Restless Leg Syndrome (RLS) is a perplexing condition that affects millions of people worldwide. Despite its prevalence, there are several common misconceptions about RLS that often lead to confusion and misunderstanding. In this article, we will debunk these myths and shed light on the true nature of RLS. So, if you’ve ever wondered about the causes, symptoms, and treatments of this puzzling syndrome, keep reading to uncover the truth behind the misconceptions.
What is Restless Leg Syndrome?

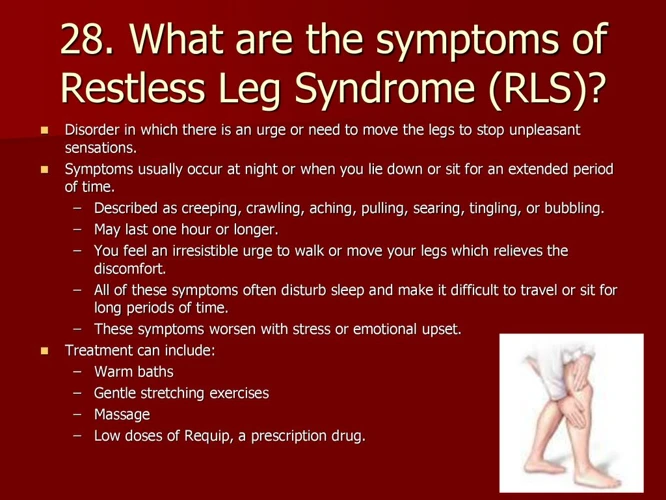
Restless Leg Syndrome, also known as Willis-Ekbom Disease, is a neurological disorder characterized by an irresistible urge to move the legs, often accompanied by uncomfortable sensations. This condition typically occurs during periods of rest or inactivity, especially in the evening or at night, making it difficult for individuals to relax and fall asleep (source).
The sensations experienced by people with RLS can vary but are often described as throbbing, itching, crawling, or tingling. These sensations can be temporarily relieved by movement, such as stretching or walking, but the relief is usually only temporary. The severity of symptoms can range from mild to severe and can fluctuate over time.
It is estimated that around 7-10% of the population is affected by RLS, with women being more prone to developing the condition than men. While the exact cause of RLS is not fully understood, it is believed to involve a combination of genetic and environmental factors. Certain medical conditions, such as iron deficiency, kidney disease, and peripheral neuropathy, have also been linked to the development of RLS.
Although RLS primarily affects the legs, it can also manifest in other parts of the body, such as the arms. In some cases, individuals may experience RLS symptoms during their waking hours, leading to distress and interruption of daily activities. This condition can also impact sleep quality, leading to daytime fatigue and excessive daytime sleepiness.
In the next sections of this article, we will address some common misconceptions about Restless Leg Syndrome and provide evidence-based information to better understand this perplexing condition.
Myth #1: Restless Leg Syndrome is just a normal case of leg cramps
Myth #1: Restless Leg Syndrome is just a normal case of leg cramps.
This is a common misconception regarding Restless Leg Syndrome (RLS). While leg cramps can cause discomfort in the legs, RLS is a distinct neurological disorder with specific characteristics. Leg cramps typically involve sudden and involuntary muscle contractions, often occurring during sleep or after intense exercise. On the other hand, RLS is characterized by an urge to move the legs and uncomfortable sensations, such as tingling or crawling, that are relieved by movement. The sensations experienced in RLS can be described as different from the pain associated with leg cramps.
Leg cramps tend to be more short-lived and can usually be alleviated through stretching and massage, while RLS symptoms persist for a longer duration and are not easily relieved. RLS commonly occurs during periods of rest or inactivity, particularly in the evening or at night, and can significantly disrupt sleep patterns. It is important to differentiate between these two conditions to ensure appropriate management and treatment options are pursued.
In the next section, we will explore another common myth about Restless Leg Syndrome, namely that it only affects older individuals.
Explanation of the misconception and why it is incorrect
Explanation of the misconception: Restless Leg Syndrome is just a normal case of leg cramps.
Leg cramps and Restless Leg Syndrome are often mistaken as the same condition, leading to the misconception that RLS is just a normal case of leg cramps. However, this is far from the truth. Leg cramps are sudden, painful contractions of the muscles, usually occurring during periods of rest or at night. On the other hand, RLS is characterized by uncomfortable sensations in the legs, accompanied by an irresistible urge to move them.
Why it is incorrect:
1. Sensations: Unlike leg cramps, which primarily cause muscle pain, RLS is associated with various sensations such as tingling, itching, or crawling. These distinct sensations are not typically experienced during leg cramps.
2. Urge to Move: People with RLS feel an overwhelming need to move their legs to alleviate the uncomfortable sensations. This urge is not present in leg cramps.
3. Movement Relief: Unlike leg cramps, where movement may worsen the pain, moving the legs can provide temporary relief from the uncomfortable sensations associated with RLS.
4. Impact on Sleep: Leg cramps may disrupt sleep, but RLS can significantly impact sleep quality and lead to insomnia, as individuals constantly feel the need to move their legs, making it difficult to find restful sleep (source).
It is essential to differentiate between leg cramps and Restless Leg Syndrome, as the underlying causes and management approaches differ. Leg cramps are often due to muscle strain or dehydration, while RLS has neurological origins. If you suspect you may have RLS, it is crucial to consult a healthcare professional for an accurate diagnosis and appropriate treatment strategies, including practical tips for managing RLS at night (source).
Myth #2: Restless Leg Syndrome only affects older individuals
Restless Leg Syndrome (RLS) is often mistakenly believed to only affect older individuals. However, this is a common misconception. While it is true that RLS prevalence does increase with age, it can affect individuals of all age groups, from children to the elderly.
In fact, research has shown that RLS can start in childhood or adolescence. A study published in the Journal of Pediatric Neurology found that RLS symptoms were present in approximately 2% of children aged 8-17 years. Another study published in the journal Sleep Medicine reported that RLS prevalence among teenagers ranged from 2.4% to 6.5%.
RLS can also affect pregnant women. It is estimated that up to 26% of pregnant women experience RLS symptoms, particularly during the third trimester. The hormonal changes and increased blood volume during pregnancy are believed to contribute to the development or worsening of RLS symptoms.
While it is true that the prevalence of RLS does increase with age, with the highest rates observed in individuals over 65 years old, it is important to recognize that RLS can affect individuals of all age groups. Understanding and recognizing the symptoms of RLS in younger individuals is crucial for proper diagnosis and management of the condition.
Explanation of the misconception and statistics about different age groups affected by RLS
One common misconception about Restless Leg Syndrome (RLS) is that it only affects older individuals. This misconception may stem from the fact that RLS symptoms tend to worsen with age, but it is important to understand that RLS can affect individuals of all age groups.
Statistics show that RLS affects both children and adults. In children, RLS has been estimated to affect around 1-5% of the population, with symptoms often starting before the age of ten. Children with RLS may experience difficulty sleeping and may exhibit symptoms such as leg movements during sleep and daytime drowsiness.
In adults, the prevalence of RLS increases with age. Research suggests that around 2-3% of adults experience RLS symptoms, with the prevalence being higher in women than men. The exact reasons for these gender differences are still being studied.
It is important to note that RLS can have a significant impact on quality of life, regardless of age. The symptoms can disrupt sleep, interfere with daily activities, and lead to increased fatigue and reduced productivity. It is crucial to recognize that RLS is not limited to older individuals and can affect individuals of all ages.
Myth #3: Restless Leg Syndrome is caused by poor circulation
A common misconception about Restless Leg Syndrome (RLS) is that it is caused by poor circulation. However, this belief is inaccurate. While poor circulation can contribute to various health issues, RLS has distinct underlying factors that are not solely related to blood flow.
RLS is primarily a neurological disorder, not a circulatory one. Research suggests that the main contributing factor for RLS is an imbalance of dopamine, a neurotransmitter in the brain that plays a crucial role in controlling movement and sensations. This imbalance disrupts the normal functioning of the basal ganglia, a region of the brain responsible for regulating muscle activity.
Other factors that can trigger or worsen RLS symptoms include certain medications (such as antihistamines and antidepressants), pregnancy, iron deficiency, kidney dysfunction, and certain chronic conditions like diabetes and Parkinson’s disease. However, poor circulation alone is not the root cause of RLS.
It is important to note that while poor circulation is not the direct cause of RLS, it can exacerbate symptoms. When blood flow to the legs is compromised, it can lead to discomfort and leg sensations that are similar to those experienced with RLS. However, addressing circulation issues alone will not resolve RLS symptoms. It is crucial to identify and address the underlying neurological factors, such as dopamine imbalance and other contributing factors specific to each individual.
In the next section, we will delve deeper into the neurological origins of RLS and explore the scientific evidence supporting this understanding.
Explanation of the misconception and the actual factors contributing to RLS
The misconception surrounding Restless Leg Syndrome is that it is caused by poor circulation. However, this is not entirely accurate. While circulation issues can contribute to the symptoms of RLS, they are not the sole cause.
RLS is believed to have a multifactorial origin, involving a combination of genetic, environmental, and neurological factors. It has been found that individuals with a family history of RLS are more likely to develop the condition, suggesting a genetic component.
Another important factor contributing to RLS is an imbalance in dopamine, a neurotransmitter in the brain. Dopamine plays a vital role in controlling movement and muscle activity. Low levels of dopamine or dysfunction in the dopamine receptors have been associated with the development of RLS.
Iron deficiency is also known to contribute to RLS. Iron is involved in the production of dopamine, and low iron levels can disrupt dopamine function. Addressing iron deficiency through supplementation or dietary changes may help alleviate RLS symptoms in some individuals.
Certain medical conditions, such as kidney disease, diabetes, and peripheral neuropathy, have also been linked to RLS. These conditions can affect the nerves and disrupt the signaling between the brain and legs, leading to the development of RLS symptoms.
Additionally, certain medications, including antihistamines and antidepressants, have been found to exacerbate RLS symptoms. It is important to consult with a healthcare professional to evaluate the potential impact of medications on RLS.
While circulation issues can play a role in Restless Leg Syndrome, they are not the sole cause. RLS is a complex disorder with multiple contributing factors, including genetic predisposition, dopamine imbalance, iron deficiency, and underlying medical conditions. Understanding these actual factors can help individuals and healthcare providers develop more effective strategies for managing and treating RLS.
Myth #4: Restless Leg Syndrome is a psychological condition

The misconception that Restless Leg Syndrome is a psychological condition is quite common but is not supported by scientific evidence. RLS is a neurological disorder that involves the malfunctioning of certain parts of the brain that control movement and sensory processing. It is not solely caused by psychological factors or symptoms of anxiety or depression.
Research has shown that there are specific abnormalities in the dopamine system of individuals with RLS. Dopamine is a neurotransmitter that plays a crucial role in regulating movement and sensory perception. Changes in dopamine levels or sensitivity in the brain can contribute to the development and severity of RLS symptoms.
Studies have identified genetic factors that are involved in the development of RLS. Mutations or variations in certain genes that regulate iron transport and metabolism, dopamine regulation, and neuronal development have been linked to an increased risk of RLS.
It is important to note that while RLS is not a psychological condition, it can have a significant impact on an individual’s mental well-being. The discomfort, sleep disturbances, and daily challenges posed by RLS can contribute to feelings of frustration, anxiety, and depression. A comprehensive approach to managing RLS should address both the neurological aspects of the condition and the psychological impact it may have on individuals.
In the following sections, we will delve further into the misconceptions surrounding RLS and provide more accurate information regarding its causes, treatment options, and impact on daily life.
Explanation of the misconception and scientific evidence supporting the neurological origins of RLS
The misconception surrounding Restless Leg Syndrome (RLS) is that it is a purely psychological condition. However, scientific evidence strongly supports the neurological origins of RLS. RLS is not caused by a psychological disorder or imagined sensations, but rather by abnormalities in the central nervous system.
Studies have shown that individuals with RLS have alterations in the levels of certain neurotransmitters, including dopamine. Dopamine is a chemical messenger in the brain that plays a crucial role in regulating movement and motor control. It is believed that dysfunction in the dopamine pathways contributes to the development of RLS (source).
Brain imaging studies have revealed specific patterns of brain activity in individuals with RLS. These findings provide further support for the neurological basis of the condition. The regions of the brain involved in motor control and sensory processing show abnormal activity in individuals with RLS, particularly during periods of rest or inactivity.
Additionally, genetic factors have been identified as playing a significant role in the development of RLS. Several genetic variants have been linked to an increased risk of RLS, further highlighting its neurological basis. These genetic factors may influence the functioning of specific neurotransmitter systems in the brain, contributing to the development of RLS.
The scientific evidence strongly refutes the misconception that RLS is a psychological condition. It is a real and often debilitating neurological disorder, impacting the lives of millions of individuals worldwide. Understanding the neurological origins of RLS is essential in improving diagnosis, treatment, and management strategies for this condition.
Myth #5: Restless Leg Syndrome can be cured with over-the-counter pain medications
Myth #5: Restless Leg Syndrome can be cured with over-the-counter pain medications
One common misconception about Restless Leg Syndrome is that it can be cured or effectively managed with over-the-counter pain medications. While these medications may temporarily alleviate some of the discomfort associated with RLS, they do not target the underlying causes of the condition.
Restless Leg Syndrome is a complex disorder with various contributing factors, including dopamine imbalance, iron deficiency, and genetic predisposition. Over-the-counter pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or analgesics, are not specifically designed to address these underlying causes. They may provide temporary relief by reducing pain and inflammation, but they do not target the neurological or physiological aspects of RLS.
Proper management of Restless Leg Syndrome involves a comprehensive approach that includes lifestyle changes, addressing underlying conditions, and, in some cases, medication prescribed by a healthcare professional. Iron supplements may be recommended for individuals with iron deficiency-related RLS, while dopamine agonist medications may be prescribed to help regulate dopamine levels in the brain.
It is crucial to consult a healthcare professional for an accurate diagnosis and appropriate treatment plan tailored to individual needs. Self-medication with over-the-counter pain medications may mask the symptoms temporarily but does not provide a long-term solution for managing RLS.
In addition to medication, there are various self-care strategies that can help manage Restless Leg Syndrome symptoms. These include practicing good sleep hygiene, such as sticking to a regular sleep schedule and creating a relaxing bedtime routine. Regular exercise, stress management techniques, and avoiding triggers like caffeine and nicotine can also alleviate symptoms and improve quality of life for individuals with RLS.
By debunking the myth that over-the-counter pain medications can cure RLS, we hope to emphasize the importance of seeking proper diagnosis and treatment under the guidance of a healthcare professional. Each individual’s experience with RLS may differ, and a personalized approach is necessary to effectively manage the condition and minimize its impact on daily life.
Explanation of the misconception and the importance of proper diagnosis and treatment options
Many people mistakenly believe that Restless Leg Syndrome (RLS) can be cured with over-the-counter pain medications or by simply disregarding the symptoms. However, this is a misconception that can lead to ineffective treatment and unnecessary suffering.
Proper diagnosis is crucial for individuals experiencing RLS symptoms. It is important to consult with a healthcare professional who specializes in sleep disorders or neurology to accurately diagnose RLS. This involves a comprehensive evaluation of the individual’s medical history, a thorough physical examination, and potentially additional tests to rule out other underlying conditions.
Once a diagnosis of RLS is confirmed, appropriate treatment options can be explored. The goal of treatment is to manage and alleviate the symptoms, improve sleep quality, and enhance overall quality of life. It is important to note that treatment plans may vary depending on the individual and the severity of their symptoms.
Different treatment options for RLS include lifestyle changes, such as adopting a regular sleep schedule, incorporating moderate exercise into daily routine, and implementing relaxation techniques. Medications may also be prescribed to manage symptoms and improve sleep. These may include dopaminergic agents, opioids, anticonvulsants, or iron supplements (if iron deficiency is detected).
In some cases, individuals may benefit from alternative therapies such as acupuncture, massage, or physical therapy. These complementary approaches can provide additional support and symptom relief.
It is essential to emphasize the importance of working closely with a healthcare professional to find the most suitable treatment plan. Every individual with RLS has unique needs, and a tailored approach is essential for effective management. Regular follow-up appointments should be scheduled to assess the treatment’s effectiveness and make any necessary adjustments.
Proper diagnosis and individualized treatment plans can significantly improve the quality of life for individuals living with Restless Leg Syndrome. It is important to avoid self-diagnosis and self-medication, as these can lead to ineffective treatment and potential complications. Seeking professional guidance ensures that appropriate treatments are implemented, providing the best chance for symptom relief and improved well-being.
Myth #6: Restless Leg Syndrome is not a serious medical condition
Myth #6: Restless Leg Syndrome is not a serious medical condition.
Contrary to popular belief, Restless Leg Syndrome (RLS) is indeed a serious medical condition that can significantly impact an individual’s quality of life. While it may not be life-threatening, the symptoms of RLS can be highly disruptive and detrimental to physical and mental well-being.
One of the primary ways in which RLS affects individuals is by interfering with sleep patterns. The discomfort and urge to move the legs can make it extremely challenging to fall asleep or stay asleep throughout the night. The resulting sleep deprivation can lead to daytime fatigue, irritability, and difficulty in focusing on daily tasks. In severe cases, it can even lead to insomnia and contribute to the development or worsening of mental health conditions, such as depression and anxiety.
The impact of RLS extends beyond sleep disturbances. The constant discomfort and restlessness often affect an individual’s ability to sit or lie down for extended periods, making it difficult to engage in activities that require prolonged periods of stillness, such as long car rides, flights, or movie theater outings. This can lead to social isolation and reduced participation in social and recreational activities.
Additionally, the symptoms of RLS can lead to significant distress and frustration, as they are often unpredictable and can vary in severity. The persistent discomfort and the disruption it causes in daily life can result in increased levels of stress, anxiety, and even depression. It is essential to recognize that RLS is not a trivial complaint but a genuine medical condition that can have a profound impact on an individual’s overall well-being. Seeking medical assistance and appropriate treatment is crucial to managing the symptoms and improving quality of life for those affected by RLS.
In the next section, we will discuss the different treatment options available for Restless Leg Syndrome, highlighting the importance of proper diagnosis and management strategies.
Explanation of the misconception and the impact of RLS on quality of life
The misconception that Restless Leg Syndrome (RLS) is not a serious medical condition can have a significant impact on the lives of those affected by it. RLS is often misunderstood and brushed off as a minor inconvenience, but the truth is that it can have a profound effect on a person’s quality of life.
One of the primary ways RLS impairs quality of life is through its impact on sleep. Many individuals with RLS experience difficulty falling asleep or staying asleep due to the uncomfortable sensations and urge to move their legs. This can lead to chronic sleep deprivation, daytime fatigue, and decreased cognitive function. In severe cases, it can even contribute to conditions like depression and anxiety.
The impact of RLS on quality of life extends beyond just sleep disturbances. The constant urge to move the legs can make it challenging to engage in activities that require sitting or remaining still for extended periods, such as attending movies, concerts, or long flights. It can also disrupt social interactions, as individuals with RLS may feel restless, agitated, or unable to relax during social gatherings or intimate moments.
The emotional toll of RLS should not be underestimated either. Dealing with the persistent discomfort and frustration can lead to increased stress, irritability, and a reduced sense of well-being. The lack of understanding or empathy from others who may not recognize the seriousness of the condition can further exacerbate these emotional challenges.
It is important to acknowledge that RLS is a legitimate medical condition that can significantly impact an individual’s quality of life. Seeking proper diagnosis and treatment from healthcare professionals experienced in the management of RLS is crucial in alleviating symptoms and improving overall well-being. In the next sections, we will debunk more misconceptions about RLS and explore the factors contributing to its development and effective treatment options.
Conclusion
In conclusion, it is important to debunk the common misconceptions surrounding Restless Leg Syndrome (RLS) in order to gain a better understanding of this neurological disorder. RLS is not merely a normal case of leg cramps, nor is it limited to older individuals. It is not caused by poor circulation or solely a psychological condition. Over-the-counter pain medications cannot cure RLS, and it should not be dismissed as a non-serious medical condition.
RLS has a significant impact on the quality of life, affecting sleep, daily activities, and overall well-being. Proper diagnosis and treatment options are crucial for managing RLS effectively. Seeking medical advice, addressing underlying conditions, and adopting lifestyle changes can greatly alleviate symptoms and improve the quality of life for individuals with RLS.
It is important to educate ourselves and others about the realities of Restless Leg Syndrome, debunking the misconceptions and fostering a supportive environment for those living with this perplexing condition. By spreading accurate information, we can promote understanding and empathy, and ensure that individuals with RLS receive the support and treatment they need.
Frequently Asked Questions
Q: Can Restless Leg Syndrome occur during the day?
A: Yes, although RLS symptoms are commonly experienced during periods of rest or inactivity, some individuals may also experience symptoms during the day.
Q: What are the common triggers for Restless Leg Syndrome?
A: While triggers can vary between individuals, some common triggers for RLS include stress, fatigue, caffeine, and certain medications.
Q: Is Restless Leg Syndrome a hereditary condition?
A: There is evidence to suggest that genetics play a role in the development of Restless Leg Syndrome, with approximately 50% of individuals having a family history of the condition.
Q: Can Restless Leg Syndrome be worsened by certain medications?
A: Yes, certain medications such as antidepressants, antipsychotics, and antihistamines can worsen symptoms of Restless Leg Syndrome.
Q: Does Restless Leg Syndrome only affect the legs?
A: While the legs are the most commonly affected area, Restless Leg Syndrome can also manifest in other parts of the body, including the arms.
Q: How is Restless Leg Syndrome diagnosed?
A: A diagnosis of Restless Leg Syndrome is typically based on a clinical evaluation of symptoms, medical history, and sometimes additional tests to rule out other underlying conditions.
Q: Can lifestyle changes help manage Restless Leg Syndrome?
A: Yes, making certain lifestyle changes such as regular exercise, practicing good sleep hygiene, and avoiding triggers like caffeine and alcohol can help manage symptoms of Restless Leg Syndrome.
Q: Are there any specific medications available to treat Restless Leg Syndrome?
A: Yes, there are various medications available that can help alleviate the symptoms of Restless Leg Syndrome. These include dopamine agonists, opioids, and anticonvulsants, among others.
Q: Can Restless Leg Syndrome improve spontaneously?
A: While some individuals may experience periods of remission or improvement in symptoms, Restless Leg Syndrome is a chronic condition that typically requires ongoing management.