Living with post-traumatic stress disorder (PTSD) can be an overwhelming and challenging experience. While it is widely known that nightmares are a common symptom of PTSD, the relationship between the two is complex and still not fully understood. In this article, we will delve into the intricate connection between PTSD and nightmares, exploring the underlying causes, potential explanations, and the impact they have on the individual’s mental well-being. Additionally, we will uncover effective treatments and strategies that can help relieve the burden of nightmares for those living with PTSD. Understanding this complex relationship is crucial in order to provide support and promote healing for individuals affected by both PTSD and the distressing nightmares that often accompany it.
Understanding PTSD
PTSD (Post-traumatic stress disorder) is a complex condition that develops in some individuals after experiencing or witnessing a traumatic event. It can have a profound and lasting impact on a person’s mental and emotional well-being. PTSD is characterized by a range of symptoms, including intrusive memories, flashbacks, emotional numbness, hyperarousal, and avoidance of situations that remind them of the traumatic event. These symptoms can significantly impair daily functioning and quality of life. The causes of PTSD can vary, but they generally involve experiencing or witnessing a distressing event such as combat, sexual assault, natural disasters, or accidents. It is essential to recognize that not everyone who experiences a traumatic event will develop PTSD. Factors such as the severity of the trauma, personal resilience, and availability of support networks can also influence the likelihood of developing the disorder. Understanding the complexities of PTSD is vital for creating effective strategies for diagnosis, treatment, and support for individuals experiencing this challenging condition.
Defining PTSD
refers to the process of understanding and describing the key characteristics and diagnostic criteria of post-traumatic stress disorder. PTSD is a psychiatric disorder that can develop following exposure to a traumatic event. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) outlines specific criteria for diagnosing PTSD, which includes exposure to a traumatic event, re-experiencing symptoms such as intrusive thoughts or nightmares related to the event, avoidance of reminders of the trauma, negative changes in mood and cognition, and heightened arousal or reactivity. These symptoms must persist for more than one month and cause significant distress or impairment in daily functioning. It is important to note that the diagnosis of PTSD requires the presence of specific symptoms and their impact on the individual’s life, as well as ruling out other potential causes for the symptoms. By understanding and defining the specific criteria for PTSD, clinicians and researchers can accurately identify and provide appropriate support and interventions for individuals who are affected by this disorder. For more information on the connection between trauma and nightmares, you can refer to this article.
Causes and Symptoms of PTSD
PTSD can be triggered by a range of traumatic events, including natural disasters, physical or sexual assault, military combat, accidents, or the unexpected loss of a loved one. The specific causes of PTSD can vary from person to person, but there are common factors that contribute to its development. Anchored by a traumatic event, PTSD can arise when an individual perceives their life or the lives of others to be in danger. This overwhelming experience can disrupt the normal processing of memories and emotions, leading to the persistent symptoms of PTSD.
The symptoms of PTSD can be wide-ranging and can manifest in various ways. Intrusive memories and flashbacks are hallmark symptoms of the disorder, where individuals experience vivid recollections of the traumatic event, often feeling as if they are reliving it. These memories can be triggered by various stimuli, such as sights, sounds, or smells, associated with the traumatic event. Avoidance behaviors are common in individuals with PTSD, where they actively try to avoid anything that reminds them of the traumatic experience. This can include avoiding certain places, people, or activities that may trigger distressing memories.
Negative changes in mood and cognition are prevalent in individuals with PTSD. They may experience feelings of guilt, shame, or a negative outlook on life. They may have trouble remembering key aspects of the traumatic event or have difficulty concentrating on everyday tasks. Hyperarousal is another symptom of PTSD, where individuals constantly feel on edge or hypervigilant. They may experience difficulties with sleep, irritability, or have exaggerated startle responses to sudden, loud noises.
It is important to note that the symptoms of PTSD can vary among individuals and can have a significant impact on their daily lives. The diagnosis of PTSD requires the presence of specific symptoms for at least one month, causing significant distress or impairment in social, occupational, or other important areas of functioning. Understanding the causes and symptoms of PTSD is crucial in order to effectively identify and provide appropriate support and treatment for individuals affected by this debilitating condition.
Impact of PTSD on Mental Health
- Increased anxiety and hyperarousal: Individuals with PTSD often experience heightened levels of anxiety and hyperarousal. This can manifest as a constant state of vigilance, difficulty relaxing, being easily startled, and feeling on edge. The intrusive thoughts and memories associated with PTSD can exacerbate these symptoms, leading to a significant impact on mental health.
- Depression: PTSD can also contribute to the development of depression. The distressing nature of the traumatic event, coupled with the ongoing symptoms of PTSD, can lead to feelings of hopelessness, sadness, and a loss of interest in previously enjoyed activities. Depression and PTSD often coexist and can reinforce each other, amplifying the negative impact on mental health.
- Social and interpersonal difficulties: The effects of PTSD can extend beyond the individual’s internal state and significantly impact their relationships and social interactions. PTSD can lead to social withdrawal, a sense of detachment, and difficulties in forming or maintaining close relationships. This sense of isolation can further contribute to the deterioration of mental health.
- Impaired cognition and memory: Cognitive difficulties are commonly reported by individuals with PTSD. This may include difficulties with concentration, memory, and decision-making. The intrusive thoughts and nightmares associated with PTSD can disrupt normal cognitive processes, leading to challenges in daily functioning and overall mental well-being.
- Substance abuse: Unfortunately, individuals with PTSD may turn to substance abuse as a means of coping with the distress and emotional pain caused by their symptoms. Substance abuse further compounds the negative impact on mental health and can lead to a vicious cycle of addiction and worsening PTSD symptoms.
These are just a few examples of the wide-ranging impact that PTSD can have on an individual’s mental health. It is important to recognize that each person’s experience with PTSD may differ, and the severity of symptoms can vary. An individualized approach to treatment and support is crucial in addressing the specific mental health challenges faced by those with PTSD. For more information on the link between nightmares and traumatic experiences, or the neuroscience of nightmares, please refer to the respective articles.
The Role of Nightmares
Nightmares play a crucial role in the context of PTSD, as they are a prevalent symptom among individuals with this disorder. These distressing dreams can be intrusive, vivid, and often relive elements of the traumatic event, causing intense fear and distress. There are different types of nightmares experienced by people with PTSD, ranging from realistic replays of the traumatic event to symbolic dreams that reflect the emotional impact of the trauma. Common themes in these nightmares include threat, danger, helplessness, and loss. Nightmares can serve as a manifestation of the unresolved trauma, as they allow the mind to process and attempt to make sense of the traumatic experience during sleep. They can also act as powerful reminders, causing fear and anxiety that persists even after waking. Understanding and addressing the role of nightmares in the context of PTSD is crucial for providing effective treatment and support to individuals living with this challenging condition.
Types of Nightmares Experienced by PTSD Patients
Types of Nightmares Experienced by PTSD Patients:
Nightmares experienced by individuals with PTSD can vary in content and intensity. These distressing dreams often reflect the traumatic experiences or themes associated with the trauma. Here are some common types of nightmares frequently experienced by those with PTSD:
- Recurrent Trauma Nightmares: These nightmares involve re-experiencing the traumatic event in vivid detail. The individual may relive the sensory aspects of the trauma, such as sights, sounds, and emotions.
- Entrapment Nightmares: These nightmares revolve around being trapped or unable to escape, mirroring the feeling of helplessness often associated with trauma. The person may experience scenarios where they are confined, pursued, or unable to flee.
- Threat Nightmares: These nightmares involve scenarios where the individual perceives imminent danger or threat to themselves or others. It could include being chased, attacked, or witnessing harm being inflicted upon loved ones.
- Nightmares of Loss and Grief: Individuals with PTSD may experience nightmares that evoke feelings of loss, grief, and mourning. These nightmares may involve the deceased or the person’s inability to prevent harm or protect others.
- Survivor Guilt Nightmares: Survivors of traumatic events often experience feelings of guilt or blame. Nightmares related to survivor guilt may involve scenarios where the individual is unable to save others or escape feelings of responsibility for the traumatic event.
It is crucial to note that the content of nightmares can vary widely among individuals, influenced by their unique experiences and traumas. These nightmares can be highly distressing, leading to sleep disturbances and further exacerbating the symptoms of PTSD. Understanding the different types of nightmares experienced by individuals with PTSD enables us to develop targeted interventions to address these distressing sleep disruptions.
Common Themes and Triggers in PTSD-Related Nightmares
PTSD-related nightmares can be vivid, intense, and distressing, triggering a range of emotions and physical reactions. These nightmares often revolve around themes related to the traumatic event that led to the development of PTSD. For example, a combat veteran might experience nightmares involving scenes of warfare, while a sexual assault survivor may have nightmares depicting moments of violation or fear. These themes can vary widely depending on the individual’s unique traumatic experiences. Triggers for PTSD-related nightmares can be internal or external. Internal triggers can include thoughts, memories, or emotions associated with the traumatic event. External triggers, on the other hand, can be certain sounds, smells, or situations that remind the individual of the trauma. It is important to note that not all individuals with PTSD have nightmares directly related to their traumatic experiences. Nightmares can also manifest as symbolic representations or metaphors connected to the underlying trauma. The unpredictability and intensity of these nightmares can further contribute to sleep disturbances and increased emotional distress for individuals living with PTSD.
Explanations and Theories
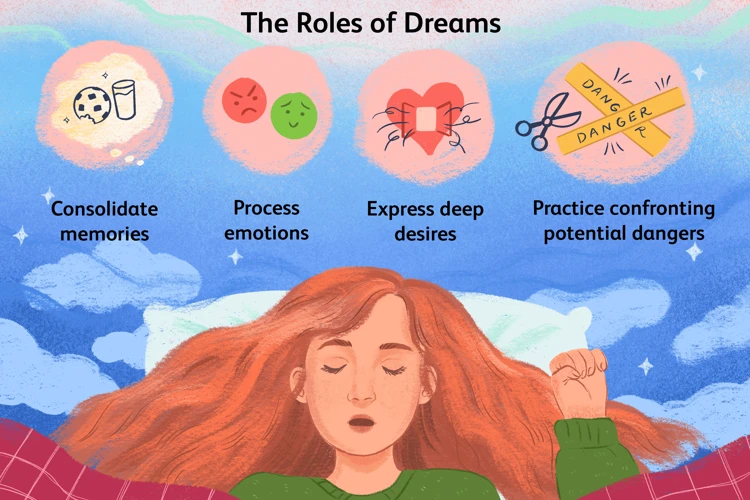
The explanations and theories surrounding the relationship between PTSD and nightmares are still undergoing research and exploration. Psychological theories suggest that nightmares in individuals with PTSD may be an attempt by the brain to process and make sense of the traumatic experiences. This theory posits that the content of the nightmares reflects the person’s unresolved fears, emotions, and memories related to the traumatic event. On the other hand, neurobiological factors are also believed to play a role. Research indicates that changes in brain chemistry and activity can contribute to the occurrence of nightmares in individuals with PTSD. The amygdala, responsible for the perception of fear and emotional memory, may become hyperactive, leading to heightened emotional responses during sleep. Additionally, disruptions in the sleep cycle, such as increased REM sleep, have been observed in PTSD patients and may contribute to nightmares. A comprehensive understanding of the complex interplay between psychological and neurobiological factors is crucial for developing effective interventions and treatments for individuals affected by both PTSD and nightmares.
Psychological Theories on the Connection
Psychological theories offer valuable insights into the connection between PTSD and nightmares. One such theory is the reconsolidation theory, which suggests that during sleep, traumatic memories and emotions associated with them are reactivated, leading to nightmares as a way for the brain to process and integrate these distressing experiences. Another theory, the threat simulation theory, proposes that nightmares serve an adaptive function by simulating threatening scenarios and allowing individuals to rehearse potential responses and coping strategies. This theory suggests that in the case of PTSD, nightmares may reflect the person’s ongoing sense of vulnerability and the need to stay vigilant against potential threats. Additionally, the emotional regulation theory posits that nightmares serve as a way for individuals to regulate their intense emotions associated with trauma, providing an opportunity for emotional processing and catharsis. These psychological theories provide a framework for understanding the intricate relationship between PTSD and nightmares, highlighting the role of the brain in processing and integrating traumatic experiences during sleep.
Neurobiological Factors at Play
Neurobiological factors play a significant role in the relationship between PTSD and nightmares. The functioning of the brain and its intricate network of neurotransmitters and hormones is a key focus of study in understanding this connection. Researchers have found that individuals with PTSD may have alterations in the brain regions responsible for regulating emotions, particularly the amygdala and prefrontal cortex. These alterations can result in heightened fear responses, hyperarousal, and difficulty with emotional regulation. Additionally, there is evidence that the neurotransmitters serotonin and norepinephrine, which are involved in the sleep-wake cycle and mood regulation, may be dysregulated in individuals with PTSD. These neurochemical imbalances can contribute to the occurrence of nightmares and the disturbance of REM sleep, the sleep stage where dreams are most vivid. Studies have shown that the brain’s stress response system, particularly the hypothalamic-pituitary-adrenal (HPA) axis, is dysregulated in individuals with PTSD. This dysregulation can lead to increased physiological arousal and the release of stress hormones like cortisol, which can impact sleep quality and contribute to nightmare frequency. Understanding the neurobiological factors at play in PTSD-related nightmares provides valuable insights into the mechanisms underlying this symptom and may guide the development of targeted treatments in the future.
Effects of Nightmares on PTSD

Nightmares can have a profound impact on individuals with PTSD (Post-traumatic stress disorder), exacerbating their symptoms and further impairing their recovery. One of the most significant effects of nightmares on PTSD is the disruption of sleep quality. Nightmares can cause severe sleep disturbances, leading to insomnia and sleep deprivation. Lack of adequate sleep can further intensify symptoms of PTSD, such as increased anxiety, irritability, and difficulty concentrating. Additionally, nightmares can retraumatize individuals, as they often involve distressing scenes or memories related to the original traumatic event. This can trigger intense emotional and physical reactions, such as panic attacks or night sweats, further deepening the individual’s distress. Effectively addressing nightmares in individuals with PTSD is crucial not only for improving their sleep quality but also for alleviating their overall symptoms and aiding in their recovery process.
Impact on Sleep Quality
The impact of nightmares on sleep quality for individuals with PTSD is profound. Nightmares can disrupt the normal sleep cycle and prevent individuals from getting the restorative sleep they need. When nightmares occur, they can induce intense emotions such as fear, anxiety, and distress, often leading to sudden awakenings throughout the night. This fragmented sleep pattern can leave individuals feeling exhausted, fatigued, and irritable during the day. As a result, their ability to function optimally is compromised, and they may struggle with concentration, memory, and decision-making. The frequent nightmares can contribute to the development of insomnia, which perpetuates a cycle of poor sleep quality and exacerbates the symptoms of PTSD. It is crucial to address the impact of nightmares on sleep quality in order to promote overall well-being and aid in the recovery process for individuals with PTSD.
Exacerbating PTSD Symptoms and Impairing Recovery
Exacerbating PTSD Symptoms and Impairing Recovery:
– Increased Hyperarousal: Nightmares can contribute to increased levels of hyperarousal in individuals with PTSD. These vivid and distressing dreams can trigger intense emotions, causing heightened anxiety, fear, and a sense of impending danger. As a result, individuals may experience an elevated state of hyperarousal, making it challenging to relax, sleep, and engage in daily activities.
– Disrupted Sleep Patterns: Nightmares can severely disrupt sleep patterns for individuals with PTSD. These distressing dreams often lead to frequent nighttime awakenings, difficulty falling back asleep, and feelings of restlessness. The disrupted sleep can result in chronic sleep deprivation, exacerbating symptoms of irritability, mood swings, and fatigue.
– Reinforcement of Traumatic Memories: Nightmares can serve as powerful reminders of the traumatic event that caused the initial onset of PTSD. They can replay distressing scenes and images associated with the trauma, reinforcing the individual’s fear and anxiety. This constant reminder can hinder the healing process and impede progress in therapy and recovery.
– Triggering Avoidance Behaviors: To avoid experiencing nightmares, individuals may develop avoidance behaviors that limit their engagement with certain activities, places, or people that might trigger distressing memories. While avoiding triggers may provide temporary relief, it can ultimately hinder the recovery process by preventing individuals from confronting and processing their trauma in a healthy and therapeutic manner.
– Deterioration of Mental Health: The presence of nightmares in individuals with PTSD can lead to a deterioration in mental health. The distress and emotional intensity associated with nightmares can contribute to increased symptoms of depression, anxiety, and overall psychological distress. This can create a vicious cycle, as worsening mental health can further exacerbate the frequency and intensity of nightmares.
It is essential to address and manage nightmares in individuals with PTSD to alleviate the burden and enhance the recovery process. By doing so, individuals can experience improved sleep quality, reduced hyperarousal, and a renewed sense of control over their symptoms, promoting overall well-being and better mental health outcomes.
Treating Nightmares in PTSD
Treating nightmares in PTSD is a vital aspect of the overall treatment plan for individuals with post-traumatic stress disorder. Psychotherapeutic approaches such as cognitive behavioral therapy (CBT) and exposure therapy have shown promising results in reducing the frequency and severity of nightmares. These therapies aim to address the underlying trauma, challenge negative thought patterns, and gradually expose the individual to distressing memories or situations in a controlled and safe manner. Additionally, medications such as prazosin and selective serotonin reuptake inhibitors (SSRIs) can be prescribed to help manage nightmares and improve sleep quality. It is crucial to understand that each individual may respond differently to treatment, and a combination of therapies may be necessary to effectively alleviate nightmares in PTSD. By providing evidence-based interventions and tailored support, healthcare professionals can help individuals with PTSD regain control over their sleep and minimize the distress caused by persistent nightmares.
Psychotherapeutic Approaches
Psychotherapy plays a vital role in helping individuals with PTSD manage their nightmares. Several psychotherapeutic approaches have shown effectiveness in alleviating nightmare severity and frequency. Cognitive Behavioral Therapy (CBT) is a commonly used psychotherapeutic intervention. It aims to modify negative thoughts and beliefs surrounding the trauma, thereby reducing the distress associated with nightmares. Within CBT, a technique called Image Rehearsal Therapy (IRT) has demonstrated success in treating nightmares. IRT involves the individual rewriting the narrative of their nightmare, transforming it into something less distressing. This technique can help reduce the intensity and emotional impact of the nightmares, ultimately leading to improved sleep quality. Eye Movement Desensitization and Reprocessing (EMDR) is another psychotherapeutic approach used in the treatment of PTSD and associated nightmares. EMDR combines guided eye movements or other forms of bilateral stimulation with therapeutic intervention. It aims to help the individual process traumatic memories and decrease their emotional response to those memories, including nightmares. Additionally, Exposure therapy may be utilized to gradually and safely expose the individual to situations or triggers associated with their trauma, allowing them to build resilience and reduce anxiety symptoms, which can also contribute to alleviating nightmares. These psychotherapeutic approaches provide individuals with valuable tools and strategies to manage and overcome the distressing nightmares associated with PTSD.
Medications and Their Effectiveness
When it comes to treating nightmares associated with PTSD, medication can be a valuable tool in the comprehensive treatment plan. There are several types of medications that healthcare professionals may prescribe to alleviate the frequency and intensity of nightmares:
1. Selective Serotonin Reuptake Inhibitors (SSRIs): SSRIs are commonly prescribed antidepressants that can help regulate serotonin levels in the brain. These medications, such as sertraline (Zoloft) or paroxetine (Paxil), have been found to reduce nightmare frequency and improve sleep quality in individuals with PTSD.
2. Prazosin: Prazosin is a medication typically used to treat high blood pressure, but it has also shown promise in reducing nightmares for individuals with PTSD. It works by blocking specific receptors in the brain, preventing the adrenaline response that often triggers nightmares.
3. Atypical Antipsychotics: In some cases, healthcare providers may prescribe atypical antipsychotic medications, such as quetiapine (Seroquel) or risperidone (Risperdal), to manage nightmares associated with PTSD. These medications can help stabilize mood and reduce symptoms related to trauma.
4. Benzodiazepines: Benzodiazepines are a class of medications that act as sedatives and can help reduce anxiety and promote sleep. However, they are generally used for short-term relief due to the risk of dependence and potential side effects.
5. Off-label Medications: In certain situations, healthcare professionals may prescribe off-label medications to address nightmares in PTSD. These may include medications like pramipexole, clonidine, or gabapentin, which have shown some efficacy in reducing nightmare frequency.
It is important to note that medication should always be prescribed and monitored by a qualified healthcare professional. The effectiveness of these medications can vary among individuals, and finding the right medication and dosage may involve some trial and error. Additionally, medication alone is rarely sufficient; it is often combined with psychotherapy or other therapeutic approaches for the best outcomes in managing PTSD-related nightmares.
Preventing Nightmares in PTSD
For individuals with PTSD, experiencing nightmares can be distressing, exacerbating their symptoms and impacting their overall well-being. While it may not be possible to completely eliminate nightmares, there are strategies that can help in preventing and managing nightmares for individuals with PTSD. Developing coping strategies, such as practicing relaxation techniques, engaging in regular physical exercise, and participating in therapy, can help individuals better cope with their emotions and reduce the frequency and intensity of nightmares. Additionally, creating a safe sleep environment can also contribute to preventing nightmares in PTSD. This may involve reducing exposure to triggers before bedtime, establishing a consistent sleep routine, and creating a comfortable and calming sleep environment. By implementing these measures, individuals living with PTSD can take steps towards minimizing the disruptive impact of nightmares on their sleep and overall well-being.
Developing Coping Strategies
Finding effective coping strategies is crucial for individuals with PTSD to manage and reduce the intensity of nightmares. Coping strategies can help restore a sense of control and provide a greater sense of safety, allowing for improved sleep quality and overall well-being. One approach to developing coping strategies involves therapy, such as Cognitive Behavioral Therapy (CBT). CBT aims to identify and challenge negative thought patterns and beliefs associated with the trauma, helping individuals develop healthier thought patterns and coping mechanisms. Another helpful coping strategy is relaxation techniques, such as deep breathing exercises, meditation, or progressive muscle relaxation. These techniques can promote relaxation before sleep, reduce anxiety, and improve overall sleep quality. Additionally, creating a structured bedtime routine and engaging in relaxing activities before sleep can help signal to the body and mind that it is time for rest. This can include activities such as reading, listening to calming music, or taking a warm bath. It is important to note that finding the right coping strategies may require some trial and error, as what works for one individual may not work for another. It is essential to work closely with a healthcare professional or therapist who can provide guidance and support throughout the process of developing effective coping strategies. By implementing and practicing these strategies, individuals with PTSD can improve their ability to manage and reduce the impact of nightmares on their overall well-being.
Creating a Safe Sleep Environment
When it comes to creating a safe sleep environment for individuals with PTSD, certain strategies can help promote a sense of safety and relaxation during bedtime. Firstly, it is important to ensure that the bedroom is a comfortable and calming space. This can be achieved by keeping the room clean, organized, and free from clutter. Soft lighting, calming colors, and soothing decor can also contribute to a peaceful atmosphere. Additionally, removing any potential triggers or reminders of trauma from the sleep environment is crucial. This may involve avoiding certain images, sounds, or scents that may evoke distressing memories. Creating a consistent bedtime routine can also be beneficial in signaling to the brain and body that it is time to relax and prepare for sleep. Engaging in relaxation techniques such as deep breathing exercises or gentle stretching before bed can further promote a sense of calmness. For individuals who experience anxiety or discomfort during the night, having comforting items such as stuffed animals, weighted blankets, or soothing music can provide a sense of security. Lastly, ensuring a quiet and noise-free environment by using earplugs or a white noise machine can help minimize disturbances that may interrupt sleep. By implementing these strategies, individuals with PTSD can create a safe and comforting sleep environment that supports improved sleep quality and a sense of security during the night.
Conclusion
In conclusion, the relationship between PTSD and nightmares is a topic that requires further exploration and understanding. While nightmares are a common symptom of PTSD, the exact mechanisms behind their occurrence and impact are complex and multifaceted. It is evident that nightmares in individuals with PTSD can have a detrimental effect on sleep quality and exacerbate the symptoms of the disorder, making the recovery process more challenging. However, through psychotherapeutic approaches and medications, there are strategies available for treating nightmares in individuals with PTSD, ultimately aiming to improve their overall well-being. Developing coping strategies and creating a safe sleep environment are also essential in preventing nightmares and providing relief for those affected by this condition. Further research into the psychological and neurobiological aspects of the PTSD-nightmare connection will contribute to a better understanding and more targeted interventions. By addressing the interplay between PTSD and nightmares, we can enhance the lives of individuals with this challenging disorder and support their journey towards healing and recovery.
Frequently Asked Questions
1. Can PTSD develop immediately after a traumatic event?
No, the symptoms of PTSD may not appear immediately after a traumatic event. In some cases, it may take days, weeks, or even months for the symptoms to manifest.
2. Are nightmares the only sleep disturbance associated with PTSD?
No, nightmares are a common sleep disturbance in individuals with PTSD, but they are not the only one. Other sleep problems include insomnia, night sweats, and sleepwalking.
3. Do all individuals with PTSD experience nightmares?
No, not all individuals with PTSD have nightmares. While nightmares are a common symptom, some individuals may experience other types of sleep disturbances or none at all.
4. Can nightmares be a sign of PTSD in children?
Yes, nightmares are often seen in children with PTSD. They may have recurring nightmares related to the traumatic event they experienced.
5. Are there specific triggers that can cause nightmares in individuals with PTSD?
Yes, certain triggers can evoke nightmares in individuals with PTSD. These triggers may include reminders of the traumatic event, specific sounds, smells, or sights associated with the trauma.
6. Can treatment for nightmares also help improve overall PTSD symptoms?
Yes, addressing and treating nightmares in individuals with PTSD can have a positive impact on their overall symptoms. Improved sleep quality can contribute to better mental health and well-being.
7. Are medications effective in reducing nightmares associated with PTSD?
Medications can be effective in reducing nightmares for some individuals with PTSD. However, their effectiveness varies, and it is important to consult a healthcare professional for appropriate medication options.
8. Can therapy help in managing nightmares related to PTSD?
Yes, therapy, such as cognitive-behavioral therapy (CBT) and eye movement desensitization and reprocessing (EMDR), can be beneficial in managing and reducing nightmares associated with PTSD.
9. Is it possible to prevent nightmares in individuals with PTSD?
While it may not be possible to completely prevent nightmares in individuals with PTSD, developing coping strategies, maintaining a consistent sleep routine, and creating a safe sleep environment can help minimize their occurrence.
10. Can PTSD nightmares ever completely disappear?
With proper treatment and support, it is possible for PTSD nightmares to reduce in frequency and intensity over time. However, individual experiences may vary, and complete elimination of nightmares may not be feasible for everyone.








