Narcolepsy, a complex neurological disorder characterized by excessive daytime sleepiness, sudden loss of muscle tone (cataplexy), and vivid dreaming, has long been an intriguing mystery to scientists and medical professionals. While the exact cause of narcolepsy remains elusive, there is growing evidence to suggest that genetics play a significant role in its development. In this article, we will delve into the intricate details of the inheritance patterns of narcolepsy and explore the genetic factors that contribute to its onset. By unraveling the genetic mechanisms and understanding the interplay between genetics and environmental triggers, we hope to shed light on this enigmatic condition and pave the way for better diagnosis, treatment, and genetic counseling.
The Basics of Narcolepsy
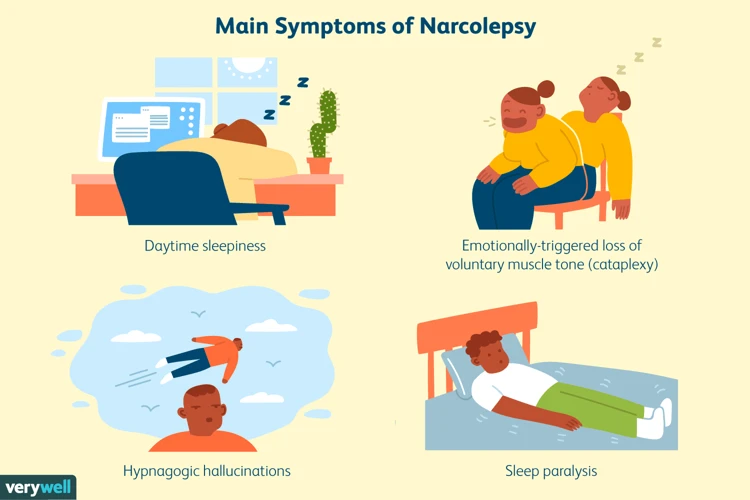
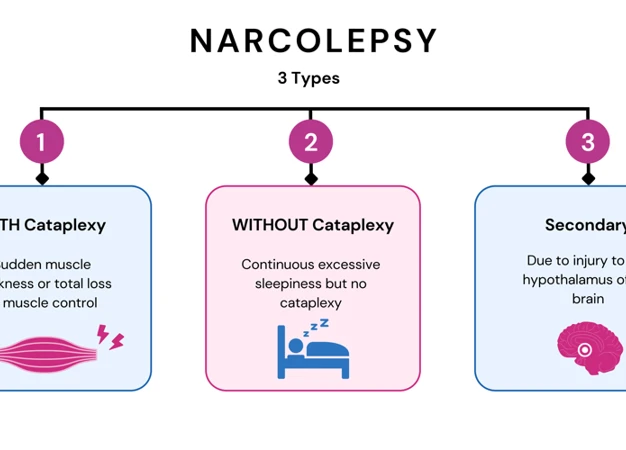
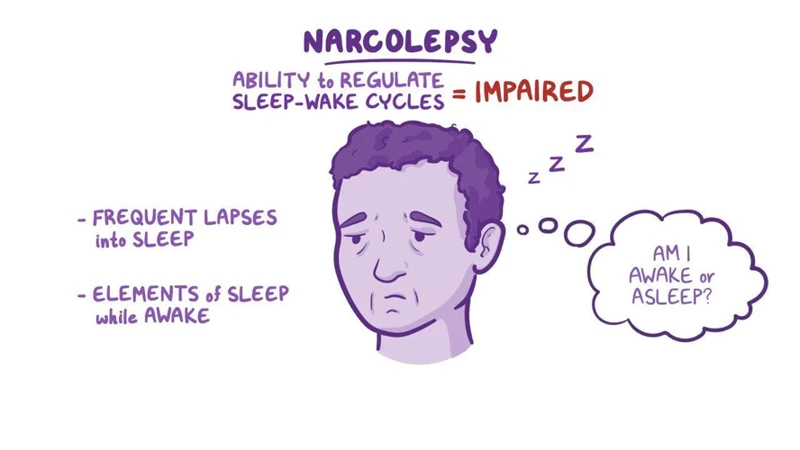
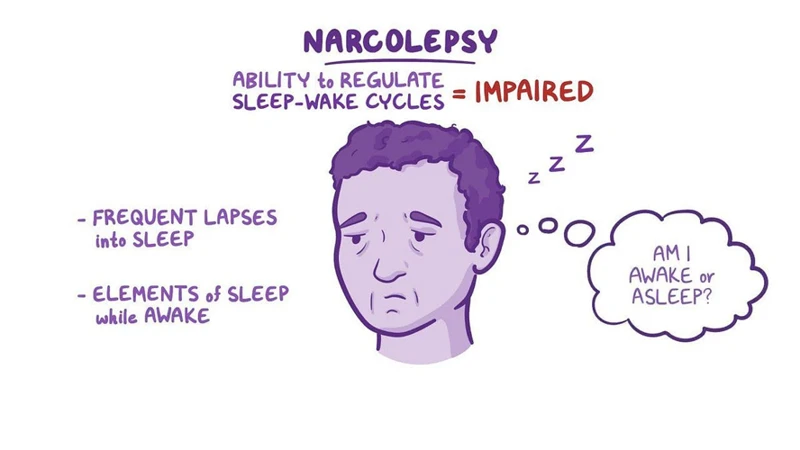
Narcolepsy is a neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. It is characterized by excessive daytime sleepiness, sudden muscle weakness or paralysis (known as cataplexy), hallucinations, and disrupted nighttime sleep. People with narcolepsy often experience irresistible episodes of sleep during the day, regardless of the circumstances. These episodes can occur at inappropriate times, such as during work meetings or while driving, posing serious safety risks. Narcolepsy can greatly impact daily life, making it challenging to maintain regular activities and fulfill responsibilities.
The exact cause of narcolepsy is still not fully understood, but it is believed to involve a combination of genetic and environmental factors. Research has shown that genetic predisposition plays a significant role in the development of narcolepsy. Certain genes, such as the Human Leukocyte Antigen (HLA) genes, have been found to be associated with an increased risk of narcolepsy. These genes help regulate the immune system, suggesting that immune system dysfunction may play a role in the development of the disorder.
Narcolepsy affects both men and women and can occur at any age, although it often begins during adolescence or young adulthood. The symptoms of narcolepsy can vary in severity and may worsen over time. In addition to excessive sleepiness and cataplexy, individuals with narcolepsy may also experience sleep paralysis, which is a temporary inability to move or speak while falling asleep or waking up, as well as vivid dream-like hallucinations. The impact of narcolepsy on daily life can be significant, leading to difficulties in academic or professional settings, strained relationships, and an overall decreased quality of life.
It is important to differentiate narcolepsy from other sleep disorders, such as sleep apnea, which also involves excessive daytime sleepiness but has different underlying causes and symptoms. Understanding the basics of narcolepsy can help individuals recognize the signs and seek appropriate medical care. Early diagnosis and treatment can help manage symptoms and improve the overall wellbeing of individuals with narcolepsy. If you want to learn more about the differences and similarities between narcolepsy and sleep apnea, you can read our article on the topic. For inspiring stories of individuals who have successfully managed narcolepsy, you can check out our collection of narcolepsy success stories.
Genetic Factors in Narcolepsy
Genetic factors play a crucial role in the development of narcolepsy, a complex neurological disorder. One significant finding is the observation of familial aggregation, where narcolepsy tends to run in families. This suggests a genetic predisposition to the condition. Studies have also identified specific genes, such as the Human Leukocyte Antigen (HLA) genes, that are associated with an increased risk of narcolepsy. These genes are involved in regulating the immune system, indicating a possible connection between immune system dysfunction and narcolepsy. Genome-wide association studies have revealed additional genetic variants that contribute to the susceptibility of developing narcolepsy. Understanding the genetic factors involved in narcolepsy is crucial for unraveling the underlying mechanisms of the disorder and may pave the way for improved diagnosis, treatment, and prevention. For more information on the causes and symptoms of narcolepsy, you can refer to our comprehensive guide here.
1. Familial Aggregation
Familial aggregation refers to the observation that narcolepsy tends to occur more frequently within certain families, suggesting a genetic component to the disorder. Numerous studies have shown that individuals with a family history of narcolepsy are at a higher risk of developing the condition themselves. Researchers believe that specific genetic variations are passed down from parents to their children, increasing the susceptibility to narcolepsy.
One study found that first-degree relatives (such as parents, siblings, and children) of individuals with narcolepsy are about 20 to 40 times more likely to develop the disorder compared to the general population. This familial aggregation provides strong evidence for a genetic basis in narcolepsy. It is important to note, however, that not all individuals with a family history of narcolepsy will go on to develop the disorder themselves. Other factors, such as environmental triggers or additional genetic variations, may also play a role in determining whether someone develops narcolepsy.
To better understand the genetic underpinnings of familial aggregation, researchers have conducted genome-wide association studies (GWAS). These studies scan the entire genome for genetic variations that are more common in individuals with narcolepsy compared to those without the condition. GWAS have identified certain regions of the genome that are associated with an increased risk of narcolepsy. One well-known example is the HLA-DQB1 gene, which is part of the Human Leukocyte Antigen (HLA) system involved in immune response. Variations in this gene, particularly the HLA-DQB1*06:02 allele, have been strongly associated with narcolepsy with cataplexy in various populations.
In addition to HLA genes, GWAS have also implicated other genes involved in immune regulation and neuronal development as potential risk factors for narcolepsy. These findings suggest a complex interplay between genetic and immune mechanisms in the development of the disorder. Further research is ongoing to better understand the specific genes and genetic pathways involved in narcolepsy.
The observation of familial aggregation in narcolepsy highlights the role of genetics in the susceptibility to the disorder. Having a family history of narcolepsy increases the likelihood of developing the condition, although other factors, such as environmental triggers, may also contribute to its onset. By studying the genetic variations associated with narcolepsy, researchers aim to unravel the underlying mechanisms and develop more targeted treatments for this debilitating disorder.
2. HLA Alleles
HLA (Human Leukocyte Antigen) alleles have been a subject of interest in narcolepsy research due to their association with the disorder. HLA is a group of genes that play a crucial role in the immune system by helping it recognize and distinguish between self and non-self cells. Specifically, the HLA-DQB1*06:02 allele has been strongly linked to an increased risk of narcolepsy. This association has been found in various populations around the world, further supporting the genetic component of the disorder.
The HLA-DQB1*06:02 allele is present in the majority of individuals with narcolepsy with cataplexy, the most common form of narcolepsy. Research has shown that approximately 90% of individuals with this form of narcolepsy have the HLA-DQB1*06:02 allele, compared to only 12-38% of the general population.
It is important to note that possessing the HLA-DQB1*06:02 allele does not guarantee the development of narcolepsy. While it increases the risk, there are individuals who have the allele but do not develop the disorder. This suggests the involvement of additional genetic and environmental factors in the manifestation of narcolepsy.
Interestingly, the HLA-DQB1*06:02 allele is not specific to narcolepsy and can also be found in individuals without the disorder. This indicates that other factors, such as immune system dysregulation or interactions with other genetic variants, may be necessary for the development of narcolepsy in individuals with this allele.
It is worth mentioning that other HLA alleles, such as HLA-DRB1*15:01 and HLA-DQA1*01:02, have also been associated with an increased risk of narcolepsy, although to a lesser extent than HLA-DQB1*06:02.
The presence of certain HLA alleles, particularly HLA-DQB1*06:02, plays a significant role in the genetic predisposition to narcolepsy. However, the exact mechanisms by which these alleles contribute to the development of the disorder are still not fully understood and require further research. The association with HLA alleles provides valuable insights into the genetic factors involved in narcolepsy and can aid in the diagnosis and understanding of this complex neurological condition.
3. Genome-wide Association Studies
Genome-wide Association Studies (GWAS) have been instrumental in advancing our understanding of the genetic factors associated with narcolepsy. GWAS is a research approach that involves comparing the genomes of individuals with a particular condition, in this case, narcolepsy, to those without the condition in search of genetic variations that are more prevalent in the affected population.
Through GWAS, researchers have identified specific genetic regions that are associated with an increased risk of developing narcolepsy. One of the most significant findings is the involvement of the Human Leukocyte Antigen (HLA) gene complex. The HLA gene complex plays a crucial role in the immune system and is responsible for recognizing and presenting foreign substances, such as viruses or bacteria, to initiate an immune response.
In narcolepsy, variations in the HLA gene complex, particularly the HLA-DQB1*06:02 allele, have been strongly linked to the development of the disorder. Studies have shown that more than 90% of individuals with narcolepsy with cataplexy carry this specific HLA allele compared to around 20-30% in the general population.
Additionally, GWAS studies have highlighted other genetic variations outside the HLA gene complex that contribute to the risk of narcolepsy. These variations involve genes related to the immune system, such as T-cell receptor genes and genes associated with the production of hypocretin/orexin, a neuropeptide that plays a crucial role in regulating wakefulness and sleep.
The findings from GWAS have provided valuable insights into the genetic basis of narcolepsy. However, it is important to note that genetic variations alone are not sufficient to cause narcolepsy. Environmental factors, such as viral infections or psychological stress, may also play a role in triggering the onset of narcolepsy in genetically susceptible individuals.
GWAS studies have significantly contributed to our understanding of the genetic factors associated with narcolepsy. The identification of specific genetic variations, particularly within the HLA gene complex, has provided valuable insights into the role of the immune system in the development of narcolepsy. Further research is needed to unravel the complex interactions between genetic and environmental factors that contribute to the onset and progression of this intriguing neurological disorder.
Inheritance Patterns of Narcolepsy
The inheritance patterns of narcolepsy provide valuable insights into how this complex neurological disorder is passed down through generations. While the exact genetic mechanisms are still being explored, researchers have identified several inheritance patterns that play a role in the development of narcolepsy. One of these patterns is autosomal dominant inheritance, where a single copy of the mutated gene from one affected parent is sufficient to cause narcolepsy in their offspring. Another pattern is autosomal recessive inheritance, where two copies of the mutated gene, one from each parent, are required for narcolepsy to manifest. Additionally, polygenic inheritance, involving the contribution of multiple genes, has also been implicated in narcolepsy susceptibility. These inheritance patterns provide valuable information for understanding the genetic basis of narcolepsy and can contribute to improved diagnosis, treatment, and genetic counseling for individuals and families affected by this condition.
1. Autosomal Dominant Inheritance
Autosomal dominant inheritance is one of the patterns observed in the transmission of narcolepsy through generations. In this type of inheritance, a single copy of the mutated gene is sufficient to cause the disorder. This means that if one parent carries the gene mutation, there is a 50% chance of passing it on to each child. However, it’s important to note that not all individuals who inherit the gene mutation will develop narcolepsy. Other factors, such as environmental triggers or additional genetic variations, may also play a role in determining the expression and severity of the disorder.
Research has identified several genes that are associated with autosomal dominant narcolepsy, with the most significant being the gene known as HCRTR2, which codes for the hypocretin receptor 2. Mutations in this gene disrupt the normal functioning of the receptor, leading to a deficiency in hypocretin signaling, a key factor in regulating sleep-wake cycles. As a result, individuals with autosomal dominant narcolepsy experience excessive daytime sleepiness, cataplexy, and other symptoms associated with the disorder.
Although autosomal dominant narcolepsy is relatively rare compared to other inheritance patterns, studying families with this type of inheritance has provided valuable insights into the genetic basis of narcolepsy. Understanding the role of specific gene mutations in the development of narcolepsy can aid in the development of targeted therapies and interventions. It also highlights the importance of genetic testing and counseling for individuals and families affected by autosomal dominant narcolepsy, as it can provide valuable information regarding the risks and potential inheritance patterns for future generations.
2. Autosomal Recessive Inheritance
Autosomal recessive inheritance is another inheritance pattern that has been observed in narcolepsy. In this pattern, both parents are carriers of a mutated gene related to narcolepsy but do not show any symptoms themselves. When both parents pass on their respective mutated genes to their child, the child has a higher risk of developing narcolepsy.
In the context of narcolepsy, researchers have identified specific gene mutations associated with the disorder. One such gene is the gene that codes for the hypocretin receptor 2 (HCRTR2). When this gene is mutated, it can lead to a decrease or complete loss of hypocretin receptor function, resulting in the development of narcolepsy with cataplexy.
When both parents carry a single copy of the mutated HCRTR2 gene, they are considered carriers for autosomal recessive narcolepsy. Carriers typically do not experience symptoms of narcolepsy themselves, but they can pass on the mutated gene to their children. If a child inherits a mutated gene from both parents, their chances of developing narcolepsy increase significantly.
To better understand how narcolepsy can be inherited in an autosomal recessive pattern, let’s take a closer look at a hypothetical scenario:
1. Both parents are carriers of the mutated HCRTR2 gene but do not have narcolepsy themselves.
2. Each parent has a 50% chance of passing on either the mutated gene or the normal gene to their child.
3. If both parents pass on the mutated gene (a 25% chance), the child is at risk of inheriting narcolepsy and may develop the disorder.
4. If the child receives one mutated gene and one normal gene (a 50% chance), they will not develop narcolepsy but will become a carrier of the mutated gene, like their parents.
5. If both parents pass on the normal gene (a 25% chance), the child will not develop narcolepsy and will not be a carrier for the mutated gene.
It is important to note that inheriting a mutated gene associated with narcolepsy does not guarantee that an individual will develop the disorder. Other genetic and environmental factors may also contribute to the development of narcolepsy. Autosomal recessive inheritance is just one of the possible inheritance patterns observed in narcolepsy, and further research is still needed to fully understand the complex genetic mechanisms involved.
Understanding the various inheritance patterns is crucial for genetic counseling and assessing the risk of narcolepsy in families with a history of the disorder. By identifying individuals who carry mutated genes associated with narcolepsy, healthcare professionals can provide appropriate guidance, support, and potentially early interventions to minimize the impact of the disorder on individuals’ lives.
3. Polygenic Inheritance
Polygenic inheritance is another important inheritance pattern that has been linked to narcolepsy. Unlike Mendelian patterns of inheritance, which are determined by a single gene, polygenic inheritance involves the interaction of multiple genes in contributing to the development of a trait or disorder. In the case of narcolepsy, research has shown that multiple genes are involved in its susceptibility.
Various genome-wide association studies (GWAS) have identified several genetic variations across different chromosomes that are associated with an increased risk of narcolepsy. These variations may be present in different combinations, and individuals with a higher number of risk alleles have a greater likelihood of developing the disorder. The specific genes involved in polygenic inheritance have not yet been fully determined, but they likely play a role in regulating the immune system, neurotransmitter function, and sleep-wake cycles.
Polygenic inheritance means that the risk of developing narcolepsy is influenced by the cumulative effect of these genetic variations, as well as interactions with environmental factors. It is important to note that having these genetic variations does not guarantee the development of narcolepsy, as other factors, both genetic and environmental, also come into play.
Understanding the polygenic nature of narcolepsy can have implications for genetic counseling and risk assessment. Genetic counselors can use information about an individual’s specific combination of genetic variations to estimate their risk of developing narcolepsy. This knowledge can help individuals make informed decisions and take proactive measures to manage their sleep patterns and seek appropriate medical care.
Polygenic inheritance plays a role in the susceptibility to narcolepsy. Multiple genes, with variations located across different chromosomes, interact to contribute to the development of this complex disorder. While the specific genes involved have not been fully elucidated, their influence on immune function, neurotransmitters, and sleep-wake cycles is likely significant. Recognizing the polygenic nature of narcolepsy enhances our understanding of its genetic basis and provides valuable information for genetic counseling and risk assessment.
Understanding the Genetic Mechanisms
Understanding the genetic mechanisms underlying narcolepsy is crucial in unraveling the mysteries of this complex disorder. One significant genetic factor is dysfunction in the orexin system. Orexins, also known as hypocretins, are neuropeptides that play a pivotal role in regulating wakefulness and sleep. In individuals with narcolepsy, there is a deficiency of orexin-producing neurons in the brain, resulting in disrupted sleep-wake cycles. This deficiency is thought to be caused by an autoimmune response where the body’s immune system mistakenly attacks and destroys these neurons. Another genetic mechanism implicated in narcolepsy involves mutations in the hypocretin receptor genes. These mutations can prevent the receptors from properly receiving and transmitting signals, further contributing to the disruptions in sleep and wakefulness. By understanding these genetic mechanisms, researchers can develop targeted therapies aimed at restoring orexin function and potentially alleviating the symptoms of narcolepsy.
1. Orexin System Dysfunction
Orexins, also known as hypocretins, are neuropeptides produced in the hypothalamus region of the brain. They play a crucial role in regulating the sleep-wake cycle and promoting wakefulness. Dysfunction of the orexin system has been strongly associated with narcolepsy. In individuals with narcolepsy, there is a deficiency or complete absence of orexin production, which leads to a disruption in the normal sleep-wake regulation.
The exact cause of orexin system dysfunction in narcolepsy is still not fully understood. However, it is believed to involve an autoimmune response in which the body’s own immune system mistakenly targets and destroys the cells that produce orexin. This autoimmune response may be triggered by a combination of genetic and environmental factors, although the specific triggers are not yet fully known.
The absence or deficiency of orexin in individuals with narcolepsy leads to the symptoms experienced, including excessive daytime sleepiness and cataplexy. Without the proper regulation of the sleep-wake cycle, individuals with narcolepsy struggle to stay awake during the day and may experience sudden episodes of muscle weakness or paralysis triggered by emotions. These symptoms can significantly impact their daily life and overall well-being.
Understanding the dysfunction of the orexin system in narcolepsy has played a crucial role in the development of treatments. Medications that increase the levels of orexin in the brain, such as selective orexin receptor agonists, have shown promise in managing the symptoms of narcolepsy. By targeting the underlying cause of orexin deficiency, these medications can help improve daytime wakefulness and reduce the frequency of cataplexy episodes.
Research continues to unravel the complexities of orexin system dysfunction in narcolepsy. Further understanding of the mechanisms involved in the autoimmune response and the genetic factors that contribute to orexin deficiency will aid in the development of more targeted and effective treatments. By addressing the specific dysfunction in the orexin system, researchers and clinicians are working towards improving the management and quality of life for individuals with narcolepsy.
2. Hypocretin Receptor Mutations
Narcolepsy is a complex disorder that involves various genetic mechanisms, one of which is hypocretin receptor mutations. Hypocretins, also known as orexins, are neuropeptides that play a crucial role in the regulation of wakefulness and sleep. They are produced by a group of cells in the hypothalamus called the hypocretin/orexin neurons. These neurons release hypocretins which bind to and activate specific receptors known as hypocretin receptors.
In individuals with narcolepsy, there can be mutations or deficiencies in the hypocretin receptors. This disruption in the hypocretin system has been linked to the symptoms of excessive daytime sleepiness and abnormal transitions between sleep and wakefulness. Research has found that individuals with narcolepsy often have lower levels of hypocretin in their cerebrospinal fluid. This deficiency is thought to result from an autoimmune destruction of the hypocretin-producing cells.
There are two types of hypocretin receptor mutations that have been identified in narcolepsy: HCRTR1 and HCRTR2. HCRTR2 mutations are less common and primarily related to familial cases of narcolepsy. Mutations in the HCRTR2 gene have been found to lead to abnormalities in the function of the hypocretin receptor 2, which subsequently disrupts the sleep-wake cycle.
On the other hand, HCRTR1 gene mutations are relatively rare, but they have been associated with sporadic cases of narcolepsy. These mutations result in dysfunction of the hypocretin receptor 1, affecting its ability to bind with hypocretin and transmit the wake-promoting signals.
It is important to note that while hypocretin receptor mutations are one genetic mechanism involved in narcolepsy, they are not the sole cause. Narcolepsy is a complex disorder with multifactorial causes, and other genetic factors, such as HLA alleles and polygenic inheritance, also contribute to its development. Understanding the role of hypocretin receptor mutations in narcolepsy helps shed light on the underlying genetic mechanisms involved in sleep-wake regulation and can potentially lead to targeted therapies in the future.
Environmental Triggers and Genetic Susceptibility
Environmental factors and genetic susceptibility both play pivotal roles in the development of narcolepsy. While genetic factors provide a predisposition to the disorder, certain environmental triggers can act as catalysts for its onset. Various factors in the environment, such as infections, hormonal changes, and emotional stress, have been linked to the triggering of narcolepsy symptoms.
One significant environmental trigger associated with narcolepsy is the H1N1 influenza virus, also known as the swine flu. Studies have shown that individuals who were infected with this particular strain of the flu had a higher risk of developing narcolepsy. It is believed that the infection may trigger an autoimmune response in genetically susceptible individuals, leading to the destruction of cells that produce hypocretin, a neurotransmitter that regulates wakefulness and sleep.
Hormonal changes, particularly those during puberty, have also been implicated as potential triggers for the development of narcolepsy. The onset of narcolepsy often occurs during adolescence, a time when major hormonal shifts occur in the body. These hormonal changes may contribute to alterations in the immune system and neurochemical balance, ultimately increasing the risk of developing the disorder.
Emotional stress or significant life events can potentially act as triggers for narcolepsy symptoms. Stressful situations, such as the loss of a loved one or major life changes, can disrupt sleep patterns and exacerbate the symptoms of narcolepsy. It is believed that stress may disrupt the delicate balance of neurotransmitters involved in regulating wakefulness and sleep, leading to increased daytime sleepiness and other symptoms.
While environmental triggers can initiate the manifestation of narcolepsy symptoms, it is important to note that not everyone who encounters these triggers will develop the disorder. Genetic susceptibility plays a crucial role in determining how an individual responds to these environmental factors. Certain genes, such as those related to immune system function and hypocretin production, influence an individual’s vulnerability to developing narcolepsy when exposed to environmental triggers.
Understanding the interplay between genetic susceptibility and environmental triggers can help in the management and prevention of narcolepsy. By identifying individuals who may be at a higher risk due to genetic factors, healthcare professionals can provide targeted interventions and support to minimize the impact of environmental triggers. Additionally, raising awareness about potential triggers and implementing stress management techniques can contribute to better overall management for individuals with narcolepsy.
Genetic Counseling for Narcolepsy
Genetic counseling can be a valuable resource for individuals and families affected by narcolepsy. Genetic counselors are healthcare professionals who specialize in the field of genetics and provide guidance and support to individuals seeking understanding about the genetic factors involved in certain conditions. In the case of narcolepsy, genetic counseling can help educate individuals about the inheritance patterns and genetic risks associated with the disorder.
During a genetic counseling session for narcolepsy, a counselor will typically gather a detailed family history to assess the likelihood of an inherited component. They may also discuss the known genetic factors associated with narcolepsy, such as the HLA genes, which have been linked to an increased risk of developing the disorder. The counselor will explain the various inheritance patterns that may occur, including autosomal dominant inheritance, autosomal recessive inheritance, and polygenic inheritance. Understanding the inheritance patterns can help individuals determine the likelihood of passing on the condition to future generations.
In addition to discussing the genetic aspects of narcolepsy, genetic counselors can also provide information about available testing options. While there is no specific genetic test for narcolepsy, genetic testing may be recommended in certain cases to help identify any underlying genetic variations that could contribute to the disorder. However, it’s important to note that genetic testing cannot definitively diagnose narcolepsy, as the disorder is complex and likely involves a combination of genetic and environmental factors.
Genetic counselors can also address the emotional and psychological aspects of living with narcolepsy. They can provide support, resources, and coping strategies for managing the impact of the disorder on daily life. Additionally, they can help individuals make informed decisions about family planning and discuss options such as preimplantation genetic testing or adoption.
It is important to remember that genetic counseling is a personalized process, and each individual’s experience and needs may vary. The information and guidance provided by genetic counselors can empower individuals and families to make informed healthcare decisions and better understand the genetic aspects of narcolepsy. If you or a loved one is living with narcolepsy and seeking more information or support, consulting a genetic counselor may be a beneficial step to consider.
Conclusion
In conclusion, the role of genetics in narcolepsy is becoming increasingly evident. While the exact genes and mechanisms involved in narcolepsy susceptibility are still being studied, research has shown that genetic factors play a significant role in the development of this complex neurological disorder. Familial aggregation, HLA alleles, and genome-wide association studies have provided valuable insights into the genetic component of narcolepsy.
The inheritance patterns of narcolepsy can vary and include autosomal dominant, autosomal recessive, and polygenic inheritance. Understanding these patterns and the underlying genetic mechanisms can help in the diagnosis, treatment, and genetic counseling of narcolepsy patients.
Genetic research has also revealed specific dysfunctions in the orexin system and mutations in hypocretin receptors as contributing factors to narcolepsy. These findings have provided crucial insights into the genetic mechanisms that underlie the disorder.
It is important to note that while genetics play a significant role, environmental triggers are also thought to interact with genetic susceptibility in the development of narcolepsy. Further research is needed to elucidate the complex interplay between genetics and environmental factors.
Genetic counseling for narcolepsy can be beneficial, especially for individuals with a family history of the disorder. Genetic counselors can provide information about the inheritance patterns, the risks of passing on narcolepsy to future generations, and support individuals in making informed decisions regarding family planning.
In conclusion, the study of genetics in narcolepsy is a rapidly evolving field that holds promise for improved understanding, diagnosis, and treatment of this enigmatic condition. By unraveling the genetic components of narcolepsy, we can better support individuals affected by this disorder and work towards developing personalized therapeutic approaches in the future.
Frequently Asked Questions
1. Can narcolepsy be inherited?
Yes, there is evidence to suggest that narcolepsy has a genetic component. Certain genes, such as HLA genes, have been found to be associated with an increased risk of developing narcolepsy.
2. What are the common symptoms of narcolepsy?
The common symptoms of narcolepsy include excessive daytime sleepiness, sudden loss of muscle tone (cataplexy), hallucinations, sleep paralysis, and disrupted nighttime sleep.
3. Can narcolepsy be cured?
Currently, there is no cure for narcolepsy. However, symptoms can be managed through a combination of medication, lifestyle changes, and behavioral therapy to improve overall quality of life.
4. How is narcolepsy diagnosed?
Narcolepsy is diagnosed through a combination of medical history, physical examination, sleep studies (polysomnography and multiple sleep latency tests), and other specialized tests to assess the presence of certain biomarkers.
5. Are there any triggers for narcolepsy symptoms?
Yes, narcolepsy symptoms can be triggered by factors such as stress, strong emotions, sudden changes in sleep schedule, and certain medications.
6. Can narcolepsy be mistaken for other sleep disorders?
Yes, narcolepsy can sometimes be mistaken for other sleep disorders, such as sleep apnea. However, a thorough evaluation by a sleep specialist can help differentiate narcolepsy from other conditions.
7. Can narcolepsy be dangerous?
Narcolepsy can pose risks to personal safety, especially when excessive sleepiness or cataplexy episodes occur during activities like driving or operating machinery. It is important for individuals with narcolepsy to take appropriate precautions to minimize these risks.
8. Is narcolepsy more common in certain populations?
Narcolepsy occurs worldwide and is found in people of all ethnic backgrounds. However, some studies have suggested that certain ethnic groups, such as individuals of African or Asian descent, may have a higher prevalence of narcolepsy.
9. Can narcolepsy develop later in life?
While narcolepsy often begins during adolescence or young adulthood, it can develop at any age, including later in life. However, the symptoms and their severity may vary depending on the age of onset.
10. Can narcolepsy be managed without medication?
While medication is often used to manage narcolepsy symptoms, lifestyle modifications such as maintaining a regular sleep schedule, practicing good sleep hygiene, and avoiding excessive caffeine and alcohol intake can also help improve symptoms and overall well-being.