Have you ever wondered how medication can affect the frequency and intensity of your nightmares? Medication plays a crucial role in managing various mental health conditions, but its impact on our dreams is often overlooked. In this article, we will delve into the intriguing world of medication and its effects on our nighttime experiences. We will explore different types of medication, such as antidepressants, antipsychotics, and anxiety medication, and how they can influence our dreaming patterns. Additionally, we’ll discuss the potential side effects and factors that can influence the medication’s impact on nightmares. So, if you’re ready to unravel the mysteries of medication and dreams, let’s dive right in.
Types of Medication

There are several types of medication that can have an impact on the frequency and intensity of nightmares. Let’s explore these medications below:
1. Antidepressants: Antidepressants are commonly prescribed to treat depression, anxiety, and other mood disorders. While they are effective in alleviating symptoms, some individuals may experience changes in their dream patterns when taking these medications. Research suggests that certain antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), may suppress REM sleep, which is the stage of sleep associated with vivid dreaming.
2. Antipsychotics: Antipsychotic medications are often prescribed for individuals with schizophrenia or bipolar disorder. These medications can also affect dream patterns and may decrease the intensity of nightmares. However, it’s important to note that the impact of antipsychotics on dreaming can vary from person to person.
3. Anxiety Medication: Anxiety medication, including benzodiazepines and selective serotonin reuptake inhibitors (SSRIs), can help manage anxiety symptoms. While these medications can contribute to better sleep quality, they may also affect dream content and reduce the occurrence of nightmares.
It’s crucial to consult with a healthcare provider or psychiatrist when considering medication for the treatment of nightmares. They can provide personalized recommendations based on individual circumstances and medical history.
1. Antidepressants
When it comes to the effects of medication on nightmares, antidepressants play a significant role. Here are some key points to consider regarding the impact of antidepressants on nightmares:
1. Suppression of REM Sleep: Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), have been linked to the suppression of REM sleep. REM sleep is the stage of sleep associated with intense dreaming. While this can be beneficial for individuals experiencing distressing nightmares, it’s essential to note that not all antidepressants have the same impact on REM sleep.
2. Changing Dream Content: Some individuals report changes in their dream content while taking antidepressants. These changes can range from reduced emotional intensity to alterations in the overall theme or narrative of the dreams. Antidepressants may influence the brain’s chemical balance, which can subsequently affect dream experiences.
3. Altered Dream Patterns: Antidepressants can alter the natural progression of sleep cycles and disrupt the normal pattern of dreams. This can lead to variations in dream recall and intensity. It’s important to note that individual responses to antidepressants can vary, and not all individuals will experience significant changes in dreaming while on these medications.
It’s crucial to discuss any concerns or questions about antidepressants and their impact on nightmares with a healthcare provider. They can provide personalized information and guidance based on your specific needs and circumstances. Additionally, exploring resources such as the role of nightmares in processing trauma can provide further insights into the complex relationship between medication and dreams.
2. Antipsychotics
Antipsychotics are a class of medication primarily used for treating conditions such as schizophrenia, bipolar disorder, and other psychotic disorders. When it comes to their impact on nightmares, antipsychotics can have variable effects. These medications work by modulating neurotransmitters in the brain, which can influence sleep patterns and dream content. While antipsychotics generally do not suppress REM sleep as strongly as some antidepressants, they may still contribute to changes in dreaming experiences. Some individuals may find that antipsychotics reduce the intensity of their nightmares, leading to more restful sleep. However, it’s important to note that the effects can differ from person to person. Research suggests that certain antipsychotic medications, such as aripiprazole, can help manage nightmares associated with post-traumatic stress disorder (PTSD). Although the exact mechanism behind this effect is not yet fully understood, it provides hope for individuals seeking relief from distressing nightmares. It’s crucial to discuss the use of antipsychotics for nightmares with a healthcare provider who can evaluate individual circumstances and recommend the most appropriate treatment approach. For those interested in exploring the symbolic meaning behind their nightmares, analyzing common symbols in nightmares can provide insight into the subconscious messages that dreams may convey.
3. Anxiety Medication
Anxiety medication, such as benzodiazepines and selective serotonin reuptake inhibitors (SSRIs), can be prescribed to individuals experiencing anxiety disorders. These medications work to reduce anxiety symptoms and promote a sense of calmness. When it comes to nightmares, anxiety medication can have both positive and negative effects.
Reducing Nightmares: Anxiety medication can help reduce the frequency and intensity of nightmares for individuals with anxiety-related sleep disturbances. By addressing the underlying anxiety and promoting better sleep quality, these medications can contribute to more peaceful and less distressing dreams.
Changing Dream Content: Some individuals on anxiety medication may experience alterations in dream content. The medication can influence the imagery and emotions within dreams, making them less anxiety-inducing or disturbing. This can bring relief to individuals who have previously experienced frequent distressing nightmares.
Side Effects: As with any medication, anxiety medications can have potential side effects. These may include drowsiness, dizziness, confusion, and even paradoxical effects such as increased anxiety or nightmares. It’s important to discuss any concerns or side effects with a healthcare provider to assess the best course of action.
It’s crucial to note that the effectiveness and impact of anxiety medication on nightmares can vary from person to person. Some individuals may find significant relief, while others may experience minimal change. Communication between the individual and their healthcare provider is essential in monitoring and adjusting the medication to best suit their needs.
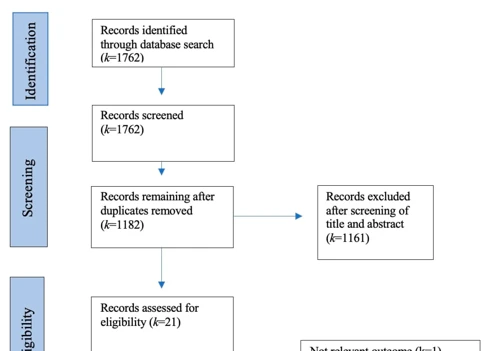
How Medication Affects Dreaming
Medication can have various effects on our dreaming patterns. Let’s explore how different medications impact our dreams:
1. Suppression of REM Sleep: Some medications, particularly antidepressants, can suppress Rapid Eye Movement (REM) sleep, which is the stage of sleep associated with vivid dreaming. This can result in a reduction in dream frequency and intensity.
2. Changing Dream Content: Certain medications, such as antipsychotics, may alter dream content. They can influence the emotional tone of dreams, making them less intense or reducing the occurrence of nightmares. However, the specific impact on dream content can vary from person to person.
3. Altered Dream Patterns: Medications may also cause changes in dream patterns, such as experiencing more or fewer dreams, or experiencing more vivid or mundane dreams. These changes can be influenced by the specific medication, dosage, and individual factors.
Understanding how medication affects dreaming can help individuals manage potential side effects and better understand their experiences during sleep. It is important to discuss any concerns or questions regarding medication and dreaming with a healthcare provider or psychiatrist to ensure appropriate management.
1. Suppression of REM Sleep
When it comes to the effect of medication on dreaming, one significant factor is the suppression of REM sleep. REM (rapid eye movement) sleep is a stage of sleep associated with vivid dreaming. Certain medications, such as some antidepressants, have been found to suppress REM sleep, thus potentially impacting the frequency and intensity of nightmares. Here are some key points to consider regarding the suppression of REM sleep:
- Antidepressants: Medications like selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed for depression and anxiety disorders. One possible side effect of these medications is a decrease in the REM sleep stage. While this can lead to a reduction in nightmares, it may also limit the overall dream content experienced during sleep.
- Impact on Nightmares: The suppression of REM sleep can lead to a decrease in the frequency of nightmares. However, it’s important to note that not all individuals may experience this effect. The impact can vary based on factors such as the specific medication, dosage, and individual response.
- Alternative Dream Patterns: In some cases, the suppression of REM sleep may result in a shift in dream patterns. Instead of vivid and memorable dreams, individuals might experience less intense and less memorable dreams. This alteration in dream content can influence the overall dream experience.
It’s essential to highlight that the impact of medication on REM sleep and nightmares can differ from person to person. Factors such as individual variation and dosage play a role in determining the specific effects. Consulting with a healthcare provider or psychiatrist is crucial in understanding the potential impact of medication on REM sleep and nightmares in individual cases.
2. Changing Dream Content
Changing dream content is another effect of medication on our nighttime experiences. Certain medications, particularly antidepressants and antipsychotics, have the potential to alter the content of our dreams. This means that the themes, emotions, and events we experience in our dreams may be influenced by the medication we are taking.
For example, some individuals may notice a reduction in vividness or intensity of their dreams while taking medication. It is not uncommon for medication to dampen emotional experiences in dreams, resulting in dreams that feel more neutral or less emotionally charged. On the other hand, some individuals may report experiencing more vivid or unusual dreams as a result of medication. These changes in dream content can vary depending on the specific medication, dosage, and individual factors.
Researchers have found that antidepressants, in particular, can impact dream content by altering neurotransmitter levels in the brain. For instance, SSRIs, which increase serotonin levels, have been associated with more positive and uplifting dream experiences. Conversely, medications that modulate dopamine levels, such as antipsychotics, may influence dream content by affecting the brain’s reward system and emotional processing.
It’s important to note that the changes in dream content can be subjective and vary from person to person. Some individuals may not notice any significant changes in their dreams while on medication, while others may experience more pronounced alterations. It’s always advisable to discuss any concerns or experiences related to dream content with a healthcare provider or psychiatrist to ensure the medication is effectively addressing your symptoms.
3. Altered Dream Patterns
Altered dream patterns are another notable effect of medication on our nighttime experiences. When individuals take certain medications, such as antidepressants or antipsychotics, it can lead to changes in the structure and content of their dreams. One common alteration is the reduction in vividness and emotional intensity of dreams. Medications can sometimes dampen the overall clarity and emotional impact of dreams, making them feel less realistic or vivid. This can be both a positive and negative effect, as it may alleviate distressing or unsettling dreams but also diminish the immersive quality of positive or neutral dreams. Additionally, some medications may disrupt the normal progression of dreams throughout the night. This could result in fragmented or disjointed dream sequences, making it difficult to recall dreams effectively. As a result, individuals may have difficulty understanding the storyline or coherent narrative structure of their dreams. It’s important to remember that the specific impact on dream patterns can vary depending on the type of medication and the individual’s unique physiological response. However, understanding these altered dream patterns can provide insight into how medication influences our nightly journeys in the realm of dreams.
Frequency and Intensity of Nightmares with Medication
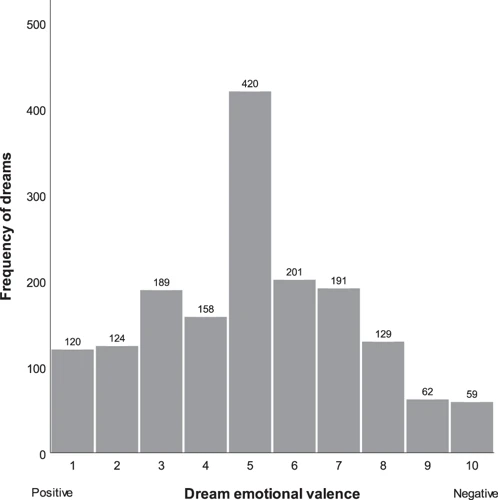
When it comes to the frequency and intensity of nightmares, medication can have varying effects. Let’s explore these effects below:
1. Decreased Frequency: Medication, particularly antidepressants and antipsychotics, can help reduce the frequency of nightmares. By addressing underlying mental health conditions or regulating brain chemistry, these medications can create a more stable sleep environment, leading to a decrease in nightmares.
2. Reduction in Intensity: Along with decreasing the frequency of nightmares, some medications may also lessen the intensity of the dreams themselves. This can provide relief to individuals experiencing distressing or highly vivid nightmares, allowing for a more restful sleep.
3. Possible Side Effects: While medication can be beneficial in managing nightmares, it’s important to be aware of potential side effects. These can vary depending on the specific medication and individual factors. Common side effects may include drowsiness, changes in appetite, or mood fluctuations. Consulting with a healthcare provider can help address any concerns and minimize potential adverse effects.
By understanding the effects that medication can have on the frequency and intensity of nightmares, individuals can make informed decisions in collaboration with their healthcare provider when choosing the most suitable treatment approach.
1. Decreased Frequency
When it comes to the effects of medication on nightmares, one of the positive outcomes that individuals may experience is a decreased frequency of nightmares. The use of certain medications, such as antidepressants and antipsychotics, has been shown to reduce the occurrence of nightmares in some individuals. These medications work by impacting brain chemicals and neurotransmitters that regulate sleep and dreaming.
Here are a few key points to consider regarding the decreased frequency of nightmares:
1. Medication Mechanisms: Antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), can help regulate serotonin levels in the brain. Increased levels of serotonin can contribute to more stable sleep patterns and a reduction in nightmares. Similarly, antipsychotic medications may also interfere with the neurochemical processes that trigger nightmares, resulting in a decreased frequency.
2. Individual Variation: It’s important to note that the impact of medication on nightmares can vary from person to person. While some individuals may experience a significant reduction in nightmare frequency, others may notice only a slight improvement or no change at all. The effectiveness of medication can depend on various factors, including the underlying cause of the nightmares and individual differences in brain chemistry.
3. Timeframe of Improvement: It’s also essential to be aware that the decrease in nightmare frequency may not occur immediately after starting medication. It may take several weeks for the medication to reach its full effect, and some individuals may need to try different medications or dosage adjustments before noticing a significant reduction in nightmares.
In any case, it is vital to work closely with a healthcare provider or psychiatrist who can monitor the effects of the medication and make necessary adjustments as needed. Regular communication with the healthcare provider is essential to ensure that the chosen medication is effectively addressing the frequency of nightmares and overall mental well-being.
2. Reduction in Intensity
When it comes to the effects of medication on nightmares, one significant outcome is the reduction in intensity. Certain medications, such as antipsychotics and some antidepressants, have the potential to lessen the severity and emotional impact of nightmares. This reduction can be particularly beneficial for individuals who experience distressing and vivid nightmares that interfere with their sleep and overall well-being.
Antipsychotic medications, commonly used in the treatment of schizophrenia and bipolar disorder, may help to minimize the intensity of nightmares. These medications work by affecting neurotransmitter activity in the brain, which can influence the content and emotional intensity of dreams. By modulating brain chemistry, antipsychotics can help to create a less distressing dream environment, reducing fear, anxiety, and other negative emotions often associated with nightmares.
Similarly, certain antidepressants can contribute to a reduction in nightmare intensity. These medications, particularly selective serotonin reuptake inhibitors (SSRIs), can alter neurotransmitter levels in the brain, leading to improved mood regulation and decreased emotional reactivity during dreams. As a result, the intensity of nightmares may be dampened, allowing for a more restful and less disruptive sleep experience.
While medication can be effective in reducing the intensity of nightmares, it is important to remember that individual responses may vary. What works for one person may not have the same impact for another. Additionally, the dosage and timing of medication can play a significant role in determining its effectiveness in reducing nightmare intensity. Finding the right balance and working closely with a healthcare provider or psychiatrist is crucial to optimize the benefits of medication in managing nightmare intensity.
Medication, particularly antipsychotics and certain antidepressants, can contribute to a reduction in the intensity of nightmares. By modulating brain chemistry and influencing neurotransmitter activity, these medications help create a less distressing dream environment and minimize the emotional impact of nightmares. However, it is essential to consider individual variations, dosage, and timing when utilizing medication for nightmare management. Consultation with a healthcare professional is the best approach to ensure the most effective and personalized treatment plan.
3. Possible Side Effects
When taking medication for nightmares, it’s important to be aware of the possible side effects that may accompany the treatment. Here are some potential side effects to consider:
- Drowsiness: Some medications used for nightmares can cause drowsiness, especially during the initial stages of treatment. It’s important to follow the prescribed dosage and avoid activities that require alertness until you know how the medication affects you.
- Changes in appetite: Certain medications may have an impact on your appetite, leading to either an increase or decrease in food intake. This can potentially affect your overall well-being, so it’s important to monitor any changes and discuss them with your healthcare provider.
- Weight gain or loss: It’s not uncommon for medications to cause weight fluctuations. Some individuals may experience weight gain, while others may experience weight loss. This can be a concern for some, so monitoring your weight and discussing any significant changes with your healthcare provider is advised.
- Gastrointestinal issues: In some cases, medication for nightmares may cause gastrointestinal side effects such as nausea, vomiting, or digestive discomfort. If these symptoms persist or worsen, it’s important to consult with your healthcare provider.
- Mood changes: Medications can sometimes affect mood and emotions. While these effects may vary from person to person, it’s important to be mindful of any significant changes in your emotional well-being and discuss them with your healthcare provider.
- Other side effects: Depending on the specific medication prescribed, there may be other potential side effects such as dry mouth, blurred vision, or changes in libido. It’s important to familiarize yourself with the potential side effects of the medication and report any concerns to your healthcare provider.
Remember, everyone’s response to medication can vary, and not everyone will experience these side effects. However, it’s important to be aware of them and have open communication with your healthcare provider throughout the treatment process. They can offer guidance, address any concerns, and make adjustments if necessary.
Factors Influencing Medication’s Impact on Nightmares

Several factors can influence the impact of medication on nightmares. Understanding these factors can help individuals manage their medication and its effects on their dream patterns more effectively.
1. Dosage and Timing: The dosage and timing of medication can play a significant role in its impact on nightmares. Adjustments in dosage or changing the time of administration can potentially influence dream patterns and the occurrence of nightmares.
2. Individual Variation: Each person may respond differently to medication, including its effects on dreaming. Some individuals may experience a decrease in nightmares, while others may still experience them despite medication. It’s important to recognize that individual variation exists and to communicate any concerns or changes in dream patterns to a healthcare provider.
3. Interaction with Other Medications: If an individual is taking multiple medications, there is a possibility of drug interactions that could affect dream patterns. It’s essential to inform healthcare providers about all medications being taken to ensure a comprehensive understanding of potential interactions.
By considering these factors, individuals can work closely with healthcare providers to find the most suitable medication regimen and manage any changes in dream patterns effectively.
1. Dosage and Timing
When it comes to the impact of medication on nightmares, the dosage and timing of the medication play a significant role. Let’s explore how these factors can influence the relationship between medication and nightmares:
- Dosage: The dosage of medication can directly affect its impact on nightmares. In some cases, a higher dosage may lead to a greater reduction in nightmare frequency and intensity. However, it’s important to strike a balance as excessively high dosages may lead to unwanted side effects. Healthcare providers carefully consider the optimal dosage based on individual needs and monitor its effectiveness over time.
- Timing: The timing of medication intake is another crucial factor to consider. Some medications, such as those that suppress REM sleep, may be more effective when taken in the evening or close to bedtime. This strategic timing can potentially reduce the occurrence of nightmares during the night. However, for medications that have a stimulating effect, it might be advisable to take them earlier in the day to minimize disruption to the sleep cycle. Healthcare providers can provide specific guidance on the best timing for medication intake based on individual circumstances.
It is vital to follow the prescribed dosage and timing instructions provided by healthcare professionals. They have the expertise to determine the appropriate dosing and timing to maximize the therapeutic benefits of the medication while minimizing the potential impact on nightmares. Communication with healthcare providers is essential to ensure proper management and adjustment of medication as needed.
2. Individual Variation
Individual variation plays a significant role in how medication affects the frequency and intensity of nightmares. Each person’s response to medication can vary, making it crucial to recognize that what works for one individual may not work for another. Factors such as metabolism, genetic predispositions, and overall health can influence how medication interacts with the body’s systems.
One individual may experience a reduction in nightmares and find relief from intense dreams while taking a specific medication, while another individual may have no noticeable change or even an increase in nightmares. This variation can be attributed to differences in brain chemistry and how the medication interacts with individual neurotransmitters.
It’s important to communicate openly with healthcare providers about any changes in nightmare frequency or intensity while taking medication. They can adjust dosages, switch medications, or explore alternative treatments based on an individual’s unique response.
Additionally, personal circumstances such as stress levels, traumatic experiences, and other mental health conditions can affect how medication impacts nightmares. Some individuals may find that medication alone does not completely resolve their nightmares and that additional therapies, such as cognitive-behavioral therapy or relaxation techniques, may be necessary to manage their dreams effectively.
Understanding individual variation is crucial in the treatment of nightmares and ensures that healthcare providers can tailor treatment plans to meet the specific needs of each person. By recognizing and addressing individual differences, it is possible to find the most effective approach to managing nightmares while on medication.
3. Interaction with Other Medications
Interaction with other medications is an important consideration when it comes to the effects of medication on nightmares. It’s essential to understand how different medications may interact and potentially impact dream patterns.
When multiple medications are taken together, there is a possibility of drug-drug interactions. Some medications may enhance or negate the effects of others, leading to an altered response in dream content or frequency. For example, certain medications used for treating anxiety or insomnia, such as benzodiazepines, may have sedative effects that can suppress dream activity. On the other hand, medications like stimulants or certain antidepressants may increase dream activity or intensity.
Medications can interact with substances like alcohol or recreational drugs, which can further influence dream patterns. It’s crucial to discuss all medications, including over-the-counter drugs and supplements, with a healthcare provider to ensure there are no potential negative interactions that may affect sleep and dreams.
In addition to medication interactions, it’s important to consider the potential impact of medication on underlying health conditions. Some medications used for physical health conditions, such as beta blockers or corticosteroids, may indirectly affect dreaming by managing symptoms or altering physiological processes. Understanding the comprehensive effects of all medications and their potential interactions is essential for individuals looking to manage nightmares effectively.
Managing Nightmares while on Medication
When experiencing nightmares while on medication, there are various strategies and approaches that can help manage and alleviate these distressing dreams. Communication with your healthcare provider is essential. They can adjust the dosage, timing, or even switch medications if necessary. It’s crucial to share any changes or concerns regarding your dreams with them for effective management. Additionally, adjunctive therapies such as cognitive behavioral therapy (CBT) or eye movement desensitization and reprocessing (EMDR) can be valuable in addressing the underlying causes of nightmares. These therapies can help identify triggers, develop coping mechanisms, and promote better sleep hygiene. Psychoeducation is also important, as it provides individuals with knowledge about nightmares and medication effects, helping to reduce anxiety and enhance understanding. By working closely with healthcare providers and incorporating effective strategies, nightmares on medication can be effectively managed, allowing for improved sleep and overall well-being.
1. Communication with Healthcare Provider
When dealing with nightmares while on medication, communication with your healthcare provider is paramount. Here are some important points to consider regarding this crucial aspect:
– Open and Honest Discussion: It is important to have an open and honest conversation with your healthcare provider about your experiences with nightmares. Share any changes in the frequency or intensity of your nightmares since starting medication. This information will help your provider assess the effectiveness of the medication and make any necessary adjustments.
– Medication Review: Your healthcare provider may need to review your current medication regimen to determine if any adjustments need to be made. They may consider changing the dosage, switching medications, or adding adjunctive therapies to better manage your nightmares. Regular check-ins and follow-up appointments are essential to monitor progress and address any concerns.
– Reporting Side Effects: If you experience any unwanted side effects, such as increased nightmares or other sleep disturbances, it is important to report them to your healthcare provider promptly. They can evaluate whether the side effects are related to the medication and recommend alternative options or provide strategies to mitigate the effects on your sleep.
– Exploring Alternative Treatments: Depending on the severity of your nightmares and the impact on your overall well-being, your healthcare provider may suggest additional treatments alongside medication. These may include therapy, such as cognitive-behavioral therapy for nightmares (CBT-I), which can be highly effective in managing nightmare frequency and intensity.
By maintaining open lines of communication with your healthcare provider, you can work together to find the most effective solutions for your specific needs. Remember to follow their guidance and never make changes to your medication regimen without consulting them first.
2. Adjunctive Therapies
2. Adjunctive Therapies: Adjunctive therapies refer to additional treatments or interventions that are used alongside medication to manage nightmares. These therapies can be beneficial in enhancing the effectiveness of medication and improving overall sleep quality. Here are some adjunctive therapies that have shown promise in managing nightmares:
- Cognitive-Behavioral Therapy for Insomnia (CBT-I): CBT-I is a type of therapy specifically designed to address sleep problems. It focuses on identifying and changing negative thought patterns and behaviors that contribute to sleep difficulties. CBT-I can help individuals develop healthier sleep habits and reduce the incidence of nightmares.
- Imagery Rehearsal Therapy (IRT): IRT involves rewriting the script of a recurring nightmare and practicing the revised dream scenario while awake. This technique aims to create positive associations with previously distressing dream content and reduce the occurrence of nightmares.
- Relaxation Techniques: Engaging in relaxation techniques such as deep breathing exercises, progressive muscle relaxation, or mindfulness meditation can help reduce overall stress levels and promote a more peaceful sleep. These techniques can be particularly helpful for individuals who experience nightmares related to anxiety or trauma.
- Hypnosis: Hypnosis can be utilized as an adjunctive therapy to address nightmare symptoms. Under the guidance of a trained professional, individuals can explore the underlying causes of their nightmares and learn relaxation techniques to modify dream content.
- Eye Movement Desensitization and Reprocessing (EMDR): EMDR is an evidence-based therapy primarily used for treating post-traumatic stress disorder (PTSD). It involves bilateral stimulation while individuals focus on traumatic memories, which can help reprocess the distress associated with these experiences and potentially reduce trauma-related nightmares.
It’s important to note that adjunctive therapies should be implemented under the guidance of a qualified healthcare professional or therapist. They can tailor these interventions to individual needs and circumstances to ensure optimal results. Combining medication with adjunctive therapies can provide a comprehensive approach to managing nightmares and improving overall sleep quality.
3. Psychoeducation
Psychoeducation is a valuable approach in managing nightmares while on medication. It involves educating individuals about the causes, symptoms, and treatment options for nightmares and related sleep disorders. Psychoeducation aims to empower individuals by providing them with knowledge and understanding about their condition. This knowledge can help individuals make informed decisions about their treatment and develop effective coping strategies. During psychoeducation sessions, individuals may learn about the impact of medication on their nightmares, including the potential benefits and side effects. They may also learn about additional strategies they can incorporate alongside medication, such as relaxation techniques, imagery rehearsal therapy, or keeping a dream journal. Psychoeducation sessions can be conducted with healthcare providers, psychologists, or through support groups, providing individuals with a supportive environment to ask questions and share experiences. By receiving psychoeducation, individuals can gain a better understanding of their nightmares, feel more in control of their treatment, and enhance their overall well-being.
Conclusion
In conclusion, medication can have a significant impact on the frequency and intensity of nightmares. Different types of medication, such as antidepressants, antipsychotics, and anxiety medication, can affect dream patterns in various ways. While some medications may suppress REM sleep, others can alter dream content or patterns. Overall, medication can decrease the frequency of nightmares and reduce their intensity. However, it’s important to note that the impact of medication on nightmares can vary from person to person. Factors such as dosage, timing, individual variation, and potential interactions with other medications can influence the medication’s effectiveness in managing nightmares. It is crucial to communicate openly with healthcare providers and discuss any concerns or side effects related to nightmares and medication. In addition to medication, adjunctive therapies and psychoeducation can also play a valuable role in managing nightmares. By taking a comprehensive approach, individuals can work towards minimizing the negative impact of nightmares on their overall well-being.
Frequently Asked Questions
1. Can medication completely eliminate nightmares?
While medication can help reduce the frequency and intensity of nightmares, it may not completely eliminate them. The effectiveness of medication varies from person to person, and some individuals may still experience occasional nightmares despite treatment.
2. Can medication cause unusual or vivid dreams?
Yes, some medications can cause unusual or vivid dreams as a side effect. These dreams may be more vivid, vividly remembered, or have unusual content. It’s important to discuss any changes in dream patterns with your healthcare provider.
3. Do all medications have the same impact on nightmares?
No, different medications can have varying effects on nightmares. Antidepressants may suppress REM sleep, while antipsychotics and anxiety medications can alter dream content. It’s important to consult with a healthcare provider to understand how specific medications may affect your nightmares.
4. Can the dosage and timing of medication impact nightmares?
Yes, the dosage and timing of medication can impact nightmares. Adjusting the dosage or taking medication at different times may help manage nightmares more effectively. However, it’s crucial to consult with a healthcare provider before making any changes to your medication regimen.
5. Are there any natural alternatives to medication for managing nightmares?
Yes, there are natural alternatives that may help manage nightmares. Techniques such as relaxation exercises, cognitive-behavioral therapy for sleep, and keeping a dream journal can be effective in reducing nightmares. It’s best to discuss these options with a healthcare provider or therapist.
6. Can medication for other conditions affect nightmares?
Yes, medication for other conditions can potentially impact nightmares. Medications used to treat conditions like hypertension, allergies, or Parkinson’s disease may have side effects that affect dream patterns. Discuss any changes in dream patterns with your healthcare provider.
7. Are nightmares associated with specific types of medication?
Nightmares can be associated with certain types of medication, such as antidepressants or antipsychotics. However, it’s important to note that not everyone taking these medications will experience nightmares. The relationship between specific medications and nightmares can vary.
8. Can medication change the content of nightmares?
Yes, medication can potentially change the content of nightmares. Antidepressants and antipsychotics may alter dream content by influencing neurotransmitters and brain activity during sleep. However, each person may respond differently to these medications.
9. Can combining medications increase the risk of nightmares?
Combining certain medications can potentially increase the risk of nightmares. Some interactions between medications may affect sleep quality and dream patterns. It’s important to inform your healthcare provider about all the medications you are taking to monitor for any potential interactions.
10. Can therapy be used alongside medication to manage nightmares?
Yes, therapy can be used alongside medication as a holistic approach to managing nightmares. Therapies like cognitive-behavioral therapy for nightmares (CBT-N) can complement medication by addressing underlying psychological factors contributing to nightmares. It’s recommended to discuss therapy options with a qualified mental health professional.