Cataplexy: a mysterious phenomenon that often boggles the mind. This enigmatic condition is commonly linked to narcolepsy, a sleep disorder that disrupts one’s daily life. Unraveling the intricate link between cataplexy and narcolepsy requires delving into the role of orexin, the impact of genetic and environmental factors, and the complex neurological pathways involved. In this article, we aim to demystify cataplexy and provide a comprehensive understanding of its connection to narcolepsy. Discover the symptoms, diagnosis criteria, and available treatment options for cataplexy, as well as strategies for living with and managing this condition. Join us on this journey of unraveling the enigma of cataplexy and gain insight into future research and advances in the field.
What is Cataplexy?
Cataplexy is a perplexing symptom that is often associated with narcolepsy. It is characterized by sudden episodes of muscle weakness or paralysis, typically triggered by strong emotions such as laughter, excitement, or anger. During a cataplectic episode, individuals may experience a range of symptoms including drooping of the face, slurred speech, buckling of the knees, or a complete collapse to the ground. These episodes can last from a few seconds to several minutes and can greatly impact an individual’s quality of life. Cataplexy is caused by a temporary loss of muscle tone, leading to weakness or paralysis, similar to the muscle atonia experienced during rapid eye movement (REM) sleep. This phenomenon occurs due to the inhibition of motor neurons by the brain during REM sleep to prevent individuals from acting out their dreams. However, in cataplexy, this muscle atonia occurs while the person is awake and conscious, resulting in temporary paralysis. Cataplexy is a hallmark symptom of narcolepsy and is believed to be caused by a lack of orexin, a neuropeptide that regulates wakefulness and REM sleep. To learn more about the fascinating connection between cataplexy, narcolepsy, and orexin, read our article “Famous Narcolepsy Success Stories”.
What is Narcolepsy?

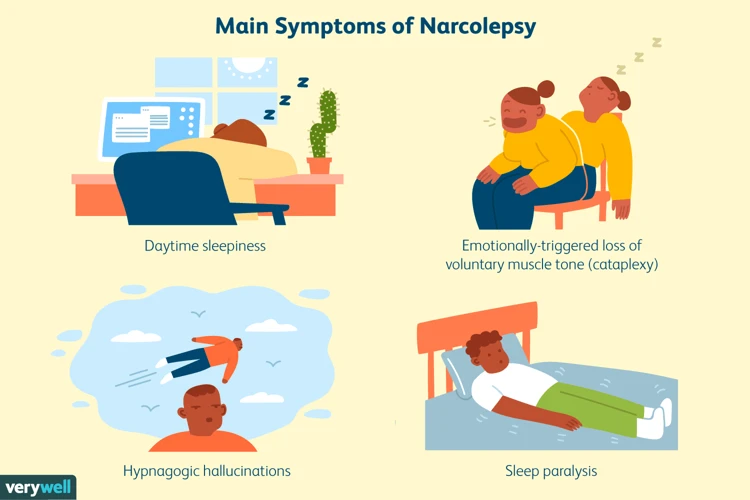
Narcolepsy is a complex neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. It is characterized by excessive daytime sleepiness, sudden uncontrollable sleep attacks, and disrupted nighttime sleep. Individuals with narcolepsy often experience excessive fatigue and struggle to stay awake during the day, regardless of how much sleep they had the night before. They may also have frequent and vivid dreams during daytime naps or while falling asleep, due to rapid entry into REM sleep. This phenomenon is known as sleep onset REM period (SOREMP). In addition to daytime sleepiness, narcolepsy can manifest in other symptoms such as cataplexy, sleep paralysis, and hypnagogic hallucinations. While the exact cause of narcolepsy is still being researched, it is believed to involve a combination of genetic predisposition and environmental factors. To learn more about the intriguing connection between narcolepsy and mental health, including the impact on dreaming and emotional well-being, read our article “Narcolepsy: The Mental Health Connection”.
The Link between Cataplexy and Narcolepsy

The link between cataplexy and narcolepsy is a complex and intriguing one. Cataplexy is considered one of the primary symptoms of narcolepsy, a neurological disorder characterized by excessive daytime sleepiness, sudden uncontrollable sleep attacks, hallucinations, and disrupted nighttime sleep. People with narcolepsy may experience cataplexy as a result of a deficiency in the neurotransmitter orexin, also known as hypocretin. Orexin plays a crucial role in regulating wakefulness and REM sleep, and its absence or dysfunction can lead to the development of both narcolepsy and cataplexy. Studies have shown that cataplexy is more commonly observed in individuals with type 1 narcolepsy, which is characterized by low or undetectable levels of orexin in the cerebrospinal fluid. However, it is important to note that cataplexy can also occur in individuals with type 2 narcolepsy, where orexin levels are relatively preserved. The exact mechanisms underlying the link between cataplexy and narcolepsy are not fully understood, but ongoing research continues to shed light on this intriguing connection. To explore the similarities and differences between narcolepsy and sleep apnea, another sleep disorder that often presents with excessive daytime sleepiness, visit our article “Narcolepsy and Sleep Apnea: Differences and Similarities”.
The Role of Orexin
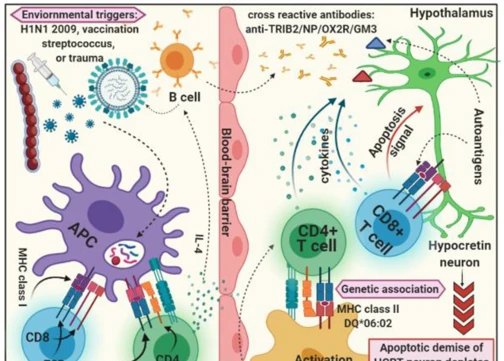
The Role of Orexin, also known as hypocretin, is crucial in understanding the connection between cataplexy and narcolepsy. Orexin is a neuropeptide produced in the hypothalamus, a region of the brain responsible for regulating various bodily functions, including sleep-wake cycles. It plays a significant role in promoting wakefulness and regulating REM sleep. In individuals with narcolepsy, including those with cataplexy, there is a deficiency of orexin due to the destruction of orexin-producing cells in the brain. This deficiency leads to a disruption in the sleep-wake cycle, resulting in excessive daytime sleepiness and the occurrence of cataplectic episodes. Research has shown that orexin acts as a stabilizer of the transition between wakefulness and REM sleep, ensuring smooth transitions and preventing sudden REM sleep intrusion during wakeful moments. The absence or reduced levels of orexin in individuals with narcolepsy cause dysregulation in this transition, leading to cataplexy episodes triggered by emotional stimuli. Understanding the role of orexin not only provides insights into the mechanism behind cataplexy but also offers potential targets for therapeutic interventions.
Genetic and Environmental Factors
Genetic and environmental factors play significant roles in the development of cataplexy and narcolepsy. Research suggests that there is a genetic predisposition to these conditions, with certain genes being associated with an increased risk. Specifically, the human leukocyte antigen (HLA) complex, which plays a role in the immune system, has been found to be involved. Variations in the HLA genes, particularly the HLA-DQB1 and HLA-DRB1 genes, have been linked to an increased risk of narcolepsy with cataplexy. Environmental factors also contribute to the development of cataplexy and narcolepsy. Infections, such as streptococcal infections, have been identified as potential triggers. Additionally, exposure to certain environmental toxins or chemicals may increase the risk of developing these conditions. The interplay between genetic and environmental factors is complex and requires further research to fully understand their contributions. Nonetheless, it is clear that both factors contribute to the development of cataplexy and narcolepsy.
Neurological Pathways Involved
The occurrence of cataplexy in individuals with narcolepsy involves a complex interplay of neurological pathways. Several brain regions and neurotransmitters are involved in regulating and modulating the symptoms of cataplexy. One key region is the hypothalamus, which plays a vital role in controlling sleep-wake cycles and the production of orexin, a neuropeptide crucial for maintaining wakefulness. In individuals with narcolepsy with cataplexy, the destruction or deficiency of orexin-producing neurons in the hypothalamus leads to a disruption in the delicate balance of neurotransmitters. The lack of orexin results in a dysregulation of various neurotransmitters, such as serotonin, dopamine, and norepinephrine, which are involved in the regulation of emotions, muscle tone, and alertness. This neurological imbalance can trigger the sudden loss of muscle tone observed during cataplectic episodes. Studies have shown that certain areas of the brain, such as the amygdala and the prefrontal cortex, which are responsible for emotional processing and regulation, also play a role in the manifestation of cataplexy. The intricate network of these neurological pathways highlights the complexity of cataplexy and brings us closer to understanding this perplexing phenomenon.
Symptoms and Diagnosis
Recognizing cataplexy can be crucial in diagnosing narcolepsy. The hallmark symptom of cataplexy is the sudden loss of muscle tone, leading to weakness or paralysis. These episodes are often triggered by intense emotions, such as laughter, excitement, or anger. The degree of muscle weakness during a cataplectic episode can vary, ranging from slight drooping of the face or slurred speech to a complete collapse. It’s important to note that cataplexy can be mistaken for other medical conditions, such as seizures or fainting spells, which is why a proper diagnosis is essential.
The diagnostic criteria for narcolepsy include the presence of cataplexy, along with other symptoms such as excessive daytime sleepiness, sleep paralysis, and hypnagogic hallucinations. To diagnose narcolepsy, a healthcare professional may conduct a thorough medical history, physical examination, and sleep studies. Sleep studies, such as polysomnography and multiple sleep latency tests, help evaluate a person’s sleep patterns, brain activity, and levels of daytime sleepiness. These tests can help confirm the presence of cataplexy and determine the severity of narcolepsy. It is important to consult a healthcare professional for an accurate diagnosis and to rule out other potential causes of similar symptoms.
Understanding the symptoms and receiving a proper diagnosis for cataplexy and narcolepsy is the first step towards managing and treating these conditions effectively. If you would like to explore further information on the relationship between narcolepsy, mental health, and emotional well-being, check out our article “The Narcolepsy-Mental Health Connection: Dreaming and Emotional Well-being”.
Recognizing Cataplexy
Recognizing cataplexy can be challenging, as it often mimics other medical conditions or is mistaken for ordinary fainting spells. A key characteristic of cataplexy is that it is triggered by intense emotions, such as laughter, surprise, or anger. The episodes of muscle weakness or paralysis during cataplexy are typically brief and reversible once the triggering emotion subsides. However, it is essential to distinguish cataplexy from other causes of muscle weakness, such as seizures or stroke. Unlike seizures, cataplexy does not involve loss of consciousness or jerking movements. It is crucial to consult a healthcare professional if you suspect cataplexy, as they can conduct a thorough evaluation by taking a detailed medical history, performing a physical examination, and ordering diagnostic tests to rule out other conditions. Evaluating the frequency, duration, and triggers of these episodes will help identify cataplexy accurately. Understanding the distinctive signs of cataplexy is vital for proper diagnosis and initiating appropriate treatment strategies.
Narcolepsy Diagnostic Criteria
To diagnose narcolepsy, healthcare professionals rely on specific diagnostic criteria. These criteria, as outlined by the International Classification of Sleep Disorders (ICSD), consist of several key components. Firstly, excessive daytime sleepiness (EDS) must be present, which is characterized by an unrestrained need to take daytime naps. Additionally, the presence of cataplexy, as discussed earlier, is a strong indicator of narcolepsy. However, not all individuals with narcolepsy experience cataplexy. Other symptoms such as sleep paralysis, hallucinations during sleep onset or awakening, and disrupted nighttime sleep may also contribute to the diagnosis. A healthcare professional will typically conduct a thorough medical history review and perform a sleep study to monitor brain activity, eye movement, and muscle tone during sleep. The results of these tests, along with the presence of the aforementioned symptoms, help confirm the diagnosis of narcolepsy. It is essential to consult with a healthcare professional to accurately diagnose and manage narcolepsy based on individual symptoms and medical history.
Treatment Options
When it comes to treating cataplexy, there are various options available that aim to manage the symptoms and improve the overall quality of life for individuals with narcolepsy. Here are some treatment options to consider:
1. Medications: Medications are often prescribed to help reduce the frequency and severity of cataplectic episodes. One commonly prescribed medication is selective serotonin reuptake inhibitors (SSRIs), which can help regulate emotions and minimize triggers. Another medication option is sodium oxybate, a central nervous system depressant, which can help improve overall sleep patterns and reduce the occurrence of cataplexy.
2. Lifestyle Adjustments: Making certain lifestyle adjustments can also play a role in managing cataplexy. Establishing a consistent sleep schedule, ensuring an adequate amount of sleep each night, and practicing good sleep hygiene can help reduce the likelihood of cataplectic episodes. Avoiding triggers such as intense emotions, sudden surprises, or stressful situations can also help minimize the risk of cataplexy.
3. Cognitive Behavioral Therapy (CBT): CBT can be beneficial for individuals with cataplexy, as it focuses on identifying and managing triggers, as well as developing coping strategies. It can help individuals recognize their emotional and physical states, and learn techniques to reduce the impact of triggers on cataplexy episodes.
4. Support and Coping Strategies: Joining support groups or therapy sessions with others who have narcolepsy can provide valuable emotional support and a sense of community. Sharing experiences, tips, and coping strategies can be immensely helpful in navigating the challenges of living with cataplexy.
It’s important to note that treatment plans may vary depending on each individual’s unique situation and needs. Consulting with a healthcare professional who specializes in sleep disorders is crucial in determining the most appropriate and effective treatment options. Remember, with the right combination of treatments and support, cataplexy can be well-managed, allowing individuals to lead fulfilling lives.
Medications
Medications play a crucial role in the management of cataplexy. There are several options available that can help reduce the frequency and severity of cataplectic episodes. One of the most commonly prescribed medications is selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine or venlafaxine. These medications help regulate serotonin levels in the brain, which can help stabilize mood and reduce the occurrence of cataplexy. Another class of medications used are tricyclic antidepressants (TCAs), such as imipramine or clomipramine, which also work to regulate serotonin levels and can effectively control cataplexy symptoms. Sodium oxybate, a medication that is taken at night, has been shown to improve both daytime sleepiness and cataplexy, making it another viable option for treatment. Additionally, stimulant medications, such as methylphenidate or modafinil, may be prescribed to help manage excessive daytime sleepiness and reduce the frequency of cataplexy episodes. It is important to consult with a healthcare professional to determine the most appropriate medication and dosage for individual needs. Regular follow-ups and adjustments may be necessary to achieve optimal symptom management. It is essential to understand that medication is just one aspect of cataplexy treatment, and it is often combined with other strategies and lifestyle adjustments to effectively manage this condition.
Lifestyle Adjustments
Lifestyle adjustments play a crucial role in managing cataplexy and minimizing its impact on daily life. Here are some recommendations for making necessary changes:
1. Establish a consistent sleep schedule: Maintaining a regular sleep routine helps regulate the sleep-wake cycle and promotes better overall sleep quality. Aim to go to bed and wake up at the same time every day, even on weekends.
2. Take short, scheduled naps: Planned, strategic naps throughout the day can help reduce excessive daytime sleepiness associated with narcolepsy. Keep the naps brief (around 15-20 minutes) to avoid interfering with nighttime sleep.
3. Create a sleep-friendly environment: Ensure that your bedroom is conducive to sleep by keeping it dark, quiet, and cool. Consider using eye masks, earplugs, or white noise machines to minimize disturbances.
4. Avoid stimulants: Stimulants like caffeine and nicotine can disrupt sleep patterns and worsen symptoms of cataplexy. Limit or eliminate the consumption of these substances, especially in the evening.
5. Exercise regularly: Engaging in regular physical activity can help improve sleep quality and reduce daytime sleepiness. However, be mindful not to exercise too close to bedtime, as it may interfere with falling asleep.
6. Manage stress: Stress and emotional turmoil can trigger cataplectic episodes. Explore stress-management techniques such as deep breathing exercises, mindfulness, yoga, or engaging in hobbies to help relax and reduce stress levels.
7. Develop a support network: Connect with others who have cataplexy or narcolepsy to share experiences and coping strategies. Joining support groups or online communities can provide valuable emotional support and practical advice.
Remember, everyone’s experience with cataplexy is unique, so it may take some trial and error to find the most effective lifestyle adjustments for you. Be patient and stay committed to finding the strategies that work best in managing your condition.
Living with Cataplexy
Living with cataplexy can be challenging, but with the right strategies and support, individuals can effectively manage their symptoms and lead fulfilling lives. One key aspect of living with cataplexy is identifying and managing triggers. Since cataplexy is often triggered by strong emotions, it can be helpful to learn relaxation techniques, such as deep breathing or meditation, to reduce the intensity of emotional responses. Additionally, avoiding situations or stimuli that commonly trigger episodes can be beneficial. Creating a supportive environment is essential for those with cataplexy. Educate family, friends, and coworkers about the condition so they can better understand and respond appropriately during episodes. Seeking support from support groups or online communities can also provide a sense of belonging and understanding.
Coping strategies are vital for managing cataplexy. Developing a consistent sleep routine and practicing good sleep hygiene can help minimize sleep disruptions and reduce the frequency of cataplectic episodes. Taking scheduled naps throughout the day may also help alleviate excessive daytime sleepiness. For individuals whose cataplexy significantly affects their daily functioning, it may be necessary to make certain lifestyle adjustments. This can include finding alternative employment arrangements, such as flexible work hours or working remotely when possible, to accommodate the unpredictable nature of cataplexy. Creating a safe living environment by removing potential hazards, such as sharp objects or obstacles, can help reduce the risk of injury during episodes.
Living with cataplexy requires a multi-faceted approach that includes managing triggers, seeking support, and implementing coping strategies. Despite the challenges, individuals with cataplexy can lead fulfilling lives by adapting their lifestyle and surrounding themselves with understanding and supportive individuals. By taking proactive steps to manage their condition, they can improve their overall quality of life.
Managing Triggers
Managing triggers is crucial for individuals with cataplexy in order to minimize the frequency and severity of episodes. Identifying and avoiding triggers can greatly improve their quality of life. Here are some strategies to effectively manage triggers:
1. Emotional Regulation: Since intense emotions often provoke cataplexy episodes, developing emotional regulation techniques can be helpful. This may involve practicing relaxation exercises, such as deep breathing or meditation, to reduce emotional arousal and maintain emotional stability.
2. Stress Management: Minimizing stress levels can play a significant role in managing cataplexy triggers. Engaging in stress-reducing activities, such as regular exercise, yoga, or mindfulness practices, can help to mitigate the impact of stress on cataplexy.
3. Sleep Hygiene: Maintaining a consistent sleep schedule and practicing good sleep hygiene can improve overall sleep quality, which in turn can help manage cataplexy symptoms. This includes ensuring a comfortable sleep environment, avoiding stimulants before bed, and establishing a relaxing bedtime routine.
4. Medication Management: Following a prescribed medication regimen is crucial for managing cataplexy triggers. Medications such as selective serotonin reuptake inhibitors (SSRIs) or sodium oxybate can be prescribed to reduce the frequency and severity of cataplexy episodes. It is important to consult with a healthcare professional to determine the most suitable medication approach.
5. Avoiding Stimulants: Stimulants, such as caffeine and certain medications, can exacerbate cataplexy symptoms. It is advisable to limit or avoid the consumption of stimulants to prevent potential trigger episodes.
6. Regular Exercise: Engaging in regular physical activity not only has numerous health benefits but can also help regulate sleep patterns and reduce stress. However, it is important to balance exercise intensity to avoid overexertion, which can sometimes trigger cataplexy.
By implementing these strategies and creating a personalized management plan with the guidance of healthcare professionals, individuals with cataplexy can gain more control over their triggers and enjoy a better quality of life.
Support and Coping Strategies
Support and coping strategies play a crucial role in assisting individuals living with cataplexy. Dealing with the challenges and limitations imposed by this condition can be overwhelming, but with the right support network and coping techniques, individuals can lead fulfilling lives. First and foremost, it is important for individuals with cataplexy to seek support from friends, family, and healthcare professionals who understand the condition and its impact. Connecting with support groups or online communities can also provide a sense of belonging and a platform for sharing experiences and advice. Additionally, educating oneself and loved ones about cataplexy can help to reduce misunderstandings and stigma surrounding the condition. Developing coping strategies is another key aspect of managing cataplexy. These strategies may include identifying triggers for cataplexy episodes and finding ways to minimize exposure to these triggers. Learning stress management techniques, such as deep breathing exercises or mindfulness meditation, can also help in reducing the frequency and severity of cataplexy episodes. Establishing a consistent sleep routine and prioritizing adequate rest can contribute to overall well-being and better management of narcolepsy symptoms. Lastly, individuals with cataplexy can explore therapeutic approaches such as cognitive-behavioral therapy (CBT) to address any emotional or psychological challenges that may arise from living with the condition. By implementing these support systems and coping strategies, individuals with cataplexy can enhance their resilience and improve their quality of life.
Research and Future Advances
Research and future advances in the field of cataplexy and narcolepsy hold promising prospects for improved understanding and treatment options. Scientists and researchers are continuously exploring various avenues to unravel the underlying mechanisms of cataplexy and its connection to narcolepsy. One area of focus is the role of genetics in the development of these conditions. Genetic studies have identified certain genes and variations that increase the risk of narcolepsy with cataplexy. Understanding these genetic factors can pave the way for targeted therapies. Additionally, advancements in neuroscience have shed light on the complex neurological pathways involved in cataplexy and narcolepsy. Researchers have discovered that the loss of orexin-producing neurons in the brain is a major contributor to the development of cataplexy and narcolepsy. This finding has led to the development of medications that target the orexin system, providing hope for more effective treatments in the future. Other areas of research include exploring the impact of environmental factors, such as infections or exposure to certain substances, on the development of cataplexy and narcolepsy. Studies are being conducted to identify the potential links between narcolepsy and mental health, as well as the differences and similarities between narcolepsy and other sleep disorders like sleep apnea. By delving deeper into these areas of research, scientists aim to uncover novel therapeutic approaches and interventions that can improve the lives of individuals with cataplexy and narcolepsy. The field of cataplexy and narcolepsy research is a rapidly evolving one, and with ongoing studies, we can expect exciting advancements that will offer new insights and better management strategies in the future.
Conclusion
In conclusion, cataplexy is a fascinating phenomenon that is intimately linked to narcolepsy. Understanding the intricate connection between these two conditions requires examining the role of orexin, the influence of genetic and environmental factors, and the complex neurological pathways involved. It is crucial to recognize the symptoms of cataplexy and understand the diagnostic criteria for narcolepsy to facilitate timely diagnosis and treatment. Although there is currently no cure for cataplexy, various treatment options, including medications and lifestyle adjustments, can help manage symptoms and improve quality of life. Additionally, individuals living with cataplexy can benefit from identifying and managing triggers and seeking support to cope with the challenges they may face. Exciting advancements in research continue to explore the mysteries of cataplexy and narcolepsy, offering hope for improved understanding, treatment, and future breakthroughs. By shedding light on the enigma of cataplexy, we can promote awareness, support, and empathy for those affected by this perplexing condition and ultimately contribute to a better quality of life for individuals with cataplexy and narcolepsy.
Frequently Asked Questions
1. How common is cataplexy?
Cataplexy is relatively rare, occurring in approximately 70-80% of individuals with narcolepsy type 1 (also known as narcolepsy with cataplexy). It is less common in individuals with narcolepsy type 2.
2. Can cataplexy be mistaken for seizures?
Yes, cataplexy episodes can resemble seizures, leading to a misdiagnosis. However, cataplexy episodes are typically triggered by emotions, while seizures have various causes and can occur spontaneously.
3. Is cataplexy treatable?
While there is no cure for cataplexy, there are treatment options available to manage the symptoms. Medications, lifestyle adjustments, and support from healthcare professionals can greatly improve the quality of life for individuals with cataplexy.
4. Are there any specific triggers for cataplexy?
Emotional triggers such as laughter, excitement, anger, or surprise are common triggers for cataplexy episodes. However, triggers can vary from person to person, and it’s important for individuals with cataplexy to identify and avoid their specific triggers.
5. Can cataplexy affect daily activities?
Yes, cataplexy can significantly impact daily activities. The sudden loss of muscle tone during cataplectic episodes can cause falls, difficulty speaking, and interfere with tasks that require muscle control such as eating or writing.
6. Is cataplexy hereditary?
There is evidence supporting a genetic predisposition to cataplexy, particularly in individuals with narcolepsy type 1. Certain genetic markers have been identified to increase the likelihood of developing cataplexy, but additional research is needed in this area.
7. Can cataplexy be diagnosed without narcolepsy?
Cataplexy is most commonly associated with narcolepsy, particularly narcolepsy type 1. However, isolated cataplexy (without other symptoms of narcolepsy) can occur in rare cases, but diagnosis and management may differ in these instances.
8. How is cataplexy diagnosed?
A diagnosis of cataplexy is typically made based on a combination of symptoms, medical history, and a sleep study called a polysomnogram. This test monitors brain activity, muscle tone, and other physiological markers during sleep.
9. Can stress worsen cataplexy symptoms?
Yes, stress can exacerbate cataplexy symptoms in some individuals. It’s important to manage stress levels and develop coping mechanisms to help reduce the frequency and severity of cataplectic episodes.
10. Can cataplexy improve over time?
In some cases, cataplexy severity can lessen over time, but this varies between individuals. Treatment options, lifestyle adjustments, and support can help individuals effectively manage cataplexy symptoms and improve their overall quality of life.