Navigating the intricate and fascinating world of nightmares can provide valuable insights into the complex web of human emotions and experiences. Many individuals have experienced the eerie and unsettling feeling of waking up from a vivid and disturbing dream, only to find that the remnants of the nightmare linger long after they have opened their eyes. Interestingly, there is a strong connection between nightmares and Post-Traumatic Stress Disorder (PTSD), a condition that affects millions of people worldwide. In this article, we will delve into the intricacies of this connection, exploring the definition of nightmares, the symptoms of PTSD, and the various ways in which these two phenomena intertwine. Get ready to uncover the mysterious realm where dreams and trauma intersect.
The Basics of Nightmares
Nightmares, intense and often terrifying dreams, are a fascinating phenomenon that has captivated the human mind for centuries. These distressing dreams typically occur during Rapid Eye Movement (REM) sleep, a stage of sleep associated with vivid dreaming. Nightmares can vary in intensity and duration, leaving individuals feeling overwhelmed and fearful. While nightmares can be influenced by personal experiences and emotions, there are also common themes that tend to recur across different individuals. These eerie dreams often involve perilous situations, such as being chased, falling, or confronting a threatening presence. Exploring the complexities of nightmares allows us to delve deeper into the intricacies of the human mind and its connection to our deepest fears and anxieties. Understanding the basics of nightmares provides a foundation for further exploring their association with psychological disorders such as PTSD and their impact on sleep and mental well-being.
Definition of Nightmares
The definition of nightmares is a fascinating subject that delves into the intricacies of human sleep and dreams. Nightmares can be defined as vivid and distressing dreams that evoke strong negative emotions, such as fear, anxiety, or terror. These dreams often awaken individuals from their sleep, leaving them with a lingering sense of unease and dread. The content of nightmares can vary widely, but they commonly involve threatening situations, such as being pursued or attacked by an unknown entity, experiencing a traumatic event, or witnessing something horrifying. Nightmares predominantly occur during REM sleep, a stage of sleep characterized by rapid eye movements and increased brain activity. During this stage, the brain is highly active, and dreams can be especially vivid and realistic. It is important to note that occasional nightmares are normal and experienced by many individuals throughout their lives. However, when nightmares become frequent, recurrent, and significantly disrupt sleep, they can be indicative of underlying sleep disorders or psychological conditions. Understanding the definition of nightmares provides a solid foundation for exploring their causes, impact, and potential treatments. For more information on sleep disorders, you can refer to the Top 10 Sleep Disorders article.
Common Themes in Nightmares
Nightmares are not just random and chaotic dream episodes; they often follow a consistent pattern of themes that cut across cultural boundaries and individual experiences. These recurring motifs in nightmares provide valuable insights into the fears and anxieties that individuals may be grappling with. One common theme is being chased or pursued, where individuals find themselves running away from an unknown or identifiable threat. This theme taps into the primal instinct of survival and the fear of impending danger. Another prevalent theme is falling, which is often associated with a sense of loss of control and vulnerability. This theme may reflect anxieties about failure, loss, or a lack of stability in one’s life. Another disturbing theme involves being trapped or unable to escape, symbolizing feelings of being trapped in a difficult situation or trapped by one’s own emotions. Another common nightmare theme is experiencing physical harm or injury, which may arise from a fear of pain or a sense of vulnerability. Other recurring themes include being naked or exposed, which represents feelings of vulnerability and shame, and encountering supernatural beings or monsters, which can symbolize deep-seated fears or anxieties. By understanding these common themes in nightmares, we gain a deeper understanding of the human psyche and the fears that haunt our subconscious minds. It is important to note that the interpretation of these themes can vary from person to person, and exploring their personal meaning can be an enlightening and introspective process. To learn more about related sleep disorders, you can read our article on sleep paralysis or how sleep disorders can impact mental health in our comprehensive guide here.
Post-Traumatic Stress Disorder (PTSD)
Post-Traumatic Stress Disorder (PTSD) is a mental health condition that can develop after experiencing or witnessing a traumatic event. This disorder can have a profound impact on an individual’s life, causing a range of distressing symptoms. People with PTSD may experience intrusive and vivid memories of the traumatic event, often triggered by reminders or cues in their surroundings. These distressing memories can lead to intense emotional distress and physiological reactions such as rapid heartbeat or sweating. Other symptoms of PTSD include avoidance of reminders of the trauma, negative changes in mood and thinking patterns, and hyperarousal, which can manifest as difficulty sleeping or being easily startled. Overview of PTSD and its numerous symptoms highlight the immense challenges faced by those living with this condition. It is crucial to understand PTSD to comprehend its connection to nightmares and their disruptive impact on individuals’ lives.
Overview of PTSD
Post-Traumatic Stress Disorder (PTSD) is a psychiatric disorder that can develop in individuals who have experienced or witnessed a traumatic event. It is important to note that not everyone who encounters trauma will develop PTSD, but those who do often experience significant distress and disruption in their lives. Here is an overview of some key aspects of PTSD:
1. Traumatic Event: PTSD usually stems from exposure to a traumatic event, such as military combat, physical or sexual assault, natural disasters, accidents, or the sudden death of a loved one. The event is typically perceived as life-threatening or causing serious injury.
2. Diagnostic Criteria: According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), PTSD is diagnosed when an individual meets specific criteria. These criteria include experiencing the traumatic event, intrusive symptoms such as flashbacks or distressing dreams, avoidance of reminders of the event, negative changes in mood or thoughts, and hyperarousal symptoms like difficulty sleeping or being easily startled. These symptoms must persist for at least one month and cause significant impairment in functioning.
3. Prevalence and Impact: PTSD can affect individuals of all ages and backgrounds. It is estimated that about 7-8% of the population will experience PTSD in their lifetime. The disorder can have a profound impact on various aspects of a person’s life, including relationships, work, and overall quality of life.
4. Co-occurring Conditions: It is not uncommon for individuals with PTSD to also experience other mental health conditions, such as depression, anxiety disorders, substance abuse, or sleep disorders. These conditions can further exacerbate symptoms and complicate treatment.
5. Treatment Options: Fortunately, there are effective treatments available for PTSD. Psychotherapy, particularly trauma-focused therapies like Cognitive Processing Therapy (CPT) and Eye Movement Desensitization and Reprocessing (EMDR), has been shown to be beneficial. Medications, such as selective serotonin reuptake inhibitors (SSRIs), may also be prescribed to alleviate symptoms.
Understanding the basics of PTSD is crucial in recognizing the signs and symptoms of this disorder and seeking appropriate help and support for those who are affected. By providing a comprehensive overview, we can better comprehend the impact of PTSD and its connection to nightmares.
Symptoms of PTSD
Commonly referred to as PTSD, Post-Traumatic Stress Disorder is a mental health condition that can develop after experiencing or witnessing a traumatic event. The symptoms of PTSD can vary from person to person but generally fall into four main categories: intrusive thoughts, avoidance and numbing, negative mood and cognition, and hyperarousal. Individuals with PTSD may experience intrusive thoughts, nightmares, or flashbacks related to the traumatic event that can feel as vivid and terrifying as the initial experience itself. This reliving of the trauma can be distressing and lead to emotional distress and physical reactions. To cope with these distressing memories, individuals with PTSD may engage in avoidance behaviors, such as avoiding certain people, places, or activities that serve as reminders of the traumatic event. This avoidance can isolate individuals and make it difficult for them to engage in daily routines or activities. Additionally, individuals with PTSD may experience a persistent negative mood or changes in their thought patterns. They may have trouble remembering aspects of the traumatic event, have negative beliefs about themselves or the world, and struggle with feelings of guilt, shame, or blame. Individuals with PTSD often exhibit symptoms of hyperarousal, meaning they are constantly on high alert. They may experience irritability, difficulty concentrating, hypervigilance, and an exaggerated startle response. These symptoms can significantly impact a person’s daily life, relationships, and overall well-being, highlighting the urgent need for effective diagnosis and treatment of PTSD.
The Nightmares-PTSD Connection

The connection between nightmares and Post-Traumatic Stress Disorder (PTSD) is a complex and multifaceted one. Numerous studies have explored the relationship between the two, shedding light on the underlying mechanisms and interactions. Research suggests that trauma, a key component of PTSD, can trigger nightmares as a form of recurring intrusive memories. These nightmares often depict the traumatic event or related themes, replaying the distressing experiences during sleep. Recurrent nightmares can also serve as a symptom of PTSD, exacerbating the distress and emotional impact of the disorder. Understanding the nightmarish aspects of PTSD is crucial in developing effective therapeutic approaches and interventions to alleviate the burden on those who suffer from this debilitating condition.
Research and Studies
– Numerous research studies have been conducted to understand the connection between nightmares and PTSD. The findings consistently highlight the strong association between the two.
– A study published in the Journal of Traumatic Stress found that individuals with PTSD are more likely to experience nightmares compared to those without the disorder. This suggests that nightmares may be a symptom or a manifestation of the trauma experienced.
– Another study, published in the Journal of Clinical Sleep Medicine, explored the relationship between nightmares and the severity of PTSD symptoms. The researchers discovered that the intensity of nightmares was correlated with the severity of PTSD symptoms. This indicates that addressing nightmares could potentially alleviate symptoms associated with the disorder.
– Research has also shown that nightmares can serve as a predictor of the development of PTSD. A study conducted with survivors of traumatic events found that those who experienced nightmares shortly after the event were more likely to develop PTSD later on.
– Studies have also examined the neurological basis of nightmares in individuals with PTSD. These studies suggest that the amygdala, a brain structure involved in processing emotions, may play a significant role in the development and recurrence of traumatic nightmares.
– Additionally, researchers have explored the efficacy of various treatment approaches for nightmares in individuals with PTSD. Cognitive Behavioral Therapy (CBT) and Eye Movement Desensitization and Reprocessing (EMDR) have shown promise in reducing nightmare frequency and intensity.
– The collective body of research and studies provides substantial evidence for the close link between nightmares and PTSD, shedding light on the underlying mechanisms and potential avenues for treatment and intervention.
How Trauma Triggers Nightmares
Trauma has a profound impact on the human mind, and it can trigger nightmares in various ways. When an individual experiences a traumatic event, the brain often struggles to process and make sense of the overwhelming emotions and sensory information associated with the trauma. This difficulty in processing can lead to fragmented memories and unresolved emotions that manifest in nightmares. The brain tries to make sense of the traumatic experience during sleep, which can result in vivid and distressing dream scenarios. Additionally, the brain’s amygdala, which plays a key role in processing emotions, becomes hyperactive after trauma. This hyperactivity can heighten the emotional intensity of dreams, making nightmares even more vivid and frightening. The brain’s attempt to process and integrate the traumatic event during sleep can also lead to the reactivation of images, sounds, and sensations associated with the trauma, further contributing to the occurrence of nightmares. It is important to note that not all individuals who experience trauma develop nightmares, as susceptibility to nightmares can vary depending on factors such as an individual’s coping mechanisms, resilience, and pre-existing psychological vulnerabilities. Understanding how trauma triggers nightmares enables us to better comprehend the intricate interplay between our mind, emotions, and experiences, shedding light on the long-lasting effects of trauma on our sleep and mental well-being.
Recurrent Nightmares as PTSD Symptoms
Recurrent nightmares serve as one of the hallmark symptoms of Post-Traumatic Stress Disorder (PTSD). These vivid and distressing dreams are often a replay or reenactment of the traumatic event that triggered the development of PTSD. Individuals with PTSD may experience nightmares that are recurrent and persistent, causing significant distress even after waking up. These nightmares may be so intense that they can trigger physical and emotional reactions, such as increased heart rate, sweating, and feelings of fear or helplessness. They can also be accompanied by intrusive thoughts and flashbacks during waking hours, further exacerbating the impact on an individual’s mental well-being.
It is important to note that recurrent nightmares are not exclusive to PTSD and can occur in other sleep disorders or mental health conditions. However, their presence in PTSD is significant, as they are intricately linked to the traumatic event and serve as reminders of the distressing experiences an individual has endured. These nightmares can act as a way for the mind to process and attempt to make sense of the trauma, often replaying the event or elements of it in various forms.
The repetitive nature of these nightmares can become a cycle of distress, as the fear and anxiety experienced during sleep can spill over into waking life, leading to increased vigilance, hypervigilance, and avoidance behaviors. Sleep disturbances caused by recurrent nightmares can further perpetuate the symptoms of PTSD, as inadequate sleep can contribute to heightened irritability, fatigue, difficulties with concentration, and heightened emotional reactivity.
To effectively address recurrent nightmares as a symptom of PTSD, it is crucial for individuals to seek professional help. Therapeutic approaches, such as Cognitive-Behavioral Therapy for Insomnia (CBT-I) and Eye Movement Desensitization and Reprocessing (EMDR), have shown promising results in reducing the frequency and intensity of nightmares. Medications, such as alpha-blockers and selective serotonin reuptake inhibitors (SSRIs), may also be prescribed in some cases to alleviate nightmares and improve sleep quality. It is important for individuals to engage in self-help strategies as well, such as maintaining a consistent sleep schedule, practicing relaxation techniques, and creating a calming sleep environment.
The presence of recurrent nightmares in individuals with PTSD highlights the profound impact of trauma on sleep and mental well-being. By addressing and managing these symptoms, individuals can work towards better sleep and improved overall quality of life.
Impact on Sleep and Daily Life
The impact of nightmares extends beyond the realm of dreams, infiltrating the very fabric of our daily lives and disrupting our sleep patterns. The distressing and vivid nature of nightmares can lead to sleep disturbances, causing individuals to experience difficulty falling asleep or staying asleep throughout the night. As a result, sleep quality is compromised, leading to daytime drowsiness, fatigue, and difficulties in concentration and cognitive function. This can significantly impact daily productivity, performance at work or school, and overall quality of life. The emotional toll of recurring nightmares can exacerbate feelings of anxiety, fear, and depression, further contributing to the disruption of mental well-being. The intricate relationship between nightmares and sleep disruption underscores the importance of addressing and managing these unsettling dreams in order to restore peaceful and restorative sleep patterns.
Sleep Disturbances Caused by Nightmares
Sleep disturbances caused by nightmares can have a significant impact on an individual’s overall sleep quality and well-being. As nightmares are typically vivid and alarming, they can disrupt the sleep cycle, leading to frequent awakenings during the night. These disruptive awakenings can result in fragmented sleep, leaving individuals feeling tired and irritable during the day. In some cases, the fear and anxiety triggered by nightmares can make it difficult for individuals to fall back asleep, exacerbating sleep disturbances further. The emotional intensity of nightmares can linger upon waking, making it challenging to calm down and enter a relaxed state conducive to sleep. Consequently, individuals may experience difficulty initiating sleep or find themselves waking up throughout the night, causing a decrease in the overall quality and duration of their sleep. These sleep disturbances can have a ripple effect on various aspects of life, from cognitive function and mood regulation to physical health and overall well-being.
Effects on Mental Health and Well-being
The effects of nightmares on mental health and well-being cannot be underestimated. Nightmares can have a profound impact on an individual’s emotional state and overall psychological well-being. The distressing nature of nightmares can cause heightened levels of anxiety, fear, and stress, which can spill over into waking life. Constantly reliving traumatic or distressing events during nightmares can lead to a heightened sense of vigilance and hypervigilance during the day, making it difficult for individuals to relax or feel safe. This can result in chronic fatigue, irritability, and difficulty concentrating, which can impair daily functioning and negatively affect interpersonal relationships. The fear of experiencing nightmares can lead to avoidance behaviors, such as avoiding sleep or certain triggers associated with the nightmares, which can further disrupt sleep patterns and contribute to a cycle of distress. The lingering effects of nightmares on mental health and well-being highlight the importance of addressing and treating these distressing dreams to promote overall psychological wellness.
Coping Mechanisms and Treatments
Coping with nightmares and managing the symptoms of PTSD requires a multi-faceted approach that combines therapeutic interventions, medications, and self-help strategies. One effective therapeutic approach for addressing nightmares and PTSD is Cognitive-Behavioral Therapy for Insomnia (CBT-I), which focuses on improving sleep patterns and reducing anxiety. This therapy may involve techniques such as imagery rehearsal therapy, where individuals rewrite the content of their nightmares to create a more positive outcome. Another option is Eye Movement Desensitization and Reprocessing (EMDR), which helps individuals process traumatic experiences and alleviate distressing symptoms. Medications such as selective serotonin reuptake inhibitors (SSRIs) and prazosin may also be prescribed to reduce the frequency and intensity of nightmares. Additionally, self-help strategies including relaxation exercises, maintaining a consistent sleep schedule, and creating a relaxing sleep environment can play a significant role in managing nightmares and promoting better sleep. By combining these coping mechanisms and treatments, individuals can take steps towards reclaiming their sleep and improving their overall well-being.
Therapeutic Approaches
Therapeutic approaches play a crucial role in addressing nightmares and managing the underlying PTSD. Several evidence-based techniques have shown effectiveness in reducing the frequency and intensity of nightmares. One commonly used approach is Cognitive Behavioral Therapy for Insomnia (CBT-I). This therapy focuses on identifying and restructuring negative thoughts and behaviors that contribute to sleep disturbances. With the guidance of a therapist, individuals learn relaxation techniques, establish a consistent sleep schedule, and develop healthy sleep habits. Another therapeutic approach is Imagery Rehearsal Therapy (IRT), which involves rewriting and rehearsing the content of nightmares to create more positive outcomes. This technique helps individuals regain control over their dreams and transform them into less distressing experiences. Eye Movement Desensitization and Reprocessing (EMDR) therapy has also demonstrated effectiveness in treating PTSD-associated nightmares. This therapy combines trauma processing with bilateral stimulation, such as eye movements or tapping, to alleviate distressing emotions and rewire maladaptive memory networks. Mindfulness-based approaches, such as Mindfulness-Based Stress Reduction (MBSR) and Mindfulness-Based Cognitive Therapy (MBCT), can also be beneficial in managing nightmares and related symptoms by promoting relaxation, self-awareness, and acceptance. It is important to note that each individual may respond differently to various therapeutic approaches, and a personalized treatment plan should be developed in collaboration with a mental health professional.
Medications for Nightmares and PTSD
Medications can play a crucial role in managing nightmares and symptoms of PTSD. While therapy and other coping mechanisms are often the first line of defense, medications can be prescribed under the guidance of a healthcare professional to supplement treatment. There are several types of medications that have shown promise in addressing nightmares and PTSD symptoms.
1. Selective Serotonin Reuptake Inhibitors (SSRIs): SSRIs, commonly used as antidepressants, are often prescribed to individuals with PTSD. These medications work by increasing the level of serotonin in the brain, a neurotransmitter that regulates mood. SSRIs can help reduce the frequency and intensity of nightmares, as well as alleviate other symptoms of PTSD, such as anxiety and depression.
2. Prazosin: Prazosin, originally designed to treat high blood pressure, has been found to be effective in reducing nightmares associated with PTSD. It works by blocking certain receptors in the brain, which helps regulate adrenaline and norepinephrine levels. By doing so, Prazosin can help alleviate the intensity and frequency of nightmares, leading to improved sleep quality.
3. Benzodiazepines: Benzodiazepines are sedative medications that can be prescribed for individuals with severe anxiety and sleep disturbances. While they may provide short-term relief, they are generally not recommended for long-term use due to their potential for dependence and side effects.
4. Antidepressants: Other classes of antidepressant medications, such as tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs), may also be prescribed to manage nightmares and PTSD symptoms. These medications work by affecting different neurotransmitters in the brain and can help regulate sleep patterns and reduce anxiety.
It is important to note that medication should always be prescribed and monitored by a healthcare professional. Each individual’s response to medication can vary, and it may take time to find the most effective medication and dosage for managing nightmares and PTSD symptoms. Regular communication with a healthcare provider is essential to monitor the benefits and any potential side effects of the medications prescribed.
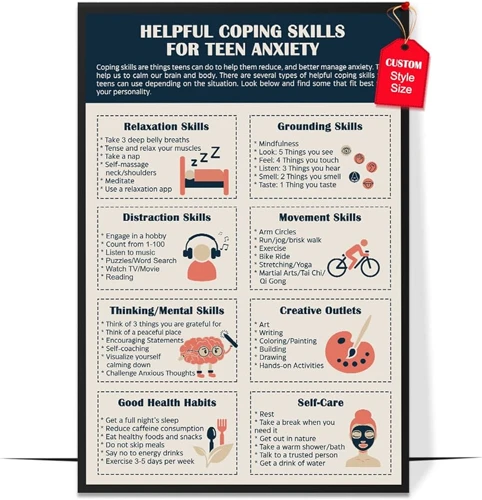
Self-Help Strategies
Self-help strategies can play a crucial role in managing nightmares and the symptoms of PTSD. These strategies empower individuals to take control of their sleep and well-being, providing a sense of autonomy and empowerment. One effective approach is practicing relaxation techniques before bedtime. Engaging in practices such as deep breathing exercises, progressive muscle relaxation, or guided imagery can help calm the mind and body, reducing anxiety and promoting a more peaceful sleep. Additionally, creating a calming bedtime routine can signal to the brain that it’s time to relax and unwind. This can include activities such as reading a book, taking a warm bath, or practicing gentle stretching. Creating a comfortable sleep environment can also contribute to better sleep. Utilizing techniques such as keeping the bedroom cool, minimizing noise and light, and investing in a supportive mattress and pillows can enhance sleep quality. Additionally, implementing stress management techniques throughout the day, such as meditation or journaling, can help alleviate underlying stress and anxiety that may contribute to nightmares. It’s important to remember that self-help strategies may vary in effectiveness for different individuals, so it’s essential to explore and experiment with various techniques to find what works best. However, if nightmares or PTSD symptoms persist or significantly impact daily life, it is recommended to seek professional help and guidance for comprehensive treatment.
Future Directions and Research
Future research in the field of nightmares and PTSD holds immense promise for advancing our understanding and improving treatment approaches. As the relationship between nightmares and PTSD continues to be explored, several key areas merit further investigation.
| 1. Longitudinal Studies: | In-depth longitudinal studies can provide valuable insights into the development and progression of nightmares in individuals with PTSD. By tracking individuals over an extended period, researchers can identify patterns and risk factors that contribute to the persistence of nightmares and their impact on mental health. |
| 2. Neurobiological Correlates: | Studying the neurobiological correlates of nightmares and PTSD can shed light on the underlying mechanisms that contribute to their co-occurrence. Investigating brain activity, neurotransmitter levels, and other physiological markers can provide a deeper understanding of the biological basis of nightmares and PTSD. |
| 3. Efficacy of Treatment Approaches: | Further research is needed to evaluate the effectiveness of different therapies and interventions for treating nightmares and PTSD. Comparing the outcomes of various therapeutic approaches, such as cognitive-behavioral therapy, exposure therapy, and eye movement desensitization and reprocessing (EMDR), can help determine the most efficient and beneficial strategies for alleviating symptoms and improving overall well-being. |
| 4. Prevention and Early Intervention: | Exploring preventative measures and early intervention strategies is crucial to mitigate the development of nightmares and PTSD. Identifying risk factors and implementing targeted interventions during critical periods, such as after a traumatic event, may help prevent the onset of debilitating nightmares and reduce the likelihood of developing PTSD. |
As research progresses, new avenues may emerge, leading to innovative and more personalized treatments. Collaborative efforts between researchers, clinicians, and individuals with lived experiences can foster a comprehensive understanding of nightmares and PTSD, ultimately paving the way for improved care and a better quality of life for those affected. The future of research in this field holds the potential to illuminate the intricate connections between dreams and trauma, offering hope and healing to individuals seeking relief from the grip of their nightmares.
Conclusion
In conclusion, the connection between nightmares and Post-Traumatic Stress Disorder (PTSD) is a complex and intriguing area of study. Through research and studies, it has become evident that trauma can trigger nightmares, and recurrent nightmares can be symptoms of PTSD. The impact of these nightmares goes beyond the realm of sleep disturbances, as they can have profound effects on mental health and overall well-being. However, there is hope for individuals experiencing these distressing dreams. Coping mechanisms and treatments, such as therapeutic approaches, medications, and self-help strategies, offer avenues for managing and alleviating the distress caused by nightmares and PTSD. Additionally, ongoing research into the field provides promising directions for future interventions and understanding. By further exploring the intricate connection between nightmares and PTSD, we can continue to enhance our knowledge and develop effective methods to support individuals on their journey to better sleep and mental health.
Frequently Asked Questions
What causes nightmares?
Nightmares can be caused by a variety of factors, including stress, anxiety, traumatic experiences, certain medications, sleep disorders, and even certain foods before bed.
Can nightmares be a symptom of PTSD?
Yes, nightmares are a common symptom of Post-Traumatic Stress Disorder (PTSD). Traumatic experiences can trigger recurring nightmares that reflect the trauma experienced.
Are nightmares harmful?
While nightmares can be distressing, they are generally not harmful on their own. However, frequent nightmares can disrupt sleep and affect overall well-being, particularly if they are part of a larger sleep disorder or mental health condition.
Can nightmares be prevented?
Preventing nightmares entirely is challenging, but adopting good sleep habits, managing stress, and addressing underlying mental health concerns can help reduce their occurrence.
What is the difference between nightmares and night terrors?
Nightmares occur during REM sleep and are vivid dreams that evoke fear or distress. Night terrors, on the other hand, occur during non-REM sleep and are episodes of intense fear or screaming, usually without vivid dream recall.
Are nightmares more common in children?
Yes, nightmares are more common in children as their imaginations and emotions are still developing. However, they can occur in individuals of all ages.
Can medications cause nightmares?
Yes, certain medications such as antidepressants, beta-blockers, and some sleep aids have been associated with an increase in nightmares as a side effect.
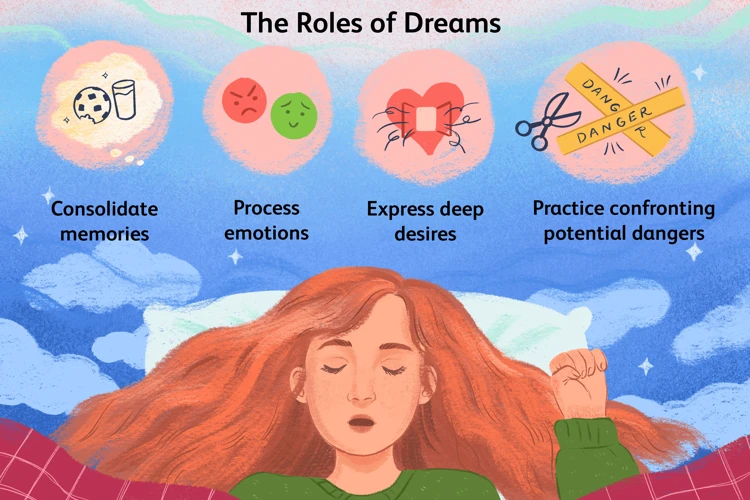
Do nightmares serve any purpose?
While the exact purpose of nightmares is still not fully understood, some theories suggest that they may help the brain process and cope with emotional experiences, particularly traumatic ones.
Can recurring nightmares be treated?
Yes, recurring nightmares can be treated through various therapeutic approaches, such as cognitive-behavioral therapy (CBT), imagery rehearsal therapy, and relaxation techniques.
How can I manage the impact of nightmares on my daily life?
Managing the impact of nightmares on daily life involves maintaining a consistent sleep schedule, practicing relaxation techniques before bedtime, creating a calming sleep environment, and seeking professional help if needed.








