Sleep apnea affects millions of people worldwide, yet it remains a poorly understood and underdiagnosed condition. It can have a significant impact on a person’s quality of life, causing chronic fatigue, impaired cognitive function, and even increasing the risk of heart disease. In this comprehensive article, we will delve into the causes, symptoms, and treatments of sleep apnea. Whether you suspect you may have sleep apnea or you are seeking to educate yourself on this condition, this article will provide you with a thorough understanding of sleep apnea and empower you to take control of your health and well-being.
What is Sleep Apnea?
Sleep apnea is a sleep disorder characterized by repeated pauses in breathing during sleep. These pauses, known as apneas, can last for several seconds to minutes and can occur multiple times throughout the night. During these episodes, the brain and the rest of the body may not receive sufficient oxygen, leading to disrupted sleep patterns and various health complications. Sleep apnea is often accompanied by loud snoring, gasping, or choking sounds as the individual attempts to resume breathing. Interestingly, individuals with sleep apnea may also experience alterations in their dreaming patterns, including a decrease in REM sleep duration and a reduction in dream recall. Understanding the nature of sleep apnea is crucial in order to address its potential health consequences and improve overall sleep quality.
The Definition of Sleep Apnea
Sleep apnea is a sleep disorder characterized by recurrent interruptions in breathing during sleep. These interruptions, known as apneas, can last for a few seconds to a few minutes and can occur multiple times throughout the night. The word “apnea” itself means “without breath” in Greek. These pauses in breathing can be caused by the relaxation and collapse of the throat muscles, which obstruct the airway and hinder the flow of oxygen. As a result, the brain and the body do not receive sufficient oxygen, leading to fragmented sleep and various symptoms. Sleep apnea is typically accompanied by loud snoring, gasping, or choking sounds as the individual struggles to resume breathing. It is important to note that sleep apnea can have different forms, including obstructive sleep apnea (OSA), central sleep apnea (CSA), and complex sleep apnea syndrome (CSAS). OSA is the most common type, accounting for approximately 84% of all sleep apnea cases. Understanding the definition of sleep apnea is crucial in recognizing the signs and symptoms of this condition and seeking appropriate diagnosis and treatment. For more information on how sleep apnea can impact dreaming patterns, you can read our article on sleep apnea and REM sleep here.
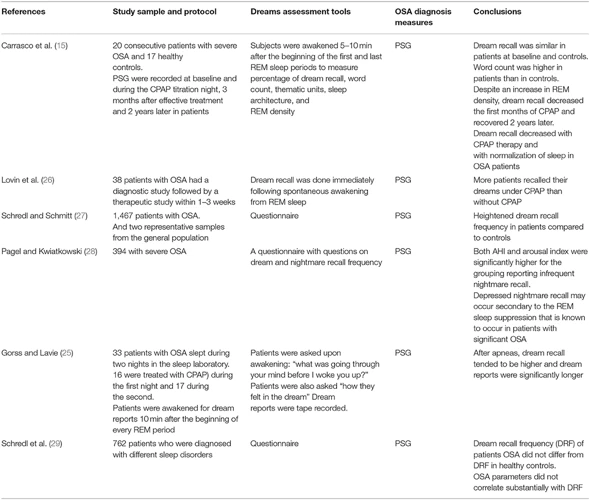
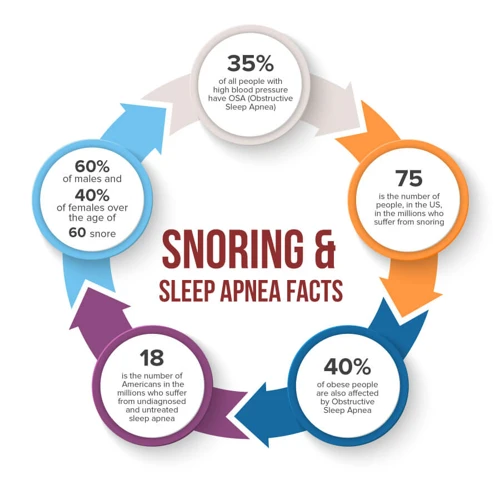
The Prevalence of Sleep Apnea
The prevalence of sleep apnea is alarmingly high, affecting a significant portion of the population. According to studies, it is estimated that approximately 936 million individuals worldwide suffer from this sleep disorder. Sleep apnea can occur in people of all ages, although it is more commonly diagnosed in adults. It is believed that around 80% of cases remain undiagnosed, further highlighting the need for increased awareness and screening. Sleep apnea is more prevalent in certain populations, such as those who are overweight or obese, middle-aged and older adults, and individuals with certain medical conditions, such as hypertension or diabetes. Additionally, men are more likely to be affected by sleep apnea than women, although the risk in women tends to increase after menopause. The high prevalence of sleep apnea emphasizes the importance of education, early detection, and appropriate treatment to mitigate its adverse effects on individuals’ overall health and well-being.
Causes of Sleep Apnea

Sleep apnea can have several different causes, and each type of sleep apnea may have distinct underlying factors. The most common form of sleep apnea is obstructive sleep apnea (OSA), which occurs when the muscles in the back of the throat fail to keep the airway open. This can be caused by various factors, including obesity, excessive weight gain, enlarged tonsils or adenoids, and structural abnormalities of the jaw or airway. Central sleep apnea (CSA) occurs when the brain fails to send the proper signals to the muscles that control breathing. This can be a result of certain medical conditions, such as heart failure or stroke. Additionally, complex sleep apnea syndrome (CSAS) can develop in individuals who have a combination of obstructive and central sleep apnea. Understanding the causes of sleep apnea is vital in determining the appropriate treatment approach and addressing the root cause of the condition.
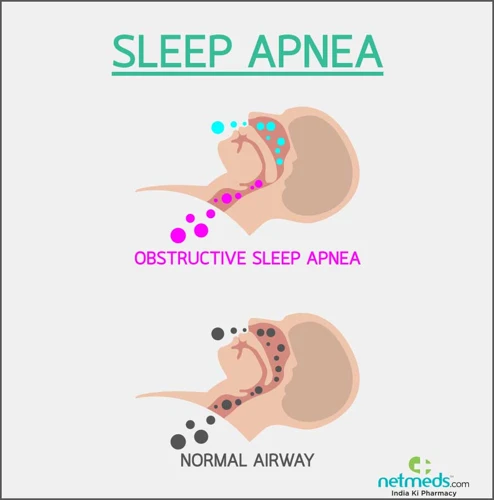
Obstructive Sleep Apnea (OSA)
Obstructive Sleep Apnea (OSA) is the most common form of sleep apnea and occurs when the upper airway becomes partially or completely blocked during sleep. This obstruction is often due to the relaxation of the muscles in the throat, tongue, and soft palate, which can result in a narrowing or complete closure of the airway. As a result, individuals with OSA may experience frequent disruptions in breathing, causing their oxygen levels to drop and arousals from sleep. These disruptions can be accompanied by loud, chronic snoring and gasping for air as the body tries to overcome the blockage and resume normal breathing. OSA can significantly impact sleep quality and lead to excessive daytime sleepiness, fatigue, and impaired cognitive function. It is also important to note that OSA can increase the risk of various health conditions such as hypertension, heart disease, and stroke. If left untreated, OSA can have serious consequences for overall health and well-being. It is crucial for individuals experiencing symptoms of OSA to seek diagnosis and appropriate treatment to improve their sleep and overall health.
Central Sleep Apnea (CSA)
Central Sleep Apnea (CSA) is a less common form of sleep apnea that is characterized by the brain’s inability to send proper signals to the muscles that control breathing during sleep. Unlike obstructive sleep apnea (OSA), CSA is not caused by a physical blockage in the airway. Instead, it is a result of a malfunction in the central nervous system. Some of the main causes of CSA include certain medical conditions, such as heart failure, stroke, or brainstem disorders. Additionally, the use of certain medications, such as opioids, can also contribute to the development of CSA. The symptoms of CSA overlap with those of OSA and may include excessive daytime sleepiness, morning headaches, restless sleep, and difficulty concentrating. Diagnosing CSA typically involves a sleep study called polysomnography, which monitors various bodily functions during sleep. Treatment options for CSA may vary depending on the underlying cause, but they often involve addressing the specific medical condition or adjusting medications. In some cases, the use of adaptive servo-ventilation (ASV), a type of positive airway pressure therapy, may be recommended to help regulate breathing during sleep. It is important to consult with a healthcare professional for proper diagnosis and treatment of CSA to improve sleep quality and overall well-being.
Complex Sleep Apnea Syndrome (CSAS)
Complex Sleep Apnea Syndrome (CSAS) is a less common form of sleep apnea that is sometimes referred to as treatment-emergent central sleep apnea (CSA). It is characterized by a combination of features seen in both obstructive sleep apnea (OSA) and central sleep apnea (CSA). Unlike OSA and CSA, which have distinct causes, CSAS occurs when a person with pre-existing OSA develops central breathing abnormalities after receiving treatment with continuous positive airway pressure (CPAP) therapy. This transition from OSA to CSAS typically happens within a few weeks or months of starting CPAP treatment. The exact underlying mechanisms responsible for CSAS are not yet fully understood, but it is believed to be related to a complex interplay between the upper airway and the central respiratory control centers in the brain. Individuals with CSAS may experience more severe symptoms compared to those with OSA or CSA alone, as it involves a combination of both obstructive and central breathing events during sleep. It is important for individuals who develop CSAS to undergo a comprehensive evaluation by a sleep specialist to determine the most appropriate treatment approach, which may include adjustments to CPAP settings or the consideration of alternative treatment options such as oral appliance therapy or surgery. Understanding the unique characteristics of CSAS can help healthcare professionals tailor treatment plans for individuals with this specific subtype of sleep apnea, ultimately improving their sleep quality and overall well-being.
Symptoms of Sleep Apnea

Sleep apnea can manifest through a range of symptoms that affect both the physical and mental well-being of individuals. Common symptoms of sleep apnea include persistent snoring, restless sleep, and abrupt awakenings accompanied by a choking or gasping sensation. Those affected may also experience excessive daytime sleepiness, morning headaches, and difficulty concentrating. Sleep apnea has been linked to an increased risk of high blood pressure, heart disease, and stroke. It is important to note that individuals with sleep apnea may experience alterations in their dreaming patterns, such as reduced dream recall. If you suspect you or someone you know may be experiencing symptoms of sleep apnea, it is essential to seek medical attention for a proper diagnosis and timely treatment.
General Symptoms of Sleep Apnea
General Symptoms of Sleep Apnea:
– Loud and Chronic Snoring: This is one of the most common symptoms of sleep apnea. The snoring is often loud, disruptive, and may even be accompanied by snorting or gasping sounds. It is important to note that not everyone who snores has sleep apnea, but it is a common indicator.
– Episodes of Breathing Cessation: Sleep apnea is characterized by repeated pauses in breathing during sleep. These episodes, known as apneas, can last for several seconds to minutes. They may be followed by a choking or gasping sensation as the individual tries to resume breathing.
– Excessive Daytime Sleepiness: People with sleep apnea often experience excessive daytime sleepiness even after seemingly getting a full night’s sleep. This persistent fatigue can significantly impact their ability to function during the day and may lead to difficulties concentrating, memory problems, and even an increased risk of accidents.
– Morning Headaches: Waking up with a headache is another common symptom of sleep apnea. These headaches are often described as a dull throbbing sensation and can be persistent throughout the day.
– Restless Sleep: Individuals with sleep apnea may have a restless sleep pattern, characterized by frequent awakenings, tossing and turning, or a feeling of not having a restful night’s sleep.
– Waking up with a Dry Mouth or Sore Throat: Due to the interrupted breathing patterns during sleep, individuals with sleep apnea may wake up with a dry mouth or a sore throat. This can be a result of mouth breathing and the airway becoming dry.
It is important to consult a healthcare professional if you experience these symptoms, as they can be indicative of sleep apnea or other sleep disorders. Proper diagnosis and treatment are essential for managing sleep apnea and improving overall sleep quality and daytime functioning.
Physical Symptoms
Physical symptoms associated with sleep apnea can manifest in various ways. It is essential to recognize these symptoms as they can offer clues to the presence of the condition. Some of the most common physical symptoms of sleep apnea include:
- Loud snoring: This is a hallmark symptom of sleep apnea and is often observed by bed partners. The snoring is often loud, persistent, and may be accompanied by gasping or choking sounds.
- Episodes of breath cessation: Sleep apnea causes pauses in breathing during sleep. These pauses can last for several seconds or longer and can occur numerous times throughout the night.
- Waking up with a sore or dry throat: Due to the disruptions in normal breathing patterns, individuals with sleep apnea may wake up with a dry or sore throat.
- Morning headaches: Frequent episodes of disrupted breathing during sleep can lead to morning headaches that may range from mild to severe in intensity.
- Excessive daytime sleepiness: Individuals with sleep apnea often experience excessive daytime sleepiness regardless of the amount of time spent in bed. Excessive sleepiness can impact daily functioning and increase the risk of accidents.
- Difficulty concentrating: Sleep apnea can impair cognitive function, leading to difficulties in concentration, memory problems, and decreased alertness.
- Decreased libido: Sleep apnea can contribute to a decrease in sexual desire and performance difficulties.
- Nighttime sweating: Some individuals with sleep apnea may experience excessive sweating during sleep, leading to damp or soaked sheets and clothing.
It is important to note that these physical symptoms may vary among individuals affected by sleep apnea. It is advisable to consult a healthcare professional for an accurate diagnosis and appropriate treatment. Treating sleep apnea can not only alleviate these physical symptoms but also improve overall health and quality of life.
Mental and Emotional Symptoms
Sleep apnea not only affects physical well-being but also has a significant impact on mental and emotional health. One of the most prominent mental symptoms of sleep apnea is excessive daytime sleepiness. Due to the disrupted sleep caused by frequent apneas, individuals with sleep apnea often experience excessive fatigue, which can impact cognitive function, concentration, and memory recall. This can lead to difficulties in work or school performance and overall productivity. Additionally, sleep apnea has been linked to mood disorders such as depression and anxiety. The chronic lack of quality sleep can contribute to feelings of irritability, mood swings, and a general sense of low mood. It is important to note that addressing the underlying sleep apnea condition through appropriate treatment options can help alleviate these mental and emotional symptoms and improve overall quality of life.
Types of Sleep Apnea

Sleep apnea can be classified into three main types: obstructive sleep apnea (OSA), central sleep apnea (CSA), and complex sleep apnea syndrome (CSAS). Obstructive sleep apnea is the most common form, occurring when the airway becomes partially or completely blocked during sleep, leading to breathing difficulties. Central sleep apnea, on the other hand, occurs when the brain fails to send the proper signals to the muscles that control breathing. It is less common than obstructive sleep apnea and is often associated with underlying medical conditions such as heart failure or stroke. Lastly, complex sleep apnea syndrome refers to a combination of obstructive and central sleep apnea elements. Understanding the different types of sleep apnea is crucial for accurate diagnosis and appropriate treatment. If you’d like to learn more about the effects of sleep apnea on dreaming, you can read about its impact on dream recall here.
Obstructive Sleep Apnea (OSA)
Obstructive Sleep Apnea (OSA) is the most common and widely known form of sleep apnea. It occurs when the muscles in the back of the throat fail to keep the airway open during sleep. This obstruction can lead to frequent pauses in breathing, often accompanied by loud snoring and choking sounds as the individual struggles to breathe. OSA can have various causes, including anatomical factors such as a large tongue, tonsils, or uvula, as well as obesity, which can contribute to extra tissue in the throat. The repeated interruptions in breathing can cause fragmented and restless sleep, leading to excessive daytime sleepiness and fatigue.
The consequences of untreated OSA can be significant, ranging from mild symptoms such as morning headaches and irritability to more severe health issues like high blood pressure, increased risk of heart disease, and stroke. OSA can also have an impact on mental health, with individuals experiencing difficulties in concentration, memory, and mood disturbances.
To diagnose OSA, a sleep specialist may recommend a sleep study called polysomnography. This test measures various physiological parameters during sleep, including brain waves, eye movements, and respiratory patterns. Treatment options for OSA include lifestyle modifications such as weight loss and avoiding alcohol and sedatives, as well as the use of continuous positive airway pressure (CPAP) therapy, which involves wearing a mask that delivers pressurized air to keep the airway open during sleep. In some cases, surgery may be recommended to correct anatomical abnormalities.
It’s important to recognize the symptoms of OSA and seek medical attention if suspected, as proper diagnosis and treatment can significantly improve sleep quality and overall well-being. Don’t be discouraged if you have OSA, as there are effective interventions available to manage the condition and enhance your sleep experience.
Central Sleep Apnea (CSA)
Central Sleep Apnea (CSA) is a less common form of sleep apnea compared to Obstructive Sleep Apnea (OSA). Unlike OSA, where the airway becomes partially or completely blocked, CSA occurs when the brain fails to send proper signals to the muscles that control breathing during sleep. This results in a lack of effort to breathe for brief periods. Individuals with CSA may experience temporary cessation of breathing or shallow breaths, leading to disrupted sleep patterns and oxygen deprivation. CSA can be caused by various factors including medical conditions such as congestive heart failure, stroke, or brainstem injury. Additionally, certain medications and high altitudes may also contribute to the development of CSA. It is important to note that CSA can overlap with OSA, resulting in a condition called Complex Sleep Apnea Syndrome (CSAS). It is crucial to accurately diagnose and differentiate between the types of sleep apnea since the treatment approaches may vary. If you are interested in the relationship between central sleep apnea and dreaming, you can read more about it in our article on sleep apnea and lucid dreaming.
Complex Sleep Apnea Syndrome (CSAS)
Complex Sleep Apnea Syndrome (CSAS) is a subtype of sleep apnea that combines features of both obstructive sleep apnea (OSA) and central sleep apnea (CSA). Also known as treatment-emergent central sleep apnea (TECSA), CSAS is characterized by periods of complete or partial cessation of breathing during sleep due to a lack of respiratory effort. This condition typically occurs in individuals who have been diagnosed and treated for OSA using continuous positive airway pressure (CPAP) therapy or other forms of positive airway pressure (PAP) therapy. While the exact cause of CSAS is still not fully understood, it is believed to arise as a result of the interaction between a pre-existing vulnerability in the central respiratory control system and the application of positive airway pressure therapy. Individuals with CSAS may experience symptoms such as loud snoring, frequent awakenings, excessive daytime sleepiness, and poor sleep quality. diagnosing CSAS involves a comprehensive sleep study that includes measurements of respiratory effort, airflow, and oxygen saturation. Treatment options for CSAS include adjusting the pressure settings of CPAP therapy, the use of adaptive servo-ventilation (ASV) therapy, or a combination of these approaches. Ultimately, a personalized treatment plan should be developed in collaboration with a healthcare professional to effectively manage CSAS and improve sleep quality.
Diagnosis of Sleep Apnea
Obtaining a proper diagnosis for sleep apnea is essential for effective treatment. There are several diagnostic methods available, depending on the severity and suspected type of sleep apnea. One common method is a sleep study, also known as polysomnography, which is conducted in a sleep laboratory. This comprehensive test monitors various aspects of sleep, including brain activity, oxygen levels, heart rate, and breathing patterns. Another option is a Home Sleep Apnea Testing (HSAT), where a portable device is used to collect data on breathing, oxygen levels, and other relevant parameters while sleeping at home. Additionally, there are other diagnostic methods, such as the Epworth Sleepiness Scale and the use of specialized questionnaires, which can help assess daytime sleepiness and other symptoms associated with sleep apnea. These diagnostic techniques allow healthcare professionals to accurately diagnose sleep apnea, determine its severity, and develop an appropriate treatment plan tailored to each individual’s needs.
Sleep Study and Polysomnography
Sleep Study and Polysomnography are diagnostic procedures used to evaluate and diagnose sleep disorders, including sleep apnea. A sleep study, also known as a polysomnography, involves monitoring various physiological parameters while an individual sleeps. This comprehensive test is typically conducted in a specialized sleep center or laboratory, but it can also be done at home in some cases.
During a sleep study, the patient is connected to several sensors and electrodes that measure different aspects of their sleep. These sensors record brain activity, eye movements, muscle activity, heart rate, oxygen levels, and respiratory patterns. The collected data provides valuable insights into sleep architecture and any disruptions that may be occurring, such as apneas or hypopneas (shallow breathing).
Polysomnography allows healthcare professionals, such as sleep specialists, to assess the severity and type of sleep apnea a person may have. It helps differentiate between obstructive sleep apnea (OSA), central sleep apnea (CSA), or a combination of both, known as complex sleep apnea syndrome (CSAS). The recordings obtained during the sleep study are carefully analyzed to determine the frequency and duration of apneas, as well as the impact on sleep quality.
A sleep study and polysomnography play a crucial role in diagnosing sleep apnea and determining the most appropriate treatment plan. By accurately identifying the nature and severity of the sleep disorder, healthcare professionals can provide personalized and effective management strategies to improve sleep and overall well-being.
Home Sleep Apnea Testing (HSAT)
Home Sleep Apnea Testing (HSAT) is a convenient and cost-effective alternative to in-lab sleep studies for the diagnosis of sleep apnea. With HSAT, individuals can undergo testing from the comfort of their own homes, making it a more accessible option for many. HSAT typically involves wearing a portable sleep monitoring device during sleep, which measures parameters such as airflow, breathing effort, oxygen levels, and heart rate. These devices are easy to use and non-intrusive, allowing individuals to sleep in their own beds while collecting data. After the HSAT is completed, the recorded data is analyzed by sleep specialists, who can then determine if sleep apnea is present and, if so, the severity of the condition. It is important to note that HSAT may not be suitable for everyone, as it may not capture certain nuances that an in-lab study can. It is essential to consult with a healthcare professional to determine the most appropriate testing method based on individual circumstances. HSAT offers a convenient and efficient way to diagnose sleep apnea, enabling individuals to take necessary steps towards managing their condition and improving their sleep quality.
Other Diagnostic Methods
Other diagnostic methods beyond sleep studies and polysomnography may be employed to aid in the diagnosis of sleep apnea. One such method is the use of nocturnal oximetry, which measures the oxygen levels in the blood throughout the night. This test can help identify dips in oxygen saturation that may indicate the presence of sleep apnea. Additionally, a multiple sleep latency test (MSLT) may be conducted to evaluate daytime sleepiness and determine if it is a result of underlying sleep apnea. This test measures how quickly someone falls asleep during several brief nap opportunities throughout the day. Another diagnostic tool, called the maintenance of wakefulness test (MWT), measures a person’s ability to stay awake during designated periods of wakefulness. It is typically used to assess excessive daytime sleepiness and rule out conditions such as sleep apnea. In some cases, an imaging test like an MRI or CT scan may be recommended to evaluate the structure of the airway and assess for any obstructions that may contribute to sleep apnea. These additional diagnostic methods can provide valuable information to healthcare professionals and aid in the accurate diagnosis of sleep apnea, leading to appropriate treatment interventions.
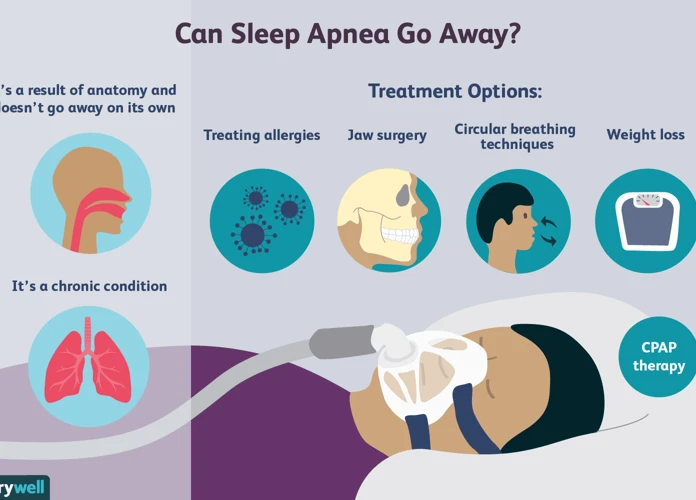
Treatments for Sleep Apnea
Treating sleep apnea is essential for managing the condition and improving overall quality of life. There are various treatment options available, depending on the severity and underlying cause of sleep apnea. Lifestyle changes and self-help measures, such as weight loss, avoiding alcohol and sedatives, and sleeping on your side, can be beneficial for mild cases. For moderate to severe sleep apnea, continuous positive airway pressure (CPAP) therapy is often recommended, which involves wearing a mask that delivers a constant flow of air to keep the airways open during sleep. Oral appliance therapy (OAT) is another non-invasive option that involves using a dental device to help keep the airways open. In some cases, surgery may be necessary to correct structural issues obstructing the airway. It’s important to work closely with a healthcare professional to determine the most suitable treatment approach for your specific condition and symptoms.
Lifestyle Changes and Self-Help Measures
Making lifestyle changes and implementing self-help measures can play a crucial role in managing sleep apnea and improving overall sleep quality. Here are some effective strategies that individuals with sleep apnea can incorporate into their daily lives:
1. Weight loss: If you are overweight or obese, shedding excess pounds can significantly reduce the severity of sleep apnea. Losing weight helps to alleviate constriction in the airway, making it easier to breathe during sleep.
2. Regular exercise: Engaging in regular physical activity can have multiple benefits for sleep apnea. Exercise helps to improve cardiovascular health, strengthen muscles, and promote weight loss. Aim for at least 30 minutes of moderate-intensity exercise, such as brisk walking or cycling, most days of the week.
3. Avoid alcohol and sedatives: Alcohol and sedatives can relax the muscles in the throat, leading to increased airway collapse during sleep. It is advisable to avoid the consumption of alcohol and sedatives, especially close to bedtime.
4. Quit smoking: Smoking is known to contribute to airway inflammation and worsen the symptoms of sleep apnea. Quitting smoking can improve both your sleep apnea and overall health.
5. Sleep position: Sleeping on your back can exacerbate sleep apnea symptoms. Try sleeping on your side or elevate your head with pillows to help keep the airways open during sleep.
6. Establish a regular sleep schedule: Maintain a consistent sleep routine by going to bed and waking up at the same time every day. This helps regulate your body’s internal clock and promotes better sleep.
7. Maintain a sleep-friendly environment: Create a comfortable and conducive sleep environment by keeping the bedroom cool, dark, and quiet. Consider using earplugs, eye masks, or white noise machines if necessary.
Implementing these lifestyle changes and self-help measures can greatly enhance the effectiveness of other treatment options and improve your overall sleep apnea management. It is important to consult with a healthcare professional for personalized guidance and support.
Continuous Positive Airway Pressure (CPAP) Therapy
Continuous Positive Airway Pressure (CPAP) therapy is a widely used and effective treatment for sleep apnea. It involves wearing a mask over the nose or both the nose and mouth while sleeping. The mask is connected to a machine that delivers a constant and steady flow of air pressure, which helps to keep the airways open and prevents them from collapsing during sleep. The primary goal of CPAP therapy is to eliminate or reduce the occurrence of apneas and hypopneas, allowing for uninterrupted breathing and a more restful sleep. Not only does CPAP therapy alleviate the symptoms of sleep apnea, such as snoring and excessive daytime sleepiness, but it also helps to improve overall health and reduce the risk of associated complications. Patients may experience an adjustment period when starting CPAP therapy, as the sensation of wearing a mask and the presence of airflow can take some getting used to. However, with proper support and guidance from healthcare professionals, many individuals find CPAP therapy to be a life-changing treatment option. It is important to note that adherence to CPAP therapy is crucial for its effectiveness. Regular use of the CPAP machine, following the prescribed pressure settings, and maintaining good mask hygiene are essential for optimal therapeutic outcomes. If you suspect you have sleep apnea, consult with a healthcare professional who can guide you through the process of obtaining a CPAP machine and provide ongoing support to ensure successful integration of CPAP therapy into your sleep routine.
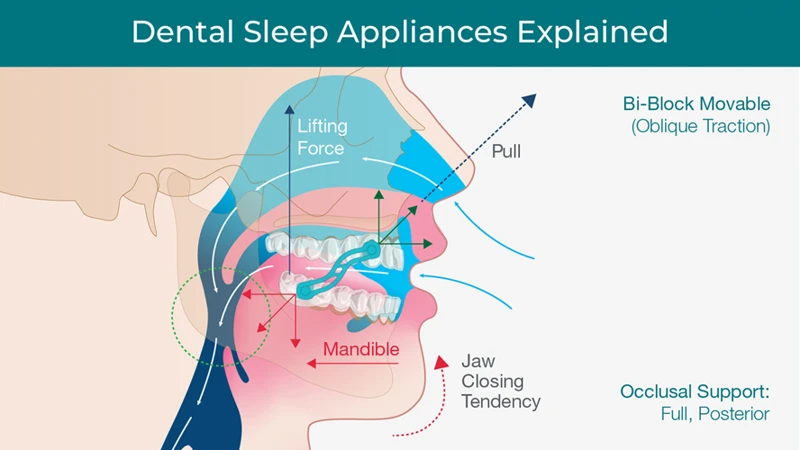
Oral Appliance Therapy (OAT)
Oral Appliance Therapy (OAT) is a non-invasive treatment option for individuals with mild to moderate obstructive sleep apnea (OSA) or who are intolerant to continuous positive airway pressure (CPAP) therapy. OAT involves the use of custom-made dental devices, also known as oral appliances or mandibular advancement devices (MADs), which are worn during sleep to help maintain an open airway.
OAT Mechanism: These oral appliances work by repositioning the lower jaw and tongue, effectively preventing the collapse of the airway and reducing the occurrences of apneas and hypopneas. By advancing the mandible in a forward position, these devices help to increase the space in the oral cavity and improve airflow.
Effectiveness of OAT: Studies have shown that oral appliance therapy can effectively reduce the frequency and severity of sleep apnea events. It has also been found to improve daytime sleepiness, quality of life, and overall sleep architecture. However, the success of OAT may vary depending on individual factors such as the severity of sleep apnea, anatomical characteristics, and patient compliance.
Types of Oral Appliances: There are different types of oral appliances available, and the choice depends on various factors including the patient’s specific needs and preferences. Some of the commonly used devices include mandibular advancement devices, tongue-retaining devices, and combination therapy devices that combine mandibular advancement with tongue stabilization.
Customization and Fitting: To ensure optimal effectiveness and comfort, oral appliances are custom-made to fit each individual’s mouth. This is typically done by a dentist or orthodontist specialized in sleep medicine. The fitting process involves taking impressions, bite registrations, and jaw measurements to fabricate a personalized appliance that fits securely and comfortably.
Monitoring and Follow-up: Once the oral appliance is fitted, regular follow-up appointments are necessary to monitor progress and make any necessary adjustments. These appointments may involve assessing the fit, evaluating treatment efficacy, and addressing any issues or discomfort that may arise.
Oral Appliance Therapy (OAT) offers a viable alternative for individuals with mild to moderate obstructive sleep apnea who cannot tolerate or prefer not to use CPAP therapy. It is important to consult with a qualified sleep specialist or dentist experienced in sleep medicine to determine if this treatment option is suitable for your specific needs and to ensure proper fitting and ongoing care.
Surgery
Surgery is considered a treatment option for sleep apnea when other non-invasive methods have failed to provide adequate relief. The goal of surgery is to remove or correct the underlying structural abnormalities that contribute to the obstruction of the airway during sleep. There are different types of surgeries available depending on the specific cause and severity of the sleep apnea. Some common surgical procedures include:
1. Uvulopalatopharyngoplasty (UPPP): This procedure involves the removal of excess tissue from the throat, including the uvula, tonsils, and parts of the soft palate. By widening the airway, UPPP can help alleviate the blockage and improve airflow during sleep.
2. Septoplasty: This surgery is performed to correct a deviated septum, which can contribute to breathing difficulties during sleep. Septoplasty straightens the nasal septum, allowing for better nasal airflow and reducing the risk of airway obstruction.
3. Maxillomandibular advancement (MMA): This surgical procedure involves repositioning the upper and lower jaw to enlarge the airway and increase its stability. By moving the jaw forward, MMA helps to prevent the collapse of the tongue and other soft tissues, effectively reducing the occurrence of apneas.
4. Tracheostomy: In severe cases of sleep apnea that cannot be effectively treated with other methods, a tracheostomy may be performed. This procedure involves creating a small opening in the windpipe and inserting a tube to bypass the obstructed upper airway. Although effective, tracheostomy is typically considered a last resort due to its invasive nature.
It’s important to note that while surgery can be an effective treatment for sleep apnea, it is not suitable for everyone. The decision to undergo surgery should be made in consultation with a healthcare professional who can assess the severity of the condition and determine the most appropriate course of action. Additionally, surgery may be combined with other treatments, such as CPAP therapy, to ensure optimal results.
Alternative and Complementary Treatments
Alternative and complementary treatments can be considered for individuals seeking alternative options or additional support in managing sleep apnea. Although these treatments should not replace conventional treatments, they may offer some relief or improvement in sleep quality. One alternative treatment that has gained attention is acupuncture, an ancient Chinese practice that involves inserting thin needles into specific points on the body to promote balance and healing. Some studies suggest that acupuncture may help reduce sleep apnea symptoms by improving respiratory function and reducing inflammation. Additionally, certain herbal remedies, such as valerian root or chamomile, are known for their relaxing and sleep-inducing properties. However, it’s important to consult with a qualified herbalist or healthcare professional before incorporating herbal remedies into your treatment plan to ensure their safety and efficacy. Lastly, practices like yoga and specific breathing techniques, such as the Buteyko method, may help improve breathing patterns and overall respiratory function. These alternative and complementary treatments can be explored in conjunction with traditional treatments for a more holistic approach to managing sleep apnea.
Acupuncture
– Acupuncture is an ancient Chinese medical practice that involves inserting thin needles into specific points on the body to promote healing and balance energy flow.
– Acupuncture has been explored as a potential treatment for sleep apnea, although research on its effectiveness is limited. It is believed that acupuncture may help improve sleep apnea symptoms by stimulating nerve pathways and releasing endorphins, which can promote relaxation and reduce inflammation.
– Some studies suggest that acupuncture may help in reducing the frequency of apneas and improving overall sleep quality in individuals with sleep apnea.
– In addition to sleep apnea-specific treatments, acupuncture may also address underlying health issues that contribute to sleep apnea, such as stress, anxiety, and chronic pain.
– Before considering acupuncture as a treatment for sleep apnea, it is important to consult with a qualified acupuncturist who has experience in treating sleep disorders.
– Acupuncture is generally considered safe when practiced by a trained professional using sterile needles. However, it may not be suitable for everyone and should not replace conventional medical treatments for sleep apnea.
– It is crucial to approach acupuncture as part of an overall comprehensive treatment plan for sleep apnea, including lifestyle modifications and other evidence-based therapies.
– As with any alternative treatment, individual results may vary, and it is important to communicate with healthcare professionals and monitor the progress of sleep apnea symptoms while undergoing acupuncture.
Herbal Remedies
Herbal remedies have been used for centuries to address various health conditions, and they are also explored as a potential complementary treatment for sleep apnea. While scientific research on the effectiveness of herbal remedies for sleep apnea is limited, some herbs have shown promise in promoting relaxation, reducing inflammation, and improving overall sleep quality.
1. Valerian root: Valerian root is commonly used as a natural remedy for insomnia and anxiety. It may help improve sleep quality and reduce the frequency of awakenings during the night.
2. Chamomile: Chamomile is well-known for its calming properties and is often used as a sleep aid. It can help reduce anxiety and promote relaxation before bedtime.
3. Lemon balm: Lemon balm is a herb that belongs to the mint family and has been used traditionally to improve sleep. It has mild sedative properties and may help reduce anxiety and promote restful sleep.
4. Lavender: Lavender is widely recognized for its soothing aroma. It can be used as an essential oil or in the form of herbal tea to promote relaxation and improve sleep quality.
5. Passionflower: Passionflower is a natural sedative that can help reduce anxiety and promote better sleep. It may also help alleviate insomnia and improve sleep duration.
It is important to note that while herbal remedies may offer potential benefits for sleep apnea, they should not replace medical treatment or therapies recommended by healthcare professionals. It is always advisable to consult with a healthcare provider before incorporating herbal remedies into your sleep apnea management plan.
Yoga and Breathing Techniques
Yoga and breathing techniques have gained recognition as complementary approaches in managing sleep apnea symptoms. Yoga, with its emphasis on mindfulness, relaxation, and controlled deep breathing, can help improve overall sleep quality. Specific yoga poses, such as the corpse pose (Savasana), the bridge pose (Setu Bandhasana), and the shoulder stand (Sarvangasana), can be beneficial for individuals with sleep apnea. These poses promote relaxation, open up the airways, and improve circulation. Additionally, pranayama, which is the practice of controlled breathing exercises, can help strengthen the respiratory muscles and enhance lung capacity. Techniques like alternate nostril breathing (Nadi Shodhana) and belly breathing (Diaphragmatic breathing) can be incorporated into a daily routine to alleviate sleep apnea symptoms. Regular practice of yoga and breathing techniques can help reduce stress, promote relaxation, and improve overall respiratory function, ultimately contributing to better sleep outcomes for individuals with sleep apnea.
Managing Sleep Apnea
Managing sleep apnea involves implementing various strategies to reduce the frequency and severity of apnea episodes, improve breathing during sleep, and enhance overall sleep quality. Sleep positioning plays a crucial role in managing sleep apnea, as sleeping on the side can help keep the airways open and reduce obstructions. Additionally, weight management is important, as excess weight can contribute to the narrowing of the airways. Managing allergies and nasal congestion is also essential, as any blockages can further impede proper breathing. By addressing these factors and adopting a sleep-friendly environment, individuals with sleep apnea can significantly improve their sleep quality and alleviate the symptoms associated with the condition. Creating a regular sleep schedule and maintaining treatment compliance, such as consistently using CPAP therapy or oral appliance therapy, are also vital components of effectively managing sleep apnea.
Sleep Positioning
Sleep positioning plays a significant role in managing sleep apnea symptoms and ensuring a more restful night’s sleep. By making conscious adjustments to how you position your body during sleep, you can potentially reduce the frequency and severity of sleep apnea episodes. The following are some sleep positioning strategies that may be beneficial:
1. Sleeping on your side: Lying on your side can help keep your airway open and reduce the likelihood of it becoming blocked during sleep. This position can also minimize the chances of snoring, which is commonly associated with sleep apnea. For added support, you can place a pillow between your knees or use a full-body pillow.
2. Elevating your upper body: Sleeping with your head and upper body elevated at an angle can prevent the relaxation of throat muscles and reduce the risk of airway obstruction. This can be achieved by using a wedge-shaped pillow or an adjustable bed that allows you to raise the head of the mattress.
3. Avoiding sleeping on your back: Sleeping on your back can exacerbate sleep apnea symptoms as gravity causes the tongue and soft tissues in the throat to block the airway. To discourage back sleeping, you can try using a body pillow or placing cushions on either side of your body to keep yourself in a side-sleeping position throughout the night.
4. Using positional therapy devices: There are specialized devices available that provide positional therapy for sleep apnea. These devices can include vests, shirts, or pillows with strategically placed supports that encourage side-sleeping and help maintain optimal airway alignment.
It’s important to note that finding the right sleep position may require some trial and error, as everyone’s condition and comfort level may vary. Consulting with a healthcare professional or sleep specialist can provide personalized guidance and recommendations based on your specific needs.
Weight Management
Weight management plays a crucial role in the management of sleep apnea. Excess weight, particularly in the neck and throat area, can contribute to the narrowing and obstruction of the airway during sleep, leading to episodes of apnea. Losing weight can significantly alleviate the symptoms of sleep apnea and even eliminate the condition in some cases. Implementing a healthy and balanced diet, combined with regular exercise, is key to achieving weight loss goals. This includes reducing the consumption of processed foods, sugary beverages, and high-fat meals. Instead, focus on incorporating whole foods, such as fruits, vegetables, lean proteins, and whole grains, into your diet. Additionally, portion control is essential in weight management. It is recommended to consult with a registered dietitian or nutritionist to create a personalized meal plan tailored to your specific needs. Regular physical activity is also important in weight management. Engage in regular aerobic exercises, such as walking, swimming, or cycling, for at least 30 minutes a day. Strength training exercises can also be beneficial in building muscle mass and boosting metabolism. By maintaining a healthy weight, individuals with sleep apnea can significantly improve their breathing during sleep and reduce the severity of their symptoms.
Managing Allergies and Nasal Congestion
Managing Allergies and Nasal Congestion
– Keep your environment clean and free from allergens. Dust, pet dander, mold, and pollen are common allergens that can contribute to nasal congestion and worsen sleep apnea symptoms. Regularly vacuum your living space, wash bedding in hot water, and use air purifiers to minimize exposure to these allergens.
– Implement nasal irrigation. Nasal irrigation, also known as nasal saline irrigation or nasal rinsing, can help alleviate nasal congestion and clear out irritants. You can use a neti pot or a saline nasal spray to flush out the nasal passages. Be sure to use sterile or distilled water and follow proper hygiene practices to avoid any potential infections.
– Consider using nasal decongestants. Nasal decongestant sprays can provide temporary relief from nasal congestion by shrinking the blood vessels in the nasal passages. However, prolonged and excessive use of these sprays can lead to dependency and rebound congestion, so it’s important to follow the instructions and not use them for more than a few days.
– Use nasal strips or dilators. Nasal strips are adhesive strips that are applied to the outside of the nose to help open up the nasal passages. Nasal dilators, on the other hand, are small devices that are inserted into the nostrils to keep them open during sleep. These aids can help improve airflow and alleviate nasal congestion.
– Consult with an allergist or ENT specialist. If you are struggling with persistent allergies or nasal congestion, it may be beneficial to seek professional guidance. An allergist or ear, nose, and throat (ENT) specialist can conduct allergy testing, recommend appropriate medications or treatments, and provide personalized advice to help manage your allergies and nasal congestion effectively.
By implementing these strategies, you can effectively manage allergies and nasal congestion that contribute to sleep apnea symptoms. However, it is important to consult with a healthcare professional for a comprehensive evaluation and personalized treatment plan based on your specific needs and medical history.
Living with Sleep Apnea
Living with sleep apnea requires careful management and lifestyle adjustments to improve sleep quality and overall well-being. Creating a sleep-friendly environment is essential, involving factors such as maintaining a comfortable room temperature, investing in a supportive mattress and pillows, and minimizing noise and distractions. Establishing a regular sleep schedule can help regulate sleep-wake cycles and promote consistent rest. Managing treatment compliance is also crucial, whether it involves using a continuous positive airway pressure (CPAP) machine or wearing an oral appliance. Compliance can be enhanced by practicing good hygiene, keeping equipment clean, and seeking support from healthcare professionals or support groups. Additionally, managing weight through exercise and a healthy diet can help alleviate symptoms of sleep apnea. Seeking allergy treatment and managing nasal congestion can also contribute to better breathing during sleep. By taking these steps and prioritizing self-care, individuals with sleep apnea can improve their quality of life and effectively manage their condition.
Creating a Sleep-friendly Environment
Creating a sleep-friendly environment is essential for individuals with sleep apnea to improve their sleep quality and reduce the severity of their symptoms. Firstly, it is important to make sure that the bedroom is quiet and free from disruptive noises. Consider using earplugs or a white noise machine to drown out any background noise that may disturb your sleep. Additionally, adjusting the room temperature to a cool and comfortable level can promote better sleep. Keeping the bedroom dark by using blackout curtains or an eye mask can help regulate the body’s internal clock and promote melatonin production, which is crucial for a restful sleep. It is also advisable to invest in a supportive and comfortable mattress and pillows that cater to your specific sleep needs. Keeping electronic devices out of the bedroom or using blue light-blocking filters can help reduce exposure to stimulating lights that can interfere with sleep. Creating a clutter-free and relaxing environment can also contribute to a more peaceful sleep atmosphere.
Establishing a Regular Sleep Schedule
Establishing a regular sleep schedule is a key aspect of managing sleep apnea and promoting restful sleep. By maintaining consistent sleep and wake times, you can regulate your body’s internal clock, also known as the circadian rhythm. This helps to synchronize your sleep patterns with the natural light-dark cycle. To establish a regular sleep schedule, consider the following tips:
1. Set a consistent bedtime and wake-up time: Aim to go to bed and wake up at the same time every day, even on weekends. This helps train your body to expect sleep at a certain time, making it easier to fall asleep and wake up naturally.
2. Create a relaxing bedtime routine: Engage in calming activities before bed, such as reading, taking a warm bath, or practicing relaxation techniques like deep breathing or meditation. Avoid stimulating activities, such as using electronic devices or engaging in intense exercise, close to bedtime.
3. Make your bedroom a sleep-friendly environment: Ensure that your sleeping space is comfortable, quiet, and dark. Consider using earplugs, eye masks, or white noise machines to block out any distractions that may interfere with your sleep.
4. Avoid caffeine and alcohol: Limit your consumption of caffeinated beverages, such as coffee and energy drinks, especially in the evening. Similarly, avoid consuming alcohol close to bedtime, as it can disrupt your sleep patterns.
5. Stick to a consistent exercise routine: Engaging in regular physical activity during the day can promote better sleep at night. However, try to complete your exercise routine at least a few hours before bedtime to allow your body time to wind down.
By establishing a regular sleep schedule, you can optimize your sleep quality and manage sleep apnea more effectively. Remember, consistency is key in training your body to follow a predictable sleep-wake routine.
Maintaining Treatment Compliance
Maintaining treatment compliance is crucial for effectively managing sleep apnea and improving symptoms. Once a treatment plan has been established, it is important to adhere to it consistently in order to maximize its benefits. One of the most common and effective treatments for sleep apnea is Continuous Positive Airway Pressure (CPAP) therapy. To maintain compliance with CPAP therapy, it is important to use the device every night as prescribed by the healthcare provider. This involves wearing a mask that covers the nose or both the nose and mouth during sleep. It may take some time to adjust to sleeping with the mask, but it is important to persevere and give the treatment a fair chance. Regular cleaning and maintenance of the CPAP equipment is also essential to ensure its longevity and effectiveness. Additionally, it is important to follow up with the healthcare provider regularly to monitor progress and make any necessary adjustments to the treatment plan. Adhering to the prescribed treatment and actively engaging in the management of sleep apnea can greatly improve symptoms and overall quality of life. Hesitations or concerns about treatment compliance should be discussed with healthcare professionals to find alternative solutions or make appropriate modifications to ensure effective long-term treatment.
Conclusion
Sleep apnea is a complex sleep disorder that can have a profound impact on an individual’s health and well-being. It is important for individuals to recognize the common symptoms of sleep apnea, such as excessive daytime sleepiness, loud snoring, and gasping for breath during sleep, and seek medical attention if necessary. Proper diagnosis and treatment are essential in managing sleep apnea and improving overall quality of life.
Treatment options for sleep apnea range from lifestyle changes and self-help measures to medical interventions such as Continuous Positive Airway Pressure (CPAP) therapy, oral appliance therapy (OAT), and even surgical procedures. It is crucial for individuals with sleep apnea to work closely with healthcare professionals to determine the most suitable treatment plan for their specific condition.
Additionally, alternative and complementary treatments, such as acupuncture, herbal remedies, and yoga and breathing techniques, may also provide some relief for certain individuals. However, it is important to approach these treatments with caution and consult with a healthcare professional before incorporating them into a sleep apnea management plan.
Managing sleep apnea requires a multifaceted approach, including sleep positioning, weight management, and managing allergies and nasal congestion. Creating a sleep-friendly environment, establishing a regular sleep schedule, and maintaining treatment compliance are also essential for effectively managing sleep apnea.
In conclusion, understanding sleep apnea and its impact on one’s health is crucial for early detection and appropriate treatment. By identifying the causes, recognizing the symptoms, and exploring various treatment options, individuals with sleep apnea can improve their sleep quality, reduce the risks associated with the condition, and ultimately enhance their overall well-being. It is important for individuals to work closely with healthcare professionals to develop a personalized treatment plan that addresses their specific needs. With proper management, individuals with sleep apnea can experience significant improvements in their sleep patterns and quality of life.
Frequently Asked Questions
What are the risk factors for sleep apnea?
Several factors can increase the risk of developing sleep apnea, including obesity, a family history of the condition, older age, being male, having a large neck circumference, and certain medical conditions such as hypertension and diabetes.
Can sleep apnea affect children?
Yes, sleep apnea can occur in children. It is often caused by enlarged tonsils or adenoids, obesity, or certain craniofacial abnormalities. Symptoms may include snoring, restless sleep, daytime sleepiness, and difficulty concentrating.
Is sleep apnea dangerous?
Yes, sleep apnea can have serious health consequences if left untreated. It can lead to chronic fatigue, high blood pressure, heart disease, stroke, diabetes, and a higher risk of accidents due to daytime sleepiness.
Can weight loss help alleviate sleep apnea symptoms?
Yes, losing weight can be an effective way to reduce sleep apnea symptoms, especially for overweight individuals. Weight loss can help decrease the severity of obstructions in the airway during sleep.
Are there any non-surgical treatments for sleep apnea?
Yes, there are non-surgical treatments available for sleep apnea. Continuous Positive Airway Pressure (CPAP) therapy, which involves wearing a mask that delivers pressurized air to keep the airway open during sleep, is the most common and effective non-surgical treatment.
How is sleep apnea diagnosed?
Sleep apnea is diagnosed through a sleep study, also known as a polysomnography. This test measures various parameters during sleep, including breathing patterns, oxygen levels, brain activity, and heart rate, to determine the presence and severity of sleep apnea.
Can sleep apnea be cured?
While there is no cure for sleep apnea, it can be effectively managed and treated. Lifestyle changes, such as weight loss and positional therapy, as well as medical interventions like CPAP therapy or oral appliance therapy, can significantly improve sleep apnea symptoms.
Are there any alternative treatments for sleep apnea?
Some alternative treatments, such as acupuncture and certain herbal remedies, have been explored for sleep apnea. However, their effectiveness in treating sleep apnea is still under investigation, and they should be used in conjunction with standard medical interventions.
Is sleep apnea linked to other medical conditions?
Yes, sleep apnea has been linked to several other medical conditions. It is associated with an increased risk of cardiovascular problems, including hypertension, heart disease, and stroke. It is also linked to metabolic disorders like diabetes and may worsen the symptoms of mood disorders such as depression and anxiety.
What can I do to improve my sleep quality with sleep apnea?
In addition to medical treatments, there are several self-help measures to improve sleep quality with sleep apnea. These include maintaining a regular sleep schedule, creating a sleep-friendly environment, avoiding alcohol and sedatives before bed, and managing nasal congestion and allergies.