In the seemingly peaceful world of sleep, bedwetting can disrupt the tranquility and leave both children and adults perplexed. Is bedwetting simply a common occurrence or does it suggest a deeper underlying medical condition? Many individuals find themselves pondering this question as they search for answers and solutions. In this comprehensive article, we will delve into the subject of bedwetting, exploring the possible causes and considering whether it may be indicative of an underlying medical issue. We will also discuss when to seek medical advice, the diagnostic process, and the various treatment options available to help alleviate bedwetting. So, let us embark on this journey together as we unravel the mysteries of bedwetting and shed light on its potential medical significance.
What is Bedwetting?

Bedwetting, medically known as nocturnal enuresis, is a common condition characterized by the involuntary release of urine during sleep. It most frequently occurs in children, but can also affect adults. Bedwetting is considered to be normal in children under the age of five, as their bladder control develops gradually. However, if bedwetting continues beyond the age of five, it may signal an underlying issue.
There are two types of bedwetting: primary and secondary. Primary bedwetting refers to cases where the individual has never achieved consistent nighttime bladder control. Secondary bedwetting, on the other hand, occurs when a person who has been consistently dry at night for at least six months suddenly starts wetting the bed again. Secondary bedwetting is more often associated with an underlying medical condition or a stressful event.
The exact cause of bedwetting is not fully understood, but several factors have been identified as possible contributors. These factors include developmental aspects, genetic predisposition, hormonal issues, urinary tract infections, diabetes, sleep disorders, emotional stress, and constipation. It is important to note that bedwetting is not typically caused by laziness, stubbornness, or other behavioral problems.
To gain a deeper understanding of the underlying medical conditions that may be associated with bedwetting, it is essential to seek medical advice and undergo proper diagnosis. By pinpointing the root cause, effective treatment options can then be explored and implemented. So, if you or your child are experiencing bedwetting, it is crucial to consult a healthcare professional for appropriate evaluation and guidance.
For more information about the potential relationship between diet and bedwetting, you can refer to our previous article on foods and bedwetting. Additionally, if you’re specifically interested in adult bedwetting, you may find our comprehensive guide on causes and treatments for adult bedwetting helpful.
Causes of Bedwetting
Bedwetting can have various causes, ranging from developmental factors to medical conditions. Understanding these causes is crucial in determining the appropriate treatment approach. Here are some possible reasons why bedwetting occurs:
1. Developmental Factors: Bedwetting is common in younger children who are still developing bladder control. It takes time for their nervous system to mature, enabling them to awaken when their bladder is full.
2. Genetic Predisposition: There is evidence to suggest that bedwetting can run in families. If one or both parents experienced bedwetting as children, their offspring may also be more likely to struggle with it.
3. Hormonal Issues: Reduced production of an antidiuretic hormone called vasopressin, which helps control urine production, can contribute to bedwetting. This hormone slows down urine production at night, but in some individuals, its levels may be insufficient.
4. Urinary Tract Infections: Infections in the urinary tract can irritate the bladder, leading to increased urgency and bedwetting episodes.
5. Diabetes: Uncontrolled diabetes can result in increased urine production, causing bedwetting.
6. Sleep Disorders: Sleep apnea and other sleep-related breathing disorders can disrupt the normal sleep pattern, leading to bedwetting.
7. Emotional Stress: Emotional stressors such as anxiety, trauma, or major life changes can contribute to bedwetting in some individuals.
8. Constipation: When the rectum is full or impacted, it can put pressure on the bladder, causing bedwetting.
Identifying the underlying cause of bedwetting is crucial in determining the most appropriate treatment approach. To learn more about how to address bedwetting, you can refer to our comprehensive guide on how to address bedwetting.
1. Developmental Factors
Developmental factors play a significant role in bedwetting. The immaturity of the bladder and urinary control systems in young children can contribute to bedwetting. The bladder’s capacity and the ability to hold urine develop at different rates in each individual, and some children may take longer to achieve nighttime bladder control than others.
Another developmental factor is the production of a hormone called antidiuretic hormone (ADH), which helps to concentrate urine and decrease urine production during sleep. In some children, the production of ADH may be insufficient, leading to increased urine production and bedwetting. This hormone imbalance tends to normalize as the child grows older.
The development of the nervous system is also important for bladder control. In young children, the communication between the bladder and the brain may not be fully established, leading to difficulties in recognizing bladder fullness and waking up to use the toilet. As the nervous system matures, these connections strengthen, and bladder control improves.
It is essential to note that developmental factors are generally considered part of the normal maturation process. Most children eventually outgrow bedwetting as their bladder control develops with age. However, if bedwetting persists beyond the age of five or causes significant distress, it is advisable to consult a healthcare professional to rule out any underlying medical conditions and discuss appropriate treatment options.
For more information on addressing bedwetting in children, you can refer to our article on how to address bedwetting.
2. Genetic Predisposition
Genetic predisposition has been identified as a potential factor contributing to bedwetting. It is believed that certain genes may play a role in an individual’s bladder control and the development of nocturnal enuresis. Research has shown that if one or both parents experienced bedwetting as children, their offspring are more likely to also struggle with bedwetting.
While the exact genes involved in bedwetting are still being studied, it is thought that genetic factors can influence bladder capacity, the production of antidiuretic hormone (ADH), and the ability to wake up in response to a full bladder. These genetic variations may affect the coordination between the bladder muscles and the brain, leading to difficulties in achieving nighttime bladder control.
It is important to note that genetic predisposition does not guarantee that an individual will experience bedwetting. It simply increases the likelihood of developing the condition. Other factors, such as developmental stages, hormonal imbalances, and urinary tract infections, may also contribute to the manifestation of bedwetting.
Understanding the genetic aspect of bedwetting can be beneficial in terms of identifying those who may be more susceptible to the condition. This knowledge can help healthcare professionals tailor treatment approaches and provide appropriate support to individuals and families dealing with bedwetting.
It is worth noting that genetic predisposition does not imply that bedwetting cannot be treated or managed. Various treatment options, such as bedwetting alarms, bladder training exercises, medications, and behavioral techniques, can be effective in improving nighttime bladder control, even for those with a genetic predisposition to bedwetting.
To learn more about addressing bedwetting, you can refer to our detailed guide on how to address bedwetting.
3. Hormonal Issues
Hormonal issues can be a potential factor contributing to bedwetting, especially in children. Hormones play a crucial role in regulating the body’s production of urine and managing bladder control. One hormone in particular, called antidiuretic hormone (ADH) or vasopressin, helps to concentrate urine and reduce the amount of urine produced during sleep. This hormone is released by the pituitary gland and is responsible for signaling the kidneys to reabsorb water, resulting in decreased urine production at night.
However, some children may have a deficiency in ADH, leading to increased urine production during sleep and ultimately bedwetting. This condition is known as nocturnal polyuria or nocturnal excessive urine production. In such cases, the child may produce a normal amount of urine throughout the day, but an excess at night due to decreased ADH levels.
Another hormonal issue that can contribute to bedwetting is an imbalance in the regulation of the hormone cortisol, which is produced by the adrenal glands. Cortisol plays a role in urine production and bladder control. When cortisol levels are disrupted, it can affect the body’s ability to control the bladder during sleep, resulting in bedwetting.
It is important to note that hormonal issues as a cause of bedwetting are relatively rare. However, if there is a suspicion of hormonal imbalance, it is advisable to consult a healthcare professional for further evaluation and appropriate management. They may recommend specific tests to assess hormone levels and determine the most suitable course of treatment.
Understanding the potential hormonal factors contributing to bedwetting can help in the diagnosis and treatment process. By addressing hormonal imbalances, healthcare professionals can recommend appropriate interventions to help manage bedwetting and improve bladder control in affected individuals.
4. Urinary Tract Infections
Urinary tract infections (UTIs) can be a potential underlying cause of bedwetting. UTIs are infections that affect any part of the urinary system, including the kidneys, bladder, ureters, and urethra. In children, UTIs can lead to bedwetting due to the discomfort and urge to urinate that accompany the infection.
Here are some important points to consider regarding the connection between UTIs and bedwetting:
1. Increased Urge to Urinate: UTIs often cause a frequent and urgent need to urinate. This increased urge can disrupt sleep and lead to bedwetting episodes.
2. Pain or Burning Sensation: UTIs can cause pain or a burning sensation during urination. This discomfort may make it difficult for children to wake up in time to reach the bathroom, resulting in bedwetting.
3. Incomplete Emptying of the Bladder: UTIs can interfere with the normal functioning of the bladder, causing it to not empty completely. This can lead to increased nighttime urine production and bedwetting.
4. Temporary Weakening of Bladder Muscles: UTIs can potentially weaken the muscles of the bladder, affecting its ability to hold urine during sleep. This can contribute to bedwetting episodes.
It is important to note that while UTIs can be a possible cause of bedwetting, they are not the sole reason for this condition. If a UTI is suspected as the underlying cause of bedwetting, medical evaluation and appropriate treatment should be sought. A healthcare professional may recommend a urinalysis or other diagnostic tests to confirm the presence of a UTI.
Treating the UTI with antibiotics and addressing any related issues can help resolve bedwetting symptoms linked to the infection. It is essential to follow the prescribed treatment plan and ensure proper hygiene practices to prevent recurrent UTIs. Seeking medical advice and prompt treatment for UTIs can contribute to the management of bedwetting and overall urinary health.
5. Diabetes
Diabetes is a medical condition characterized by high blood sugar levels due to insufficient insulin production or ineffective use of insulin by the body. While it is not a direct cause of bedwetting, uncontrolled diabetes can contribute to nocturnal enuresis. Here’s how diabetes can potentially be linked to bedwetting:
1. Polyuria: Diabetes can lead to excessive urination, a condition called polyuria. High blood sugar levels cause the kidneys to produce more urine, resulting in frequent trips to the bathroom during the day and night. For individuals with nocturnal enuresis, the increased urine production can overwhelm the bladder’s capacity, leading to bedwetting episodes.
2. Diabetic Neuropathy: Over time, uncontrolled diabetes can cause nerve damage, especially in the peripheral nerves. This condition, known as diabetic neuropathy, can affect the nerves associated with bladder function. As a result, individuals with diabetic neuropathy may experience bladder dysfunction, including difficulty sensing a full bladder and maintaining control over urinary release during sleep.
3. Nocturia: Nocturia is a condition where individuals wake up during the night to urinate. It is commonly seen in people with diabetes, particularly those with poor blood sugar control. Nocturia can disrupt sleep patterns and increase the likelihood of bedwetting episodes, as the urge to urinate becomes more urgent and difficult to control.
It is important for individuals with bedwetting issues to consult with a healthcare professional. In the case of suspected diabetes, the doctor may order blood tests to measure blood sugar levels and assess for diabetes. Proper management of diabetes through lifestyle changes, medication, and insulin therapy can help control blood sugar levels and reduce the incidence of bedwetting associated with this condition.
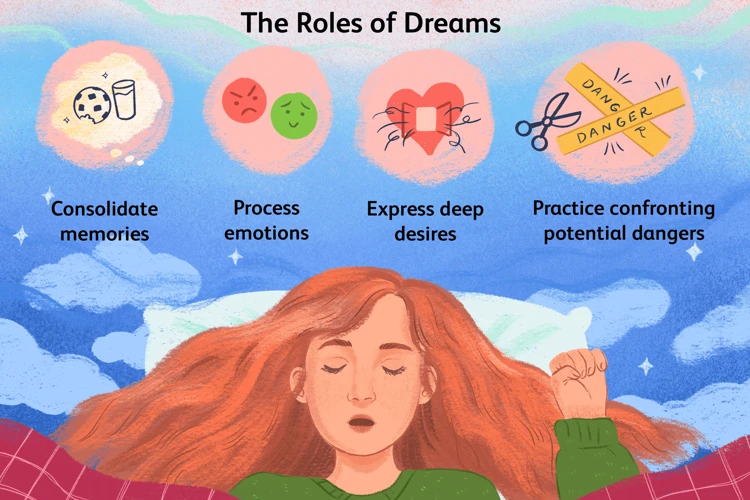
6. Sleep Disorders
Sleep disorders can be another contributing factor to bedwetting. These disorders disrupt the normal sleep pattern, making it difficult for individuals to wake up when they need to urinate. Here are some sleep disorders that have been associated with bedwetting:
1. Obstructive Sleep Apnea (OSA): OSA is a condition where breathing is repeatedly interrupted during sleep due to a physical blockage in the airway. The pauses in breathing can lead to fragmented sleep and make it challenging for individuals to wake up and go to the bathroom, resulting in bedwetting.
2. Restless Legs Syndrome (RLS): RLS causes uncomfortable sensations in the legs, often described as a crawling or tingling feeling. These sensations can disrupt sleep and contribute to bedwetting as individuals may not fully wake up when their bladder is full.
3. Narcolepsy: Narcolepsy is a neurological disorder characterized by excessive daytime sleepiness and sudden sleep attacks. The irregular sleep patterns associated with narcolepsy can lead to bedwetting, particularly during sleep episodes.
4. Parasomnias: Parasomnias are a group of sleep disorders that involve abnormal behaviors during sleep. Examples include sleepwalking, sleep talking, and night terrors. In some cases, bedwetting can occur as a result of these parasomnias.
It’s important to note that treating the underlying sleep disorder can often help resolve bedwetting. If sleep disorders are suspected as a potential cause of bedwetting, a sleep study may be recommended. During a sleep study, a person’s sleep patterns and behaviors are monitored in a controlled environment to assess the presence of any sleep disorders.
Addressing and managing sleep disorders, in conjunction with other appropriate treatment options, can significantly improve bedwetting episodes and overall quality of sleep. If you suspect that a sleep disorder may be contributing to bedwetting, it is advisable to consult a healthcare professional who specializes in sleep medicine for further evaluation and guidance.
7. Emotional Stress
Emotional stress can play a significant role in bedwetting, particularly in children. Stressful events such as moving to a new home, starting a new school, the birth of a sibling, family conflicts, or the loss of a loved one can trigger emotional turmoil and contribute to bedwetting episodes. The connection between emotions and bedwetting lies in the fact that stress activates the body’s fight-or-flight response, which can affect bladder control. When the body is under stress, it produces hormones like cortisol that can increase urine production and decrease the capacity of the bladder, making accidents more likely to occur during sleep.
Children who experience emotional stress may also inadvertently suppress their feelings, causing the stress to manifest in physical symptoms like bedwetting. Feelings of anxiety, fear, and insecurity can lead to increased bedwetting episodes. It is essential for parents and caregivers to provide a supportive and understanding environment for children facing emotional stress as they may feel embarrassed or ashamed of their bedwetting.
Addressing emotional stress requires a holistic approach that combines emotional support, open communication, and potentially professional help if needed. Encouraging children to express their emotions in a safe and nurturing environment can help alleviate some of the pressures that contribute to bedwetting. Engaging in activities that promote relaxation and stress reduction, such as mindfulness exercises, deep breathing, or engaging in hobbies they enjoy, may also be beneficial.
If emotional stress is suspected to be a significant factor in bedwetting, it is crucial to consult with a healthcare professional or a therapist who specializes in working with children or individuals experiencing emotional difficulties. They can provide valuable guidance, support, and appropriate strategies to help manage and cope with emotional stress, ultimately reducing bedwetting episodes. Remember, addressing the emotional well-being of a child or individual is an integral part of the overall approach to managing bedwetting.
8. Constipation
Constipation is another potential underlying cause of bedwetting. When a person is constipated, it means that their bowel movements are infrequent or difficult to pass. This can lead to a buildup of stool in the rectum, putting pressure on the bladder and interfering with its ability to hold urine properly.
The connection between constipation and bedwetting lies in the proximity of the bladder and bowel in the pelvic region. When the rectum becomes distended due to constipation, it can compress the bladder, reducing its capacity to hold urine. This can result in involuntary urine release during sleep.
The relationship between constipation and bedwetting is particularly significant in children. It is believed that a full rectum can trigger bladder spasms, causing involuntary urine discharge even if the child has achieved daytime control. Treating constipation by promoting regular bowel movements can often lead to a significant improvement in bedwetting.
To manage constipation, dietary changes may be necessary. Increasing fiber intake through fruits, vegetables, and whole grains can help soften the stool and promote regular bowel movements. Adequate hydration is also essential. Additionally, establishing a regular toileting routine, where the child sits on the toilet for a few minutes at specific times during the day, can encourage regular bowel movements.
In some cases, a healthcare professional may recommend the use of stool softeners or laxatives to alleviate constipation. However, it is important to consult with a medical expert before initiating any medications.
By addressing and managing constipation effectively, individuals experiencing bedwetting may see improvement in their condition. It is crucial to consider constipation as a potential cause and take appropriate steps to address it alongside other possible contributing factors.
When to Seek Medical Advice

Knowing when to seek medical advice for bedwetting is essential in determining if there are underlying medical conditions contributing to the issue. While bedwetting is relatively common in children, it is important to be aware of certain signs and situations that warrant medical attention. Here are some indicators of when seeking medical advice is recommended:
1. Age: If bedwetting persists beyond the age of 5 or continues in adolescence and adulthood, medical advice should be sought.
2. Frequency and Severity: If bedwetting occurs regularly, several times a week, or if it is accompanied by other urinary symptoms such as pain or urgency, medical attention is necessary.
3. Emotional Impact: If the bedwetting is causing significant distress or affecting the individual’s emotional well-being, seeking medical advice is important for alleviating any emotional stress associated with the condition.
4. Daytime Symptoms: If daytime symptoms such as frequent urination, urinary accidents, or urinary tract infections are present alongside bedwetting, it is advisable to consult a healthcare professional.
5. Sudden Onset or Regression: If bedwetting suddenly starts or there is a regression after a period of dryness, medical attention is warranted to investigate potential underlying causes.
6. Family History: If there is a family history of bedwetting or other urinary problems, seeking medical advice is recommended to assess any genetic predisposition or potential hereditary factors.
By recognizing these signs, individuals and parents can ensure timely intervention and appropriate medical guidance. Remember, seeking medical advice does not necessarily mean there is a serious medical condition, but it is important to rule out any underlying issues and find the most suitable treatment approach for managing bedwetting effectively.
Diagnosing Underlying Medical Conditions
When bedwetting persists beyond a certain age or is accompanied by other concerning symptoms, it may be necessary to undergo a diagnostic process to identify any underlying medical conditions. The diagnosis typically involves a combination of medical history, physical examination, and various tests. During the medical history assessment, the healthcare provider will inquire about the frequency and patterns of bedwetting episodes, as well as any related symptoms or events that may provide clues to the underlying cause. A physical examination may be performed to check for any physical abnormalities or signs of an underlying condition. Further diagnostic tests such as urinalysis, blood tests, ultrasound or imaging tests, and sometimes even a sleep study, may be recommended to gather more information and identify potential medical issues that could be contributing to the bedwetting. The diagnostic process plays a crucial role in helping healthcare professionals formulate an appropriate treatment plan for managing bedwetting and addressing any underlying medical conditions that may be present.
1. Medical History and Physical Examination
When diagnosing the underlying medical conditions associated with bedwetting, medical history and physical examination play a crucial role. During the medical history component, the healthcare provider will gather detailed information about the individual’s bedwetting history, including the frequency, patterns, and any accompanying symptoms. They may also inquire about family history of bedwetting or related conditions. This information helps paint a comprehensive picture and identify any potential predispositions or triggers.
A physical examination is then conducted to assess overall health and identify any physical abnormalities that may be contributing to the bedwetting. The healthcare provider will examine the abdomen, kidneys, bladder, and genitalia. They may also check for signs of infection or other underlying medical conditions. This examination helps rule out anatomical abnormalities or any visible signs of disease.
In some cases, additional diagnostic tests may be recommended to further investigate the underlying causes of bedwetting. These tests can provide valuable insights into the functioning of the urinary system, hormone levels, and other relevant factors. It is important to note that the specific tests conducted will depend on the healthcare provider’s assessment and the individual’s unique situation.
Medical history and physical examination form the foundation of the diagnostic process, allowing healthcare professionals to gather crucial information and assess the individual’s overall health. By understanding the potential triggers and identifying any physical abnormalities, healthcare providers can better tailor treatment plans to address the underlying medical conditions contributing to bedwetting.
2. Urinalysis
Urinalysis is a diagnostic test commonly used to evaluate the urine for any signs of infection, abnormalities, or underlying medical conditions that may be contributing to bedwetting. This non-invasive test provides valuable information about the composition and characteristics of the urine. During the urinalysis, a sample of urine is collected and analyzed in a laboratory setting. Here are some key aspects of urinalysis that help in diagnosing underlying medical conditions related to bedwetting:
1. Physical Examination: The color, clarity, and odor of the urine can provide important clues about its composition. Dark or cloudy urine may indicate the presence of blood, while a strong odor could indicate an infection.
2. Chemical Analysis: Urine is tested for the presence of various substances, such as glucose, protein, ketones, and bacteria. Elevated levels of glucose may suggest the presence of diabetes, while the presence of bacteria could indicate a urinary tract infection.
3. Microscopic Examination: A microscope is used to examine the urine for the presence of red blood cells, white blood cells, and other cellular components. The presence of red blood cells may suggest urinary tract inflammation or infection, while an increased number of white blood cells may indicate an infection.
4. Urinary pH: The pH level of the urine is measured to determine its acidity or alkalinity. Abnormal pH levels may be indicative of certain medical conditions, such as urinary tract infections or kidney problems.
5. Specific Gravity: This test measures the concentration of the urine, which can help identify issues with the kidneys’ ability to concentrate urine properly.
By analyzing the results of the urinalysis, healthcare professionals can gain valuable insights into the possible underlying causes of bedwetting. However, it is important to note that urinalysis alone may not provide a definitive diagnosis. Additional tests and evaluations may be necessary to establish a comprehensive understanding of the underlying medical condition. So, if you or your child are experiencing bedwetting, it is crucial to consult a healthcare professional for appropriate evaluation and guidance.
3. Blood Tests
Blood tests can be a valuable tool in diagnosing underlying medical conditions associated with bedwetting. When considering the possibility of an underlying condition, healthcare professionals may recommend blood tests to examine various markers and hormone levels that could provide valuable insights. Some of the common blood tests conducted for bedwetting include:
1. CBC (Complete Blood Count): This test assesses the overall health of an individual by measuring the levels of different blood components such as red blood cells, white blood cells, and platelets. An abnormal CBC can indicate the presence of infection or anemia, which may contribute to bedwetting.
2. Blood Sugar Levels: A blood test called fasting plasma glucose or A1C can determine if blood sugar levels are within the normal range. Elevated blood sugar levels could indicate the presence of diabetes, which can be a contributing factor for bedwetting.
3. Hormone Levels: Hormone imbalances, particularly in antidiuretic hormone (ADH) levels, can affect the body’s ability to regulate urine production. Blood tests can help evaluate ADH levels and identify conditions such as diabetes insipidus that may contribute to bedwetting.
4. Kidney Function: Blood tests that measure the levels of creatinine and blood urea nitrogen (BUN) can provide insights into kidney function. Impaired kidney function can affect the body’s ability to regulate urine production and contribute to bedwetting.
5. Thyroid Function: Thyroid hormones play a crucial role in growth, development, and metabolism. Imbalances in thyroid hormone levels may impact bladder control and could be a potential cause of bedwetting. Blood tests can help evaluate thyroid hormone levels and identify any abnormalities.
It is important to note that the necessity of blood tests would depend on the individual’s medical history, physical examination, and the presence of any specific symptoms or risk factors. The results from these tests, combined with other diagnostic measures, can help healthcare professionals identify and address any underlying medical conditions contributing to bedwetting.
4. Ultrasound or Imaging Tests
Ultrasound or imaging tests are commonly used diagnostic tools to evaluate the urinary system and identify any structural abnormalities that could be causing bedwetting. These tests allow healthcare professionals to get a visual representation of the kidneys, bladder, and other relevant organs. An ultrasound examination is a non-invasive procedure that uses high-frequency sound waves to produce images of the urinary tract. During the test, a small handheld device called a transducer is gently moved over the abdomen or pelvic area, emitting sound waves that create detailed images on a monitor.
The ultrasound can provide valuable information about the size and shape of the bladder and kidneys, potential blockages or abnormalities in the urinary tract, and the presence of any structural issues that may be contributing to bedwetting. It is a safe, painless, and quick procedure that does not expose the patient to any radiation.
In some cases, additional imaging tests such as a voiding cystourethrogram (VCUG) or a renal scan may be recommended. A VCUG involves the injection of a contrast dye into the bladder to enhance the X-ray images and assess the structure of the bladder and urethra during urination. This test can help identify any abnormalities in the urinary system, such as reflux or blockages.
A renal scan, also known as a nuclear medicine scan, involves the injection of a small amount of radioactive material into the bloodstream. This material collects in the kidneys, allowing healthcare professionals to observe their function and detect any abnormalities. The scan provides information about kidney size, shape, drainage, and function.
These ultrasound or imaging tests are valuable diagnostic tools in determining the underlying cause of bedwetting. They help healthcare professionals rule out structural abnormalities, identify any issues within the urinary system, and guide appropriate treatment plans. It is important to note that the need for these tests will be determined based on an individual’s medical history, physical examination, and other diagnostic findings.
5. Sleep Study
A sleep study, also known as polysomnography, is a diagnostic procedure that can be utilized to investigate bedwetting in certain cases. This specialized test involves monitoring an individual’s sleep patterns and bodily functions overnight in a sleep laboratory or at home using portable equipment. During the sleep study, various sensors are attached to the person’s body to record different physiological parameters. These parameters may include brain waves (EEG), eye movements (EOG), muscle activity (EMG), heart rate, breathing patterns, and oxygen levels.
The primary objective of a sleep study is to assess if there are any underlying sleep disorders that might be contributing to the bedwetting. One such condition is called obstructive sleep apnea (OSA), which occurs when there are recurring pauses in breathing during sleep due to airway obstruction. OSA has been associated with nocturnal enuresis, particularly in adults.
By monitoring an individual’s sleep patterns and identifying any abnormal respiratory events or disruptions, a sleep study can help determine if OSA or other sleep disorders are contributing to bedwetting. The test results can provide valuable insights into the quality and quantity of sleep, as well as any potential disruptions that may be triggering nocturnal enuresis.
It is worth mentioning that a sleep study is typically recommended when other potential underlying causes have been ruled out or if there are additional symptoms that suggest a sleep disorder. The procedure itself is painless and conducted under the supervision of a sleep technologist. Following the study, the recorded data is evaluated by sleep specialists who can interpret the results and provide appropriate recommendations for further treatment or management of bedwetting.
A sleep study is a diagnostic tool used to evaluate sleep patterns and identify any potential sleep disorders that may be contributing to bedwetting. It is a valuable resource for healthcare providers to gain insights into the complex relationship between sleep and nocturnal enuresis, aiding in the development of targeted treatment plans for individuals experiencing bedwetting.
Treatment Options
When it comes to treating bedwetting, there are several options available that can help individuals regain control over their bladder during sleep. One common treatment method is the use of bedwetting alarms, which work by detecting moisture and sounding an alarm to wake the individual up as soon as they begin to wet the bed. This helps to train the bladder and develop better nighttime control over time. Another technique is bladder training exercises, which involve creating a schedule for emptying the bladder at regular intervals throughout the day to increase its capacity and reduce the frequency of nighttime accidents. Medications may also be prescribed in certain cases to help alleviate bedwetting, such as desmopressin, which reduces urine production during sleep. Behavioral techniques, such as positive reinforcement and reward systems, can be effective in motivating children to stay dry at night. Dietary and fluid management can play a role as well, with the avoidance of certain foods and drinks before bedtime. Lastly, emotional support is crucial throughout the treatment process, as bedwetting can have an impact on an individual’s self-esteem and emotional well-being. Together, these treatment options provide a comprehensive approach to addressing bedwetting and helping individuals overcome this challenging issue.
1. Bedwetting Alarms
Bedwetting alarms are a commonly recommended and effective treatment option for managing bedwetting. These alarms work by detecting moisture or urine and triggering an audible alarm to wake the individual up when they start to wet the bed. The purpose of using bedwetting alarms is to condition the brain and bladder to recognize the sensation of a full bladder during sleep, ultimately training the individual to wake up and use the bathroom.
When considering bedwetting alarms, it’s important to understand how they work and how to use them effectively. Here are some key points to keep in mind:
1. Alarm Types: Bedwetting alarms come in various types, such as wearable alarms that attach to the underwear or pajamas, or bedside alarms that are attached to a pad placed on the bed. It’s important to choose an alarm type that is comfortable for the individual and suits their specific needs.
2. Set-Up: Proper set-up and positioning of the alarm are crucial for its effectiveness. The sensor component of the alarm should be placed where it can quickly detect moisture. For wearable alarms, the sensor should be securely attached near the child’s private area, while for bedside alarms, the sensor pad should be positioned under the bedsheet.
3. Response: When the alarm goes off, it’s important for the individual to wake up and respond promptly by going to the bathroom to finish emptying their bladder. The child or adult should be the one to turn off the alarm, rather than relying on a parent or caregiver, to reinforce their responsibility in the process.
4. Consistency: Consistent and ongoing use of bedwetting alarms is essential for effective results. It may take several weeks or even months of consistent use for the individual to achieve dry nights consistently.
5. Positive Reinforcement: Encouragement and positive reinforcement are key during the process of using bedwetting alarms. Celebrating small victories, such as dry nights or improvement over time, can help boost confidence and motivation.
It’s important to note that bedwetting alarms may not be suitable for everyone. They may not be recommended for individuals with certain medical conditions or those who do not respond well to alarm therapy. Consulting with a healthcare professional can help determine if bedwetting alarms are appropriate and provide guidance on proper usage.
In addition to bedwetting alarms, there are other treatment options available for managing bedwetting, such as bladder training exercises, medications, behavioral techniques, dietary and fluid management, and emotional support. These options can be explored based on the individual’s specific needs and the underlying causes of bedwetting.
Remember, every individual is different, and finding the most effective treatment approach may involve some trial and error. Patience, support, and understanding are essential throughout the process of managing bedwetting.
2. Bladder Training Exercises
Bladder training exercises are a non-invasive and effective approach to help improve bladder control and reduce bedwetting incidents. These exercises aim to strengthen the muscles of the bladder and increase the bladder’s capacity to hold urine. Here are some bladder training exercises that can be incorporated into a bedwetting treatment plan:
Pelvic Floor Exercises: Pelvic floor exercises, also known as kegel exercises, are commonly used to strengthen the muscles that control urination. These exercises involve contracting and relaxing the pelvic floor muscles repeatedly. This can be done by squeezing the muscles that you would use to stop the flow of urine midstream. Gradually increase the duration and number of repetitions as the muscles get stronger.
Bladder Holding: Bladder holding exercises involve consciously postponing urination when the urge to go arises. Start by attempting to hold urine for a short period, such as 15 minutes, and gradually increase the duration over time. This exercise helps increase the bladder’s capacity and trains the bladder to hold urine for longer periods.
Scheduled Voiding: Scheduled voiding involves following a strict timetable for urination throughout the day. This exercise aims to create a regular routine for emptying the bladder, which can help train the bladder to hold urine during the night. Start by scheduling bathroom breaks every two to three hours, gradually increasing the time intervals as bladder control improves.
Fluid Restriction: When implementing bladder training exercises, it may be beneficial to limit fluid intake, especially in the evening hours. However, it is important to maintain adequate hydration throughout the day, so consult with a healthcare professional for personalized fluid management recommendations.
Reward System: Incorporating a reward system can provide motivation and positive reinforcement for successfully completing bladder training exercises. Offer rewards or incentives for dry nights or successful completion of exercises, such as stickers, small prizes, or praise.
It is crucial to note that bladder training exercises may take time and consistency before results are achieved. It is recommended to consult with a healthcare professional for guidance on implementing an appropriate bladder training program tailored to individual needs. Bladder training exercises can be complemented with other treatment options, such as bedwetting alarms or medications, for a comprehensive approach to managing bedwetting.
3. Medications
Medications can be a viable option for treating bedwetting in certain cases. It is important to note that medication should only be considered after other treatment methods have been attempted and with the guidance of a healthcare professional. Here are some common medications that may be prescribed for bedwetting:
1. Desmopressin (DDAVP): This medication is a synthetic form of the hormone vasopressin, which helps reduce urine production at night. It is available in the form of tablets, nasal sprays, or oral melts. Desmopressin is often used for short-term or intermittent treatment of bedwetting, such as during sleepovers or vacations.
2. Anticholinergic drugs: These medications work by calming the bladder muscles and reducing bladder spasms. They are typically prescribed for individuals who have overactive bladder symptoms contributing to bedwetting. Examples of anticholinergic drugs include oxybutynin, tolterodine, and trospium.
3. Imipramine: This tricyclic antidepressant has been found to have an antidiuretic effect and can be used to treat primary nocturnal enuresis. Imipramine may increase the risk of side effects compared to other medications, so careful monitoring is necessary.
4. Combination therapy: In some cases, a combination of medications may be prescribed, especially when bedwetting is caused by multiple factors or when other treatment methods have not yielded satisfactory results. The specific combination of medications will depend on each individual’s unique circumstances.
It is important to remember that while medications can help manage bedwetting, they are not a cure. Once medications are discontinued, bedwetting may resume. Medications are typically used as a temporary solution alongside behavioral techniques, lifestyle modifications, and other treatment options.
The use of any medication should always be discussed with a healthcare professional who can provide guidance on the most appropriate choice and monitor its effectiveness and potential side effects.
4. Behavioral Techniques
Behavioral techniques can be effective in managing bedwetting and helping individuals gain control over their bladder function. These techniques aim to modify behaviors and establish healthy habits that promote dry nights. Here are some behavioral techniques that are commonly used:
1. Fluid Restriction: Limiting the intake of fluids, especially in the evening, can help reduce the amount of urine produced during the night. However, it is important to ensure that overall hydration needs are met and that this approach is followed under the guidance of a healthcare professional.
2. Toilet Scheduling: Encouraging regular bathroom visits before bedtime and during the day can help empty the bladder and reduce the likelihood of bedwetting. This can be done by setting specific times for toilet breaks, such as before and after meals, and before bedtime.
3. Positive Reinforcement: Creating a reward system for dry nights can motivate children and provide positive reinforcement for their efforts. This could involve small incentives such as stickers, stars, or a special treat to celebrate dry nights.
4. Bedtime Routine: Establishing a consistent bedtime routine can signal to the body that it is time to relax and prepare for sleep. This routine can include activities such as brushing teeth, reading a book, or listening to calming music, creating a relaxing environment conducive to sleep.
5. Bedwetting Alarms: Bedwetting alarms are devices that detect moisture and emit a sound or vibration to wake the individual when they begin to urinate. Over time, this helps to condition the individual to wake up before they wet the bed, allowing them to empty their bladder in the toilet.
It’s important to note that behavioral techniques may take time and consistency before desired results are achieved. Patience and support from parents, caregivers, and healthcare professionals are crucial in implementing these techniques effectively.
It is also essential to address any emotional stress or anxiety surrounding bedwetting, as this can impact progress. Open communication, reassurance, and emotional support are important aspects of managing bedwetting through behavioral techniques.
Behavioral techniques can be an effective component in the treatment of bedwetting. By implementing strategies such as fluid restriction, toilet scheduling, positive reinforcement, establishing a bedtime routine, and utilizing bedwetting alarms, individuals can take proactive steps towards achieving dry nights and gaining control over their bladder function.
5. Dietary and Fluid Management
Dietary and fluid management can play a role in managing bedwetting, especially in children. While diet alone may not cure bedwetting, making certain adjustments can potentially reduce the frequency of nighttime accidents. Here are some strategies that can be implemented:
1. Limiting Fluid Intake: Limiting fluid intake in the evening, particularly a few hours before bedtime, can help reduce the chances of bedwetting. Encourage your child to consume most of their fluids earlier in the day, ensuring they remain hydrated without overloading their bladder before sleep.
2. Avoiding Irritating Beverages: Certain beverages such as caffeinated drinks, carbonated sodas, and citrus juices can act as diuretics or irritate the bladder, making bedwetting more likely. It’s best to avoid these drinks, especially in the evening.
3. Encouraging Toilet Trips: Before bedtime, encourage your child to empty their bladder to minimize the amount of urine stored during the night. Making regular toilet trips can reduce the chances of a full bladder leading to bedwetting.
4. Fiber-Rich Diet: Ensuring an adequate intake of dietary fiber can help prevent constipation, which can contribute to bedwetting. Include fruits, vegetables, whole grains, and other fiber-rich foods in your child’s diet to promote regular bowel movements.
5. Avoiding Food Triggers: Some children may have food sensitivities or allergies that can exacerbate bedwetting. Keep an eye out for any patterns or reactions to certain foods, and consider eliminating potential triggers from their diet.
It is important to note that dietary and fluid management strategies may vary depending on the individual and the advice given by a healthcare professional. It’s always recommended to consult a healthcare provider before implementing significant dietary changes or restrictions. They can provide personalized guidance and recommend the most effective strategies for your specific situation.
Implementing these dietary and fluid management techniques, alongside other treatment options, can contribute to reducing bedwetting episodes. Remember, patience and consistency are key when it comes to managing bedwetting and finding the best approach for your child’s individual needs.
6. Emotional Support
Emotional support plays a crucial role in the management and treatment of bedwetting. Bedwetting can have a significant impact on an individual’s self-esteem and emotional well-being. It is important to create a supportive and understanding environment to help the person cope with the challenges associated with bedwetting. Here are some key aspects of emotional support:
1. Open Communication: Encourage open and honest communication about bedwetting. Let the individual know that it is not their fault and reassure them that you are there to support them.
2. Empathy and Understanding: Show empathy and understanding towards the person dealing with bedwetting. Let them know that they are not alone and that many others have experienced the same issue.
3. Positive Reinforcement: Provide positive reinforcement for dry nights and acknowledge the individual’s efforts and progress. Celebrate small victories to boost their confidence.
4. Avoid Punishment or Shame: It is essential to avoid punishing or shaming the individual for bedwetting. This can worsen their emotional distress and hinder the progress towards managing the condition.
5. Education and Awareness: Educate both the individual and their caregivers about bedwetting and its causes. This can help reduce anxiety and increase understanding of the condition.
6. Support Groups: Consider joining support groups or online communities where individuals and families dealing with bedwetting can share experiences, support each other, and exchange valuable advice and coping strategies.
7. Counseling or Therapy: In some cases, professional counseling or therapy may be beneficial, especially if the individual’s emotional well-being is severely impacted by bedwetting. A trained therapist can provide guidance and emotional support.
Remember, emotional support is a vital component of managing bedwetting. By creating a safe and understanding environment, individuals can gain the confidence and resilience needed to overcome the challenges associated with bedwetting.
Conclusion
In conclusion, bedwetting can be a distressing condition for both children and adults. While it is often considered a normal part of childhood development, it may sometimes indicate an underlying medical condition that requires attention. Understanding the various causes of bedwetting, such as developmental factors, genetic predisposition, hormonal issues, urinary tract infections, diabetes, sleep disorders, emotional stress, and constipation, can help guide individuals towards appropriate treatment options. Seeking medical advice and undergoing a proper diagnosis is crucial for identifying any potential underlying conditions. Treatment options range from bedwetting alarms and bladder training exercises to medications, behavioral techniques, dietary and fluid management, and emotional support. Remember, bedwetting should not be blamed on laziness or behavior, as it is typically involuntary. With the right support and interventions, bedwetting can be effectively managed and resolved. So, if you or your loved one is experiencing bedwetting, reach out to healthcare professionals for guidance and support.
Frequently Asked Questions
1. Is bedwetting a sign of a serious underlying medical condition?
Bedwetting can sometimes be a sign of an underlying medical condition, especially if it persists beyond the age of five or if it occurs suddenly after a period of dryness. It is important to consult a healthcare professional to rule out any potential medical issues.
2. Can emotional stress cause bedwetting?
Yes, emotional stress can contribute to bedwetting. Major life changes, traumatic events, or ongoing emotional issues can affect bladder control during sleep. Addressing and managing emotional stress can sometimes help alleviate bedwetting.
3. Are there any lifestyle factors that can influence bedwetting?
Yes, certain lifestyle factors can contribute to bedwetting. These include consuming excessive amounts of fluids before bedtime, consuming bladder irritants such as caffeine or acidic foods, and erratic sleep patterns. Modifying these factors may help improve bedwetting.
4. Can medications cause bedwetting?
Yes, some medications can affect bladder control and contribute to bedwetting. It is important to review any medications being taken and discuss concerns with a healthcare professional.
5. How effective are bedwetting alarms in treating bedwetting?
Bedwetting alarms are often considered one of the most effective treatment options for bedwetting. They work by setting off an alarm when the sensor detects moisture, conditioning the individual to wake up and use the bathroom when they feel the urge to urinate during sleep.
6. Are there any natural remedies or alternative therapies for bedwetting?
While natural remedies and alternative therapies are commonly sought, there is limited scientific evidence to support their effectiveness in treating bedwetting. It is advisable to consult with a healthcare professional for evidence-based treatment options.
7. Can constipation contribute to bedwetting?
Yes, constipation can be associated with bedwetting, particularly in children. The pressure from a full rectum can affect proper bladder emptying and lead to nighttime accidents. Treating constipation may help reduce bedwetting episodes.
8. Can bedwetting run in families?
Yes, there is evidence to suggest that bedwetting may have a genetic component. Children with parents who experienced bedwetting as children are more likely to wet the bed themselves.
9. Can bedwetting affect a child’s self-esteem?
Bedwetting can impact a child’s self-esteem, causing embarrassment, shame, and social withdrawal. Offering emotional support and reassurance, along with addressing the bedwetting issue, can help boost a child’s confidence.
10. Will my child outgrow bedwetting?
Many children do outgrow bedwetting naturally over time as their bladder control matures. However, it is important to seek appropriate medical advice and support to ensure effective management of bedwetting in the meantime.