unable to move or speak? You may have experienced a curious phenomenon called sleep paralysis. This perplexing condition often leaves people feeling scared and confused, wondering what causes it and if it’s something to be concerned about. In this article, we will delve into the science behind sleep paralysis, exploring its various types, prevalence, and potential causes. We will also investigate the intriguing connection between sleep paralysis and hallucinations, as well as its impact on mental health. Finally, we will discuss some practical strategies for managing and preventing sleep paralysis episodes. So, join us on this journey as we unlock the secrets of sleep paralysis and gain a better understanding of this mysterious sleep disorder.
Understanding Sleep Paralysis

Sleep paralysis is a fascinating and enigmatic phenomenon that occurs during sleep, leaving individuals temporarily unable to move or speak. Sleep paralysis can be a deeply unsettling experience, often accompanied by a sense of fear and a feeling of pressure on the chest. It is important to understand the different aspects of this condition in order to demystify it and alleviate any concerns. One key aspect is knowing what sleep paralysis actually is. Another aspect is recognizing the various types of sleep paralysis that can occur, such as isolated sleep paralysis or sleep paralysis in relation to other sleep disorders. Additionally, understanding the prevalence and frequency of sleep paralysis can help individuals realize that they are not alone in experiencing this phenomenon. By exploring these aspects, we can gain a deeper understanding of sleep paralysis and how it affects those who experience it. For more information on sleep paralysis, you can visit our article on Understanding Sleep Paralysis.
What is Sleep Paralysis?
Sleep paralysis is an intriguing phenomenon that occurs during sleep and involves a temporary inability to move or speak. It is essentially a brief transitional state between sleep and wakefulness, where the body remains paralyzed even as the mind becomes alert. During this episode, individuals may be fully conscious of their surroundings, but are physically unable to respond or initiate any voluntary movements. This can be an incredibly distressing experience, as individuals may feel trapped and helpless. The duration of sleep paralysis episodes can vary, with some lasting a few seconds and others lasting several minutes. It is important to note that sleep paralysis is a natural occurrence and not considered harmful or medically concerning. However, it can cause significant distress and anxiety, especially for those who experience it frequently. To delve deeper into understanding sleep paralysis, continue reading our article here.
Types of Sleep Paralysis
When it comes to sleep paralysis, there are different types that individuals may experience. Each type presents its own unique characteristics and nuances. One type of sleep paralysis is called isolated sleep paralysis, which occurs independently of any underlying sleep disorder. It typically happens when transitioning between sleep stages, such as from Rapid Eye Movement (REM) sleep to wakefulness. Another type is sleep paralysis with narcolepsy, which is often associated with the sleep disorder narcolepsy. Narcolepsy is characterized by excessive daytime sleepiness and a tendency to suddenly fall asleep. People with narcolepsy may experience sleep paralysis episodes alongside other symptoms such as cataplexy (sudden loss of muscle tone) and vivid hallucinations. Sleep paralysis related to other sleep disorders is yet another type. Conditions like sleep apnea, insomnia, and restless legs syndrome can sometimes trigger sleep paralysis episodes. In these cases, addressing and managing the underlying sleep disorder may help alleviate sleep paralysis episodes. By understanding the different types of sleep paralysis, individuals can better identify and comprehend their own experiences. To learn more about the role of anxiety and stress in sleep paralysis, you can refer to our article on The Role of Anxiety and Stress in Sleep Paralysis.
Prevalence and Frequency
Sleep paralysis is more common than you might think. Studies have revealed that around 8% of the general population experiences sleep paralysis at least once in their lives. However, the prevalence and frequency of sleep paralysis can vary across different demographics and individuals. Research has shown that certain groups are more prone to experiencing sleep paralysis, such as those with sleep disorders like narcolepsy or sleep apnea. In these cases, the occurrence of sleep paralysis can be much higher. Stress, anxiety, and disrupted sleep patterns can also contribute to an increased likelihood of experiencing sleep paralysis. Interestingly, there have been some famous cases of sleep paralysis reported throughout history, further highlighting its presence in society and its impact on individuals. To learn more about these intriguing cases, you can visit our article on Famous Sleep Paralysis Cases. Understanding the prevalence and frequency of sleep paralysis helps us comprehend the scope of this phenomenon and its significance in the lives of those who experience it.
Causes of Sleep Paralysis

The causes of sleep paralysis are multifaceted and can involve a combination of factors related to the brain, sleep cycle, and psychological aspects. One significant aspect is the role of the brain and sleep cycle. Sleep paralysis often occurs during the transition between sleep stages, particularly during REM (Rapid Eye Movement) sleep, when dreams occur. Certain neurological factors contribute to the occurrence of sleep paralysis, such as disruptions in the normal sleep pattern or irregularities in neurotransmitters. Additionally, psychological factors can play a role in sleep paralysis, including high levels of stress, anxiety, or sleep deprivation. It is important to recognize that these factors can vary from person to person, and identifying the specific triggers for each individual may require further exploration. By understanding the causes of sleep paralysis, we can begin to develop strategies to manage and prevent its occurrence.
Brain and Sleep Cycle
The brain and sleep cycle are intricately linked when it comes to sleep paralysis. Understanding this connection is crucial in comprehending the underlying mechanisms of this phenomenon. During sleep, the brain goes through different stages, including rapid eye movement (REM) sleep and non-rapid eye movement (NREM) sleep. REM sleep is characterized by vivid dreams and increased brain activity, while NREM sleep is associated with deep, restorative sleep. Sleep paralysis typically occurs during the transition between these stages, specifically when an individual is transitioning from REM sleep to wakefulness.
During REM sleep, the brain sends signals to the spinal cord to inhibit muscle movement. This is a protective mechanism that prevents individuals from acting out their dreams and potentially causing harm to themselves or others. However, in cases of sleep paralysis, this inhibition of muscle activity continues even as an individual becomes conscious. The brain, still partially in a state of REM sleep, mistakenly keeps the body in a state of paralysis, causing the individual to be temporarily unable to move or speak.
It is important to note that the exact reasons why this transition from REM sleep to wakefulness sometimes leads to sleep paralysis are not fully understood. However, researchers believe that disruptions in the normal sequence of sleep stages and disturbances in the neurotransmitters involved in regulating sleep-wake cycles may play a role.
By unraveling the intricate connection between the brain and sleep cycle, we can begin to grasp the underlying mechanisms of sleep paralysis. This knowledge paves the way for further research and potential interventions to help individuals who experience this intriguing sleep phenomenon.
Neurological Factors
Neurological factors play a significant role in the occurrence of sleep paralysis. The complex interplay between the brain’s intricate processes and the sleep cycle contribute to this phenomenon. Let’s explore some key neurological factors:
1. Disrupted REM Sleep: Rapid Eye Movement (REM) sleep is a stage of sleep associated with vivid dreaming. During REM sleep, our brain sends signals to inhibit movement to prevent us from acting out our dreams. In individuals with sleep paralysis, there can be a disruption or fragmentation of REM sleep, leading to a mismatch between the brain’s inhibitory signals and the body’s motor function.
2. Abnormalities in the Pons: The pons, a region located in the brainstem, is responsible for regulating REM sleep and muscle atonia (temporary paralysis) during this stage. Research suggests that dysfunction or abnormalities in the pons may contribute to the occurrence of sleep paralysis.
3. Imbalanced Neurotransmitters: Neurotransmitters, such as gamma-aminobutyric acid (GABA) and serotonin, play crucial roles in regulating sleep-wake cycles and muscle activity. An imbalance or dysregulation of these neurotransmitters may disrupt the normal functioning of the brain during sleep, potentially leading to sleep paralysis.
4. Hypofrontality: Hypofrontality refers to a reduced activity in the prefrontal cortex, the part of the brain responsible for decision-making and rational thinking. Some studies propose that hypofrontality during sleep paralysis episodes may contribute to the sense of fear and hallucinations experienced during these episodes.
While these neurological factors provide insight into the mechanisms underlying sleep paralysis, it is important to note that the specific causes can vary among individuals. It is a multifaceted condition influenced by various factors, including both neurological and psychological aspects. Understanding these neurological factors is a crucial step in comprehending the science behind sleep paralysis and developing potential strategies for management and prevention.
Psychological Factors
Psychological factors play a significant role in the occurrence of sleep paralysis episodes. These factors can contribute to the frequency and intensity of experiences, as well as the overall emotional impact. Stress and anxiety are common psychological factors associated with sleep paralysis. When individuals experience high levels of stress or anxiety, it can disrupt the natural sleep cycle and increase the likelihood of sleep paralysis episodes. Additionally, post-traumatic stress disorder (PTSD) has been linked to an increased risk of sleep paralysis. Traumatic events can trigger both PTSD and sleep paralysis, creating a complex interaction between the two conditions. Individuals with underlying mental health conditions such as depression or panic disorder may be more susceptible to experiencing sleep paralysis. The presence of these psychological factors can further exacerbate the distress associated with sleep paralysis, leading to a vicious cycle of anxiety and sleep disturbances. Recognizing and addressing these psychological factors through therapy, stress management techniques, and proper sleep hygiene can help in managing sleep paralysis episodes and improving overall well-being.
Science Behind Hallucinations
Hallucinations are a fascinating aspect of sleep paralysis, often leaving individuals questioning the nature of their experiences. Understanding the science behind hallucinations can shed light on this intriguing phenomenon. One crucial element is the relationship between REM sleep and dreams. During REM sleep, the brain is highly active, and dreams can occur vividly. This can lead to a blurred boundary between the dream world and reality during sleep paralysis, giving rise to hallucinations. Exploring the concept of hypnagogic and hypnopompic hallucinations can provide insights. These hallucinations occur during the transitional states between wakefulness and sleep, further contributing to the bewildering experiences of sleep paralysis. Finally, the role of brain chemistry and the visual cortex is significant. Imbalances in neurotransmitters and heightened activity in the visual cortex can amplify hallucinatory experiences. By unraveling the science behind hallucinations, we can begin to comprehend the extraordinary nature of sleep paralysis and gain a deeper appreciation for the complex workings of the human brain.
REM Sleep and Dreams
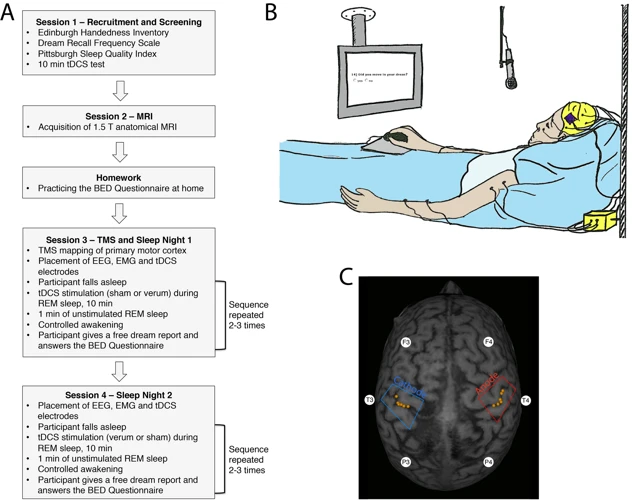
During REM (Rapid Eye Movement) sleep, fascinating things occur within the brain. REM sleep is a stage of sleep characterized by rapid eye movements, increased brain activity, and vivid dreams. It is during this stage that the brain engages in crucial processes, such as memory consolidation and emotional regulation. When it comes to sleep paralysis, REM sleep plays a significant role. During REM sleep, the brain sends signals to inhibit voluntary muscle activity, effectively preventing us from acting out our dreams and potentially harming ourselves. This temporary paralysis is known as REM atonia. However, in cases of sleep paralysis, the paralysis extends beyond the REM stage and persists into wakefulness. This means that individuals experience a disconnect between the brain’s instructions to inhibit muscle movement and the conscious desire to move. This disconnect can lead to feelings of helplessness and vulnerability. It is important to note that the vivid dreams associated with REM sleep can also influence the hallucinations often experienced during sleep paralysis. The boundary between dream and wakefulness becomes blurred, allowing dream-like images and sensations to intrude upon the waking state, resulting in hallucinations that can be frightening and disorienting. Exploring the intricate relationship between REM sleep and dreams gives us a better understanding of why sleep paralysis occurs and provides insight into the vivid and often bizarre experiences associated with this phenomenon.
Hypnagogic and Hypnopompic Hallucinations
Hypnagogic and hypnopompic hallucinations are intriguing phenomena closely associated with sleep paralysis. Hypnagogic hallucinations refer to vivid sensory experiences that occur during the transition from wakefulness to sleep. These hallucinations can take various forms, including visual, auditory, or tactile sensations. For instance, individuals may see vivid images or hear voices that are not actually present. On the other hand, hypnopompic hallucinations occur during the awakening process, as individuals transition from sleep to wakefulness. Similarly, these hallucinations can involve sensory experiences that feel incredibly real. It is not uncommon for people to report seeing shadowy figures, hearing mysterious sounds, or feeling the presence of someone or something in the room. Both hypnagogic and hypnopompic hallucinations can be intense and disorienting, adding to the already surreal experience of sleep paralysis. Researchers believe that these hallucinations may be attributed to the intrusion of dream-like imagery and sensations into wakefulness or the inability of the brain to fully transition between sleep and wakefulness. The exact mechanisms behind these hallucinations are still not fully understood, but they are thought to involve disruptions in the normal processes of the sleep-wake cycle and the brain’s perception and interpretation of sensory information. Understanding the science behind these hallucinations is crucial in unraveling the mysteries of sleep paralysis and its associated phenomena.
Brain Chemistry and Visual Cortex
The intricate workings of the brain and its chemistry play a significant role in understanding the relationship between sleep paralysis and hallucinations. When it comes to the specific topic of brain chemistry and the visual cortex, research suggests that abnormalities in neurotransmitters and neural circuits may contribute to the occurrence of hallucinations during sleep paralysis. Neurotransmitters such as serotonin and dopamine, which regulate mood and perception, have been found to be imbalanced in individuals experiencing sleep disorders. This disruption in neurotransmitter activity can impact the functioning of the visual cortex, the part of the brain responsible for processing visual information. Abnormalities in the visual cortex can lead to misinterpretations of sensory input and give rise to vivid and often terrifying hallucinations during sleep paralysis episodes. It is important to note that further investigation is needed to fully understand the intricacies of brain chemistry and the visual cortex in relation to sleep paralysis. However, these preliminary findings provide valuable insights into the fascinating connection between brain chemistry and the visual cortex in the phenomenon of sleep paralysis and its associated hallucinations.
The Role of Sleep Disorders
Sleep disorders can play a significant role in the occurrence of sleep paralysis. One such disorder is Narcolepsy, a neurological condition characterized by excessive daytime sleepiness and sudden, uncontrollable episodes of sleep. Individuals with narcolepsy often experience sleep paralysis as a symptom. Another sleep disorder that can contribute to sleep paralysis is Sleep Apnea, a condition where breathing repeatedly stops and starts during sleep, leading to fragmented sleep and disrupted REM sleep. Sleep apnea has been found to increase the risk of experiencing sleep paralysis. Additionally, other sleep disorders such as insomnia, restless legs syndrome, and sleep-related movement disorders can also be connected to sleep paralysis. Understanding the relationship between sleep disorders and sleep paralysis is crucial in comprehending the complex factors that contribute to this intriguing phenomenon. For more information on the connection between sleep disorders and sleep paralysis, you can refer to our article on The Role of Anxiety and Stress in Sleep Paralysis.
Narcolepsy and Sleep Paralysis
Narcolepsy is a neurological disorder characterized by excessive daytime sleepiness and sudden, uncontrollable episodes of falling asleep. Interestingly, narcolepsy and sleep paralysis often go hand in hand. Sleep paralysis is a common symptom experienced by many individuals with narcolepsy. During the transition between wakefulness and sleep, the brain typically prevents us from acting out our dreams by inhibiting muscle movement. However, in narcolepsy, this process becomes disrupted, leading to episodes of sleep paralysis as the individual wakes up or falls asleep. These episodes can be brief but can generate intense feelings of fear and confusion. It is important to note that not all individuals with narcolepsy experience sleep paralysis, but it is a common occurrence. By further exploring the relationship between narcolepsy and sleep paralysis, researchers hope to better understand the underlying mechanisms and develop more effective treatment strategies for both conditions. This connection highlights the intricate relationship between sleep disorders and emphasizes the need for comprehensive evaluation and management when addressing sleep-related issues. For more information on sleep paralysis and its relationship with narcolepsy, you can visit our article on Narcolepsy and Sleep Paralysis.
Sleep Apnea and Sleep Paralysis
Sleep apnea, a common sleep disorder characterized by interrupted breathing during sleep, has been found to have a strong association with sleep paralysis. The two conditions often coexist, with individuals experiencing both sleep apnea and sleep paralysis simultaneously. The relationship between sleep apnea and sleep paralysis can be attributed to several factors.
1. Disrupted Sleep: Sleep apnea disrupts the normal sleep pattern, causing frequent awakenings throughout the night. These interruptions in sleep can increase the likelihood of experiencing sleep paralysis episodes. The fragmented sleep caused by sleep apnea disrupts the sleep cycle, leading to an imbalance in REM sleep, the stage of sleep where paralysis normally occurs.
2. Oxygen Levels: In individuals with sleep apnea, the repeated cessation of breathing leads to a decrease in oxygen levels in the body. This decrease in oxygen can have an impact on brain function and potentially trigger sleep paralysis episodes. The exact mechanisms behind this relationship are still being studied but it is believed that the lack of oxygen affects the brain’s ability to regulate sleep and wakefulness.
3. Hypnagogic/Hypnopompic Hallucinations: Sleep apnea can also contribute to the occurrence of hypnagogic and hypnopompic hallucinations, which are vivid dream-like experiences that can occur during the transition between sleep and wakefulness. These hallucinations are closely associated with sleep paralysis. The disrupted sleep caused by sleep apnea can lead to an increase in these hallucinations, which in turn can trigger sleep paralysis episodes.
It is important for individuals with sleep apnea to be aware of the potential link between sleep apnea and sleep paralysis. Seeking treatment for sleep apnea, such as continuous positive airway pressure (CPAP) therapy, can help alleviate both conditions. By ensuring proper treatment and management of sleep apnea, individuals may experience a reduction in the frequency and severity of sleep paralysis episodes.
Other Sleep Disorders’ Connection
Other sleep disorders can have a significant connection to sleep paralysis. One such disorder is restless legs syndrome (RLS), which is characterized by an irresistible urge to move the legs during rest, often accompanied by uncomfortable sensations in the legs. Research has found a strong association between RLS and sleep paralysis, with individuals experiencing RLS symptoms being more likely to also experience sleep paralysis. Obstructive sleep apnea (OSA) is another sleep disorder that has been linked to sleep paralysis. OSA occurs when the airway becomes partially or completely blocked during sleep, leading to pauses in breathing and disrupted sleep. Studies have found that individuals with OSA are more prone to experiencing sleep paralysis episodes. Additionally, sleep-related movement disorders such as periodic limb movement disorder (PLMD) and REM sleep behavior disorder (RBD) have also been associated with sleep paralysis. PLMD involves repetitive movements of the limbs during sleep, while RBD is characterized by the acting out of dreams during REM sleep. Both of these disorders have shown a connection to increased occurrences of sleep paralysis. Understanding the connections between sleep paralysis and these other sleep disorders can provide valuable insights into the underlying mechanisms and potential treatment options for those experiencing sleep paralysis.
Impact on Mental Health
Sleep paralysis not only disrupts our physical well-being but also has a significant impact on mental health. The experience of being trapped in a state of paralysis while experiencing vivid hallucinations can be extremely distressing and unsettling, leading to feelings of intense fear and anxiety. These recurring episodes of sleep paralysis can contribute to the development of anxiety disorders, such as panic disorder and social anxiety disorder. Individuals who frequently experience sleep paralysis may be at a higher risk of developing post-traumatic stress disorder (PTSD) due to the traumatic nature of these episodes. Additionally, there is evidence to suggest that sleep paralysis is associated with an increased likelihood of experiencing depressive symptoms. The impact on mental health should not be underestimated, as it can have a profound effect on an individual’s overall quality of life. It is important for those experiencing sleep paralysis to prioritize their mental well-being and seek appropriate support.
Anxiety and Sleep Paralysis
Sleep paralysis and anxiety often go hand in hand, with anxiety being one of the most common psychological factors associated with sleep paralysis. Anxiety can both trigger and be a result of sleep paralysis episodes. When individuals experience sleep paralysis, they may feel a profound sense of fear and dread, which can exacerbate their anxiety levels. This fear can stem from the inability to move or speak, as well as from the hallucinations that sometimes accompany sleep paralysis. The uncertainty and helplessness during these episodes can further fuel anxiety symptoms. On the other hand, pre-existing anxiety disorders or high levels of daily stress can also increase the likelihood of experiencing sleep paralysis. The relationship between anxiety and sleep paralysis is complex and bidirectional, with each influencing the other. Managing anxiety through various techniques, such as cognitive-behavioral therapy or relaxation exercises, may help reduce the frequency or severity of sleep paralysis episodes. Understanding the connection between anxiety and sleep paralysis can provide individuals with valuable insights into their experiences and guide them towards effective coping mechanisms. For more information on the role of anxiety and stress in sleep paralysis, you can refer to our detailed article on Anxiety and Sleep Paralysis.
Post-Traumatic Stress Disorder (PTSD)
Post-Traumatic Stress Disorder (PTSD) is a mental health condition that can have a significant impact on sleep patterns and contribute to the occurrence of sleep paralysis. Individuals who have experienced traumatic events, such as military combat, natural disasters, or physical or sexual assault, may develop PTSD. The intense psychological distress associated with PTSD can manifest in various ways during sleep, including nightmares and sleep disturbances. Sleep paralysis has been observed as a common symptom among those with PTSD. This could be attributed to the heightened physiological and psychological arousal present in individuals with PTSD, which can disrupt the normal sleep cycle and increase the likelihood of experiencing sleep paralysis. For individuals with PTSD, the experience of sleep paralysis can further exacerbate feelings of fear, anxiety, and a loss of control. Therapy techniques, such as trauma-focused therapy and cognitive-behavioral therapy, can be beneficial in addressing both the symptoms of PTSD and any sleep-related issues, including sleep paralysis. It is important for individuals with PTSD to seek professional help and support to manage their symptoms and improve overall sleep quality.
Depression and Sleep Paralysis
Depression and sleep paralysis have been found to have a complex and interconnected relationship. While it is not yet fully understood why they are linked, research suggests that there may be several contributing factors.
1. Disrupted Sleep Patterns: Depression can often lead to disrupted sleep patterns, including frequent awakenings during the night. These disruptions can increase the likelihood of experiencing episodes of sleep paralysis, as they disrupt the normal REM sleep cycle.
2. Biological Factors: Both depression and sleep paralysis are thought to involve abnormalities in certain neurotransmitters, such as serotonin and dopamine. These imbalances in brain chemistry may play a role in the development and persistence of both conditions.
3. Psychological Factors: The experience of sleep paralysis itself can be highly distressing and can lead to feelings of fear, anxiety, and helplessness. Such emotional distress can contribute to the development or exacerbation of depressive symptoms.
4. Shared Risk Factors: Depression and sleep paralysis share common risk factors such as a history of trauma, stress, and other mental health disorders. These risk factors may also contribute to the overlap between the two conditions.
It is important to note that while there is a correlation between depression and sleep paralysis, one does not necessarily cause the other. Both conditions are complex and influenced by various biological, psychological, and environmental factors. If you are experiencing symptoms of depression, such as persistent sadness, loss of interest in activities, or difficulty sleeping, it is important to seek professional help from a healthcare provider. They can provide an accurate diagnosis and recommend appropriate treatment options that address both depression and sleep paralysis.
Managing and Preventing Sleep Paralysis
When it comes to managing and preventing sleep paralysis, there are several strategies that can be effective in reducing the frequency and intensity of episodes. Sleep hygiene plays a crucial role in promoting healthy sleep patterns and can help prevent sleep paralysis. This includes maintaining a consistent sleep schedule, creating a comfortable sleep environment, and avoiding stimulants such as caffeine and electronics before bed. Stress management techniques such as relaxation exercises, mindfulness, and incorporating stress-reducing activities into your daily routine can also be beneficial. Another intriguing approach is employing lucid dreaming techniques, which involves training your mind to recognize when you are dreaming, giving you the ability to take control of the dream and potentially prevent sleep paralysis from occurring. By implementing these strategies, individuals can take an active role in managing their sleep and reducing the likelihood of experiencing sleep paralysis episodes.
Sleep Hygiene
When it comes to managing and preventing sleep paralysis, practicing good sleep hygiene is crucial. Sleep hygiene refers to the habits and practices that promote healthy sleep. By incorporating these habits into your daily routine, you can improve the quality of your sleep and potentially reduce the occurrence of sleep paralysis episodes. Here are some key tips for maintaining good sleep hygiene:
- Stick to a consistent sleep schedule: Establishing a regular sleep routine can help regulate your body’s internal clock, making it easier to fall asleep and wake up at the desired times. Aim for the same bedtime and wake-up time each day, even on weekends.
- Create a soothing sleep environment: Make your bedroom a comfortable and relaxing space. Keep the room cool, dark, and quiet, and invest in a supportive mattress and pillows. Consider using earplugs, an eye mask, or a white noise machine if necessary.
- Avoid stimulating activities before bed: Minimize exposure to bright screens, such as smartphones, tablets, and laptops, at least an hour before bedtime. The blue light emitted by these devices can interfere with the production of melatonin, a hormone that regulates sleep. Instead, engage in calming activities like reading a book or taking a warm bath.
- Limit daytime napping: If you experience sleep paralysis, it’s recommended to avoid excessive daytime napping, especially in the late afternoon or evening. Long naps or naps taken too close to bedtime can disrupt your sleep schedule and make it harder to fall asleep at night.
- Manage stress and anxiety: Stress and anxiety can contribute to sleep disturbances, including sleep paralysis. Practice relaxation techniques, such as deep breathing exercises, meditation, or yoga, to help reduce stress levels before bed.
- Avoid stimulating substances: Avoid consuming caffeine, nicotine, and alcohol close to bedtime, as they can interfere with the quality of your sleep. These substances can disrupt your sleep patterns and make you more susceptible to experiencing sleep paralysis.
By implementing these sleep hygiene practices, you can create an optimal sleep environment and promote better sleep quality, which may help reduce the occurrence of sleep paralysis episodes.
Stress Management
Stress management plays a crucial role in addressing sleep paralysis and minimizing its occurrence. Here are some effective strategies for managing stress and promoting better sleep:
1. Identify stress triggers: Take some time to identify the specific factors that contribute to your stress levels. It could be work-related pressure, relationship issues, or financial concerns. By recognizing these triggers, you can develop strategies to reduce their impact on your well-being.
2. Practice relaxation techniques: Engage in activities that promote relaxation and reduce stress. Deep breathing exercises, meditation, yoga, and progressive muscle relaxation are all effective techniques that can help calm your mind and body before bedtime.
3. Establish a bedtime routine: Create a consistent routine before bed to signal to your body that it’s time to relax and unwind. This could include activities such as reading a book, taking a warm bath, or listening to soothing music. Avoid stimulating activities, such as using electronic devices or engaging in intense exercise, close to bedtime.
4. Improve sleep environment: Create a sleep-friendly environment that promotes relaxation and restful sleep. Keep your bedroom dark, quiet, and at a comfortable temperature. Invest in a comfortable mattress and pillow to enhance your sleep quality.
5. Seek social support: Reach out to friends, family, or support groups to share your experiences and find emotional support. Talking about your stress and concerns can help alleviate their impact and provide you with a sense of comfort and understanding.
6. Engage in regular physical activity: Regular exercise has been shown to reduce stress and promote better sleep. Aim for at least 30 minutes of moderate-intensity exercise, such as walking, swimming, or cycling, most days of the week.
7. Avoid stimulants: Limit your intake of caffeine, nicotine, and alcohol, especially in the evening. These substances can interfere with sleep quality and increase feelings of anxiety and restlessness.
By incorporating these stress management techniques into your daily routine, you can create a more balanced and relaxed state of mind, decreasing the likelihood of experiencing sleep paralysis episodes. Remember, managing stress is an ongoing process, so be patient with yourself and explore what works best for you.
Lucid Dreaming Techniques
Lucid dreaming is a technique that allows individuals to become aware that they are dreaming while still in the dream state, giving them the ability to control and manipulate the dream content. For those experiencing sleep paralysis, learning and practicing lucid dreaming techniques can be an effective method of managing and preventing episodes. Below are some lucid dreaming techniques that individuals can try:
1. Reality Checks: Throughout the day, perform reality checks to determine whether you are in a dream or awake. Common reality checks include trying to push your finger through your palm or looking at a digital clock and then looking away and back again to see if the time remains the same. By regularly practicing these reality checks during wakefulness, you will increase the likelihood of performing them during a dream and realizing that you are lucid dreaming.
2. Keep a Dream Journal: Keep a journal next to your bed and write down your dreams as soon as you wake up. This practice helps improve dream recall and trains your brain to be more aware of the dream state. Reviewing your dream journal regularly can also help you identify patterns or triggers that may be linked to sleep paralysis episodes.
3. Visualization and Affirmations: Before sleeping, visualize yourself becoming aware within a dream and repeat affirmations such as “I will recognize that I am dreaming” or “I will have control in my dreams.” By setting this intention before sleep, you are priming your mind to be more receptive to the idea of lucid dreaming.
4. Mnemonic Induction of Lucid Dreams (MILD): This technique involves waking up after several hours of sleep and then setting the intention to have a lucid dream. Repeat a phrase like “I will have a lucid dream” while visualizing yourself becoming aware and in control of your dreams. After a few minutes, go back to sleep with the focused intention of entering a lucid dream.
5. Wake-Induced Lucid Dreams (WILD): This technique involves maintaining awareness as you transition from wakefulness to sleep. To practice WILD, lie down in a comfortable position and focus on staying conscious as your body relaxes. As you enter a hypnagogic state of semi-consciousness, try to enter your dreams while maintaining awareness.
Remember, mastering lucid dreaming techniques takes practice and patience. It may take some time before you are able to consistently experience lucid dreams. However, by incorporating these techniques into your routine, you can increase your chances of achieving lucidity during dreams and potentially reduce the occurrence of sleep paralysis episodes.
Conclusion
In conclusion, sleep paralysis is a mysterious and intriguing phenomenon that occurs during sleep, leaving individuals temporarily unable to move or speak. While it can be a frightening and unsettling experience, understanding the science behind sleep paralysis can help alleviate concerns and shed light on its causes and impact. It is believed to be closely related to the various stages of the sleep cycle and the complex workings of the brain, including neurological and psychological factors. Sleep paralysis is also often accompanied by hallucinations, which can be attributed to the brain’s activity during REM sleep and the interaction between the visual cortex and brain chemistry. Additionally, sleep disorders such as narcolepsy and sleep apnea have been found to be closely linked to sleep paralysis. Importantly, sleep paralysis can have a significant impact on mental health, potentially contributing to anxiety, post-traumatic stress disorder (PTSD), and depression. However, by practicing good sleep hygiene, managing stress, and exploring techniques like lucid dreaming, individuals may be able to prevent and mitigate the occurrences of sleep paralysis. Overall, while sleep paralysis may remain a perplexing phenomenon, through scientific research and a better understanding, we can navigate its effects and strive for better sleep health.
Frequently Asked Questions
What is sleep paralysis?
Sleep paralysis is a temporary condition that occurs during sleep, where individuals find themselves unable to move or speak. It often happens when transitioning between sleep stages.
Is sleep paralysis dangerous?
No, sleep paralysis itself is not physically harmful. While it can be a distressing experience, it is generally harmless and usually lasts only a few seconds to a couple of minutes.
What causes sleep paralysis?
Sleep paralysis can be caused by disruptions in the sleep cycle, neurological factors, stress, sleep deprivation, and certain sleep disorders like narcolepsy.
Can sleep paralysis be prevented?
While it may not be possible to prevent sleep paralysis entirely, maintaining good sleep hygiene, managing stress levels, and practicing relaxation techniques can help reduce the likelihood of experiencing episodes.
Are hallucinations a common component of sleep paralysis?
Yes, hallucinations often accompany sleep paralysis. These hallucinations can involve vivid and sometimes unsettling sensory experiences that give the impression of supernatural beings or threatening figures.
Does sleep paralysis always occur during REM sleep?
Sleep paralysis predominantly occurs during REM (Rapid Eye Movement) sleep, which is the sleep stage associated with dreaming. However, it can also occur during the transition between wakefulness and sleep.
Can sleep disorders like narcolepsy be linked to sleep paralysis?
Yes, sleep paralysis is commonly associated with narcolepsy, a neurological disorder characterized by excessive daytime sleepiness, sudden loss of muscle tone (cataplexy), and fragmented sleep patterns.
Are there any famous cases of sleep paralysis?
There have been reported cases of sleep paralysis throughout history, including the well-known phenomenon called the “Old Hag Syndrome,” which describes the sensation of a malevolent presence accompanied by paralysis.
How does anxiety and stress relate to sleep paralysis?
Anxiety and stress can contribute to sleep paralysis episodes. Heightened stress levels can disrupt the sleep cycle and increase the occurrence of sleep paralysis, creating a cyclical relationship between anxiety, stress, and sleep paralysis.
Can sleep paralysis impact mental health?
Yes, sleep paralysis has been linked to mental health issues such as anxiety, depression, and post-traumatic stress disorder (PTSD). The distressing nature of the experience can have a negative impact on an individual’s overall well-being.








