Do you ever wonder how certain brain processes can impact your ability to stay awake and alert during the day? Well, in this article, we will delve into the fascinating world of narcolepsy and explore the scientific basis behind this neurological disorder. Narcolepsy is a condition characterized by excessive daytime sleepiness and sudden, uncontrollable bouts of sleep. But what exactly causes narcolepsy and how does it affect the intricate workings of the brain? Join us on this journey as we uncover the mysteries of narcolepsy and shed light on the science behind its impact on the brain.
What is Narcolepsy?

Narcolepsy is a neurological disorder characterized by sudden and uncontrollable bouts of sleepiness during the day. People with narcolepsy often experience excessive daytime sleepiness, regardless of the quality and duration of their nighttime sleep. This overwhelming and persistent sleepiness can make it challenging for individuals with narcolepsy to stay awake and alert, leading to difficulty in carrying out daily activities. Along with excessive sleepiness, narcolepsy can also be accompanied by other symptoms such as cataplexy, sleep paralysis, and hallucinations. While the exact cause of narcolepsy is still not fully understood, researchers have discovered a link between narcolepsy and certain genetic factors as well as autoimmune responses. To learn more about the genetic aspects of narcolepsy, you can refer to our article on the role of genetics in narcolepsy inheritance. Additionally, if you’re curious about how narcolepsy presents in children and the steps involved in its diagnosis and intervention, you can check out our article on narcolepsy in children.
The Brain and Sleep
Understanding the relationship between the brain and sleep is crucial in comprehending the complexities of narcolepsy. The brain plays a vital role in regulating the sleep-wake cycle and various stages of sleep. During a typical night, we cycle through different sleep stages, with each stage serving a distinct purpose. One of the key stages is Rapid Eye Movement (REM) sleep, which is associated with vivid dreams and increased brain activity. REM sleep is essential for cognitive functioning, memory consolidation, and emotional processing. It is during this stage that most individuals experience muscle paralysis, preventing them from physically acting out their dreams. To explore the similarities and differences between narcolepsy and other sleep disorders such as sleep apnea, you can refer to our article on narcolepsy and sleep apnea.
Normal Sleep Patterns
Normal sleep patterns are an essential part of maintaining overall health and well-being. When we sleep, our bodies go through different stages that repeat in a cyclical pattern throughout the night. These stages can be categorized into two main types: non-rapid eye movement (NREM) sleep and rapid eye movement (REM) sleep.
During NREM sleep, which consists of three stages (N1, N2, and N3), our bodies gradually relax, and brain activity slows down. In N1, also known as the transition stage, we are in a light sleep state and can easily be awakened. N2 is a deeper sleep stage where our heart rate and body temperature decrease. It is during N3, also called slow-wave sleep, that our bodies experience deep and restorative sleep. During this stage, our muscles relax, and important processes such as tissue repair and growth occur.
REM sleep, on the other hand, is a unique sleep stage characterized by rapid eye movements, increased brain activity, and vivid dreaming. It is in REM sleep that our brains become highly active, similar to when we are awake. Our heart rate and breathing may become irregular, and our muscles become temporarily paralyzed to prevent us from acting out our dreams. REM sleep is crucial for cognitive functions like memory consolidation and emotional regulation.
The cycling between NREM and REM sleep stages typically occurs multiple times throughout the night, with each cycle lasting about 90 minutes. This alternating pattern of sleep stages is essential for achieving a balanced and restorative sleep. Disruptions in these normal sleep patterns, as seen in conditions like narcolepsy, can profoundly affect an individual’s daytime functioning and overall quality of life. Understanding these normal sleep patterns is crucial in grasping the impact that narcolepsy, and its disruption of these patterns, can have on the brain and body.
Rapid Eye Movement (REM) Sleep
Rapid Eye Movement (REM) sleep is one of the key stages of the sleep cycle that plays a crucial role in various brain and bodily functions. During REM sleep, the brain becomes highly active, and vivid dreams often occur. This stage is characterized by rapid eye movements, hence the name. It is in this stage that most of the body’s rejuvenation and restoration processes take place. REM sleep typically occurs multiple times throughout the night, with each cycle lasting approximately 90-120 minutes.
To further understand the significance of REM sleep, let’s take a closer look at some of its key features:
1. Muscle Paralysis: During REM sleep, the body undergoes a temporary state of muscle paralysis, known as atonia. This paralysis prevents individuals from physically acting out their dreams and ensures that they remain still during this active stage of sleep.
2. Brain Activation: The brain’s activity during REM sleep is remarkably similar to that of wakefulness. It is a state of heightened mental activity, with increased neural firing and activity in regions associated with emotions, memory consolidation, and learning.
3. Dreaming: REM sleep is strongly associated with the occurrence of vivid dreams. These dreams often involve complex storylines, vivid imagery, and heightened emotions. The exact purpose and function of dreaming are still not fully understood, but it is believed to be essential for cognitive processes and emotional well-being.
4. Memory Consolidation: REM sleep plays a crucial role in memory consolidation, where information and experiences from the day are processed and stored in long-term memory. This stage is believed to enhance learning and improve memory performance.
5. Restoration and Growth: REM sleep is vital for the restoration and growth of the body. It is during this stage that the brain replenishes neurotransmitters, repairs cellular damage, and promotes hormone regulation. REM sleep is particularly important for the development and maintenance of healthy brain function.
Understanding the intricacies of REM sleep is essential in comprehending the impact of narcolepsy on the sleep cycle and the brain. People with narcolepsy often experience disrupted REM sleep, leading to fragmented sleep patterns and an increased frequency of sleep attacks. To learn more about the differences and similarities between narcolepsy and other sleep disorders, such as sleep apnea, you can refer to our article on narcolepsy vs. sleep apnea.
The Role of Orexin
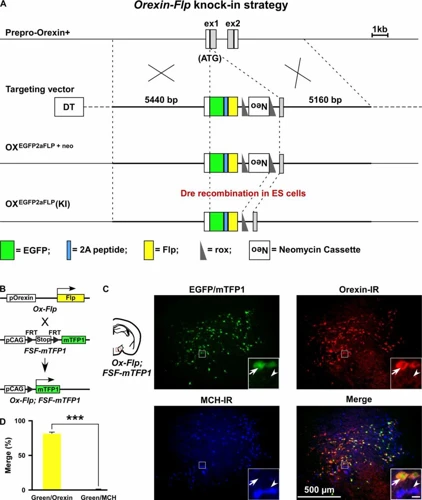
Orexin, also known as hypocretin, is a neuropeptide that plays a crucial role in regulating wakefulness and sleep. Produced in the hypothalamus, orexin acts as a key player in promoting wakefulness and maintaining a stable sleep-wake cycle. It stimulates the areas of the brain responsible for arousal and helps to stabilize the transitions between different stages of sleep. Individuals with narcolepsy often have a deficiency or absence of orexin, which disrupts their ability to regulate sleep and wakefulness. The lack of orexin leads to fragmented and unrefreshing sleep, as well as excessive daytime sleepiness. Researchers have identified a strong link between orexin deficiency and narcolepsy, particularly in cases of type 1 narcolepsy. This discovery has not only deepened our understanding of the neurobiology of narcolepsy but has also opened up new avenues for potential treatments targeting the restoration of orexin levels in the brain.
Orexin and Wakefulness
Orexin, also known as hypocretin, plays a crucial role in regulating wakefulness and sleep. It is a neuropeptide produced in the hypothalamus, a region of the brain responsible for controlling various functions, including sleep and wakefulness. Orexin acts as a stimulant, promoting wakefulness and preventing excessive sleepiness.
Here are some key points about the role of orexin in wakefulness:
1. Signaling Wakefulness: Orexin neurons in the hypothalamus send signals to other parts of the brain, such as the arousal centers in the brainstem and the cortex, to promote wakefulness. This activation helps maintain a state of alertness and vigilance.
2. Modulating Sleep-Wake Cycle: Orexin is involved in regulating the sleep-wake cycle by promoting wakefulness during the day and inhibiting sleep during the night. It helps stabilize the transition between sleep and wakefulness.
3. Energy Balance and Appetite Control: In addition to promoting wakefulness, orexin also regulates energy balance and appetite. It influences feeding behavior, with low levels of orexin leading to reduced food intake. This dual role of orexin highlights its impact on both sleep and metabolism.
4. Interaction with Neurotransmitters: Orexin interacts with various neurotransmitters in the brain, including dopamine, serotonin, and norepinephrine. These interactions help regulate arousal, mood, and other physiological processes associated with wakefulness.
Understanding the role of orexin in wakefulness is crucial when studying narcolepsy since individuals with narcolepsy often have low levels of orexin. The next section will explore the link between orexin and narcolepsy in more detail.
The Link between Orexin and Narcolepsy
The link between orexin and narcolepsy is a significant area of research in understanding the underlying mechanisms of this sleep disorder. Orexin, also known as hypocretin, is a neuropeptide that plays a crucial role in regulating wakefulness and sleep. It is produced by a group of cells in the hypothalamus, a region of the brain responsible for various physiological functions. These orexin-producing cells send signals to other parts of the brain involved in wakefulness, such as the arousal centers.
In individuals with narcolepsy, there is a deficiency or absence of orexin due to the destruction of these orexin-producing cells. This deficiency disrupts the normal sleep-wake cycle, leading to excessive daytime sleepiness and other narcoleptic symptoms. The exact cause of the destruction of these orexin-producing cells is still unclear, but it is believed to be an autoimmune response in most cases.
The link between orexin deficiency and narcolepsy is well-established, and it has contributed to the development of treatments for this sleep disorder. Medications that mimic the effects of orexin or enhance its activity are used to manage narcolepsy symptoms. These medications help regulate sleep and wakefulness, promoting better daytime alertness in individuals with narcolepsy.
Understanding the link between orexin and narcolepsy has paved the way for targeted therapies and further studies into the underlying causes of this neurological condition. Continued research in this area holds the potential for future breakthroughs in the treatment and management of narcolepsy.
Causes of Narcolepsy
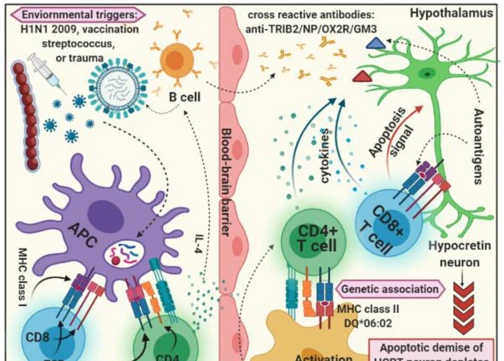
Narcolepsy can be caused by a combination of genetic predisposition and autoimmune response. It is believed that certain genes may play a role in increasing the risk of developing narcolepsy. Research has identified a specific gene variant called HLA-DQB1*06:02 that is associated with a higher susceptibility to narcolepsy. This gene variant is found in a majority of individuals with narcolepsy with cataplexy, highlighting the role of genetics in this disorder. Additionally, narcolepsy is linked to an autoimmune response, where the immune system mistakenly attacks cells that produce a neuropeptide called orexin. Orexin is responsible for regulating wakefulness and maintaining a stable sleep-wake cycle. The destruction of orexin-producing cells leads to a deficiency of orexin in the brain, resulting in the symptoms of narcolepsy. The precise triggers for this autoimmune response are not fully understood, but a combination of genetic and environmental factors is thought to contribute to its development.
Genetic Predisposition
Genetic predisposition plays a significant role in the development of narcolepsy. Multiple studies have indicated that certain genes are associated with an increased risk of developing this neurological disorder. One particular gene that has been extensively studied in relation to narcolepsy is the HLA gene complex. Specifically, variations in the HLA-DQB1 gene have been found to be strongly associated with an increased susceptibility to narcolepsy. These genetic variations can lead to a malfunction in the immune response, ultimately affecting the production of hypocretin/orexin, a neuropeptide that plays a crucial role in regulating wakefulness and sleep. Research has shown that individuals with narcolepsy often have significantly lower levels of hypocretin/orexin in their cerebrospinal fluid, further supporting the genetic link. While genetic predisposition alone may not cause narcolepsy, it significantly increases the likelihood of developing the disorder. It’s important to note that having these genetic variations does not guarantee the development of narcolepsy, as other factors such as environmental triggers and autoimmune responses also come into play. Further research is still needed to fully understand the complex interplay between genetics and narcolepsy development.
Autoimmune Response
The autoimmune response is believed to play a significant role in the development of narcolepsy. In individuals with narcolepsy, the immune system mistakenly targets and attacks certain cells in the brain that produce a neuropeptide called hypocretin, also known as orexin. Hypocretin is responsible for regulating wakefulness and maintaining a stable sleep-wake cycle. When the immune system attacks these hypocretin-producing cells, it leads to a significant reduction in the levels of hypocretin in the brain. This deficiency of hypocretin disrupts the normal sleep-wake cycle, resulting in the symptoms associated with narcolepsy. Research suggests that a specific type of immune cell known as T cells may be involved in this autoimmune response. In individuals with narcolepsy, their T cells may mistakenly recognize the hypocretin-producing cells as foreign, triggering an immune response against them. The exact triggers for this autoimmune response are still under investigation, but certain factors such as viral infections and environmental exposures have been proposed as potential contributors. Understanding the autoimmune response in narcolepsy is crucial for developing targeted treatments that aim to modulate the immune system and potentially restore normal hypocretin levels in the brain.
Brain Abnormalities in Narcolepsy
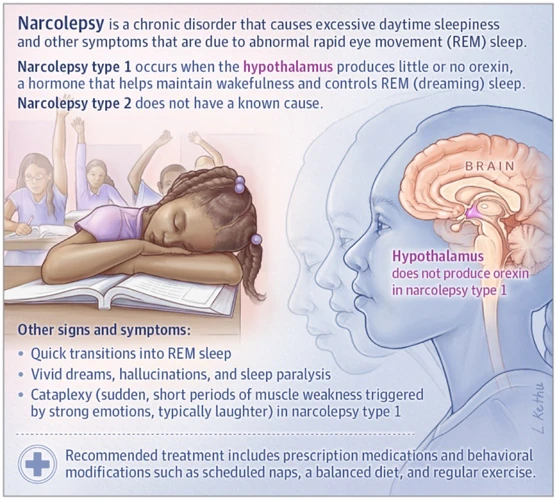
In individuals with narcolepsy, there are notable brain abnormalities that contribute to the development and manifestation of the disorder. One significant area of dysfunction is the hypothalamus, which plays a crucial role in regulating sleep and wakefulness. In people with narcolepsy, the hypothalamus fails to produce adequate amounts of a neuropeptide called orexin (also known as hypocretin), which is responsible for promoting wakefulness. This deficiency is believed to be a result of an autoimmune response that selectively destroys the orexin-producing cells in the hypothalamus. Another abnormality in the brain of those with narcolepsy involves neurotransmitters such as dopamine, norepinephrine, and serotonin. These neurotransmitters, which help regulate sleep-wake cycles, may be imbalanced in individuals with narcolepsy. Interestingly, these brain abnormalities help explain the core symptoms of narcolepsy, including excessive daytime sleepiness and disrupted REM sleep. The precise interplay between these brain irregularities and the development of narcolepsy is an ongoing area of scientific research and one that offers hope for the development of more effective treatments in the future.
Hypothalamus Dysfunction
Hypothalamus dysfunction plays a significant role in the development and manifestation of narcolepsy. The hypothalamus, a region deep within the brain, is responsible for regulating various functions, including sleep-wake cycles. In individuals with narcolepsy, there is evidence of abnormalities in the hypothalamus, specifically in the production of a neuropeptide called hypocretin, or orexin. Hypocretin plays a crucial role in promoting wakefulness and regulating REM sleep. However, in narcolepsy, there is a deficiency of hypocretin due to the destruction of the cells that produce it. This deficiency disrupts the balance between wakefulness and sleep, leading to excessive sleepiness during the day and disturbed nighttime sleep. It is believed that this dysfunction in the hypothalamus is responsible for the disrupted sleep patterns and irregular transitions between sleep stages that are characteristic of narcolepsy.
Neurotransmitter Imbalance
Neurotransmitter imbalance plays a crucial role in the development and manifestation of narcolepsy. Neurotransmitters are chemical messengers that facilitate communication between nerve cells in the brain. In narcolepsy, there is an imbalance in the levels of certain neurotransmitters, particularly hypocretin (also known as orexin), dopamine, and serotonin. Hypocretin is a neurotransmitter that regulates wakefulness and helps in maintaining arousal. In patients with narcolepsy, there is a significant decrease in the production of hypocretin due to the destruction of hypocretin-producing cells in the brain. This deficiency disrupts the balance between sleep and wakefulness, leading to excessive daytime sleepiness and other symptoms of narcolepsy.
Similarly, dopamine and serotonin, two other important neurotransmitters, play a role in sleep regulation. Dopamine helps in promoting wakefulness, while serotonin contributes to the regulation of sleep stages. In individuals with narcolepsy, there may be abnormalities in the production, release, or reuptake of these neurotransmitters, further contributing to the disruption of sleep-wake cycles.
The exact mechanisms behind neurotransmitter imbalance in narcolepsy are still being studied, but it is believed that genetic factors, autoimmune responses, and abnormalities in the brain’s receptors and transporters are involved. By understanding the role of neurotransmitters in narcolepsy, researchers and healthcare professionals can develop targeted treatments that aim to restore the balance of these chemicals in the brain.
Symptoms of Narcolepsy

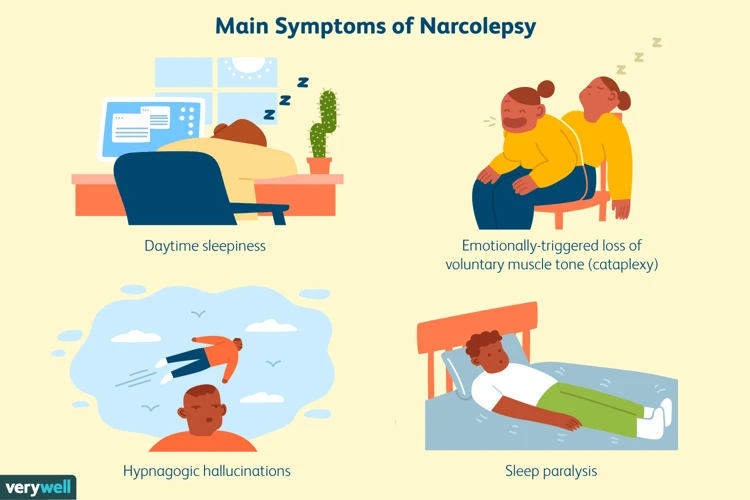
Narcolepsy is a complex disorder, often accompanied by a range of symptoms that can significantly impact an individual’s daily life. One of the primary symptoms of narcolepsy is excessive daytime sleepiness (EDS), which is characterized by an overwhelming and persistent urge to sleep during the day, even after a full night’s sleep. Individuals with narcolepsy may struggle to stay awake and alert, making it challenging to concentrate and engage in activities. Another symptom is cataplexy, which involves a sudden loss of muscle tone, resulting in temporary muscle weakness or total paralysis. This can be triggered by strong emotions such as laughter or anger, and it can significantly disrupt daily functioning. Sleep paralysis is also a common occurrence in narcolepsy, where individuals experience a temporary inability to move or speak while falling asleep or waking up. Hallucinations can accompany sleep paralysis, with vivid and sometimes frightening images or sounds. These symptoms can vary in severity and frequency among individuals with narcolepsy, making it essential to seek proper diagnosis and treatment.
Excessive Daytime Sleepiness
Excessive daytime sleepiness (EDS) is a hallmark symptom of narcolepsy and is the most common and pervasive complaint among individuals with this sleep disorder. EDS refers to an overwhelming and persistent feeling of sleepiness that occurs during the daytime, regardless of the amount of sleep obtained the previous night. It is important to note that EDS in narcolepsy is not the same as feeling tired or fatigued due to a lack of sleep, as it is a constant and uncontrollable need to sleep throughout the day.
To better understand the impact of EDS, let’s take a look at some of its key features and effects:
1. Recurrent Sleep Attacks: People with narcolepsy often experience sudden and irresistible urges to sleep, known as sleep attacks. These sleep attacks can occur at any time, even during important tasks or activities like driving, working, or socializing. These episodes of uncontrollable sleepiness can significantly disrupt daily life and may lead to accidents or diminished productivity.
2. Difficulty Maintaining Wakefulness: Individuals with narcolepsy may find it challenging to stay awake and alert for extended periods, regardless of the level of stimulation around them. Even during engaging or stimulating activities, such as watching a movie or participating in a conversation, they may struggle to maintain wakefulness.
3. Microsleep Episodes: Microsleep refers to brief, involuntary episodes of sleep that last for a few seconds up to a minute. These episodes often occur spontaneously and involuntarily, interrupting normal wakefulness. Microsleep episodes can be particularly dangerous if they happen during activities that require attention, such as driving or operating machinery.
4. Impact on Daily Functioning: The excessive daytime sleepiness associated with narcolepsy can significantly impair an individual’s ability to perform daily tasks effectively. Simple activities such as reading, studying, or watching television can become a struggle due to the constant need for sleep. People with EDS may also feel mentally foggy, which can further affect their overall cognitive functioning.
5. Emotional Consequences: EDS can also have emotional consequences, as individuals with narcolepsy may feel frustrated, depressed, or anxious due to their ongoing struggle to stay awake and alert. The impact of EDS on social interactions and relationships can also lead to feelings of isolation and reduced quality of life.
Excessive daytime sleepiness is a defining characteristic of narcolepsy and can have a profound impact on an individual’s daily life. Effective management strategies, such as medication and lifestyle changes, can help alleviate the symptoms and improve wakefulness. You can explore various treatment options and coping strategies for narcolepsy in our article on treatment options for narcolepsy.
Cataplexy
Cataplexy is a unique symptom of narcolepsy that involves a sudden loss of muscle tone or control. It is often triggered by intense emotions such as laughter, surprise, or anger. During a cataplectic episode, individuals may experience a temporary weakening of their muscles, leading to partial or complete collapse. This can range from a subtle drooping of facial muscles to a complete inability to move. While cataplexy can vary in severity and duration, it generally lasts for a few seconds to a couple of minutes.
The underlying cause of cataplexy lies in the disruption of the brain’s normal control over muscle movement. Normally, during wakefulness, the brain releases neurotransmitters that inhibit muscle activity, allowing us to remain upright and mobile. However, in individuals with narcolepsy, a loss of orexin-producing cells in the brain leads to a dysfunction in the regulation of these neurotransmitters, particularly the neurotransmitter hypocretin.
During cataplexy episodes, there is a sudden decrease in hypocretin levels, which results in the temporary loss of muscle tone. This decrease often corresponds with the triggering emotion, indicating the direct link between emotional response and muscle control. It is important to note that not all individuals with narcolepsy experience cataplexy, and its occurrence can vary from person to person.
Cataplexy can significantly impact daily life and social interactions for those with narcolepsy. The fear of experiencing an episode can lead to heightened anxiety and avoidance of situations that may trigger emotions. However, with proper diagnosis and management, cataplexy can be effectively controlled through medication and lifestyle modifications. Techniques such as regular sleep schedules, stress management, and avoiding emotional triggers can help minimize the frequency and severity of cataplectic episodes, allowing individuals to regain control over their muscles and resume their daily activities.
Sleep Paralysis and Hallucinations
Sleep paralysis and hallucinations are common symptoms experienced by individuals with narcolepsy. During sleep paralysis, a person is temporarily unable to move or speak while transitioning between sleep and wakefulness. This often occurs when falling asleep or waking up. Sleep paralysis can be accompanied by a sense of pressure on the chest, making it difficult to breathe. These episodes can be distressing and disorienting for the individual.
Hallucinations, on the other hand, involve vivid and often bizarre sensory experiences that occur during the transition into or out of sleep. These hallucinations can be visual, auditory, or tactile in nature. Individuals may see vivid images, hear voices or sounds that aren’t there, or feel sensations such as tingling or crawling on the skin. These hallucinations can be extremely vivid and realistic, blurring the line between dreams and reality.
It’s important to note that sleep paralysis and hallucinations are not exclusive to narcolepsy and can occur in other sleep disorders as well. However, the combination of excessive daytime sleepiness, cataplexy, and these symptoms is often indicative of narcolepsy.
It is believed that these experiences are a result of disruptions in the normal sleep-wake cycle and the intrusion of dream activity into wakefulness. The exact mechanisms behind sleep paralysis and hallucinations in narcolepsy are not fully understood, but they may be related to the dysfunction of the brain regions responsible for regulating sleep and wakefulness.
Living with sleep paralysis and hallucinations can be challenging, as they can disrupt sleep and lead to anxiety or fear of falling asleep. Developing coping strategies and seeking support from healthcare professionals can help individuals manage these symptoms effectively.
Diagnosing Narcolepsy
Diagnosing narcolepsy involves a comprehensive evaluation of a person’s medical history, physical examination, and specific tests to confirm the presence of the disorder. During the medical history assessment, healthcare professionals will inquire about the individual’s sleep patterns, daytime sleepiness, and any accompanying symptoms like cataplexy or sleep paralysis. They may also assess for the presence of any underlying medical conditions or medications that could be contributing to the symptoms. A physical examination may be conducted to rule out other potential causes of excessive sleepiness. Sleep studies, such as polysomnography and multiple sleep latency tests, are the main diagnostic tools for narcolepsy. Polysomnography monitors various physiological parameters during sleep to assess the quality and patterns of sleep, while the multiple sleep latency test measures the time it takes for a person to fall asleep in a controlled environment. These tests help determine the presence of rapid eye movement (REM) sleep abnormalities and the tendency for excessive daytime sleepiness. By combining the findings from the medical history, physical examination, and sleep studies, healthcare professionals can make an accurate diagnosis and develop an appropriate treatment plan tailored to the individual’s needs.
Medical History and Physical Examination
During the diagnostic process of narcolepsy, a thorough medical history and physical examination are essential. The healthcare provider will begin by taking a detailed medical history, which may involve asking questions about the patient’s sleep patterns, daytime sleepiness, and the presence of other symptoms such as cataplexy or sleep paralysis. This information helps to establish a baseline understanding of the individual’s symptoms and enables the physician to identify any potential underlying causes.
In addition to the medical history, a physical examination is conducted to assess the patient’s overall health and to rule out any other underlying conditions that may be contributing to the symptoms. This examination may include checking blood pressure, heart rate, and neurologic function. The healthcare provider will also look for any signs of physical abnormalities that may be associated with narcolepsy.
In order to provide comprehensive and accurate diagnosis, the doctor may refer the individual to a sleep specialist for further evaluation. A sleep specialist is trained to conduct specialized tests to assess the individual’s sleep patterns and overall sleep-wake balance. These tests may include polysomnography, which records brain activity, eye movements, and muscle activity during sleep, as well as multiple sleep latency testing, which measures the individual’s propensity for falling asleep during the day.
The combination of a detailed medical history and a thorough physical examination, along with possible consultation with a sleep specialist, plays a crucial role in the accurate and timely diagnosis of narcolepsy. It allows healthcare professionals to gather vital information and determine the most appropriate course of action for managing the symptoms and improving the quality of life for individuals with narcolepsy.
Sleep Studies
Sleep studies, also known as polysomnography, play a crucial role in diagnosing narcolepsy. These studies allow healthcare professionals to monitor and evaluate various physiological aspects of sleep, providing valuable insights into the sleep patterns and abnormalities present in individuals with narcolepsy. During a sleep study, a patient spends the night in a specialized sleep laboratory, where their sleep is closely monitored and recorded by a team of sleep technicians and experts.
Polysomnography involves the use of multiple sensors and electrodes that are strategically placed on the patient’s body to measure different physiological parameters. These include brain waves (EEG), eye movements, muscle activity, heart rate, and breathing patterns. This comprehensive data helps in identifying the different stages of sleep, including REM (rapid eye movement) sleep.
In the case of narcolepsy, the results of a sleep study can often reveal certain characteristic patterns. For example, individuals with narcolepsy tend to enter REM sleep more quickly than individuals without the condition. This means that they may experience episodes of REM sleep occurring unexpectedly throughout the day, even during wakefulness. This finding, along with other abnormalities observed during the sleep study, can aid in confirming a diagnosis of narcolepsy.
In addition to polysomnography, other specialized tests like the Multiple Sleep Latency Test (MSLT) may be conducted to further evaluate daytime sleepiness and the tendency to enter REM sleep. The MSLT involves measuring the time it takes for an individual to fall asleep in a comfortable and quiet environment during several scheduled naps throughout the day. Individuals with narcolepsy typically exhibit shorter sleep onset times during these naps, providing further evidence of their excessive daytime sleepiness.
Sleep studies, including polysomnography and the MSLT, are essential tools for diagnosing narcolepsy. By analyzing the data obtained from these tests, healthcare professionals can gain a comprehensive understanding of a patient’s sleep patterns and identify any abnormalities that may be indicative of narcolepsy.
Treatment Options for Narcolepsy

When it comes to treating narcolepsy, there are various options available to help manage the symptoms and improve quality of life. Medications play a crucial role in the treatment of narcolepsy and are often prescribed to help regulate sleep-wake cycles. Stimulants like modafinil and armodafinil are commonly prescribed to promote wakefulness during the day. Another class of medication called sodium oxybate is often used to improve nighttime sleep and reduce symptoms such as cataplexy. In addition to medications, making lifestyle changes can also be beneficial in managing narcolepsy. Establishing a regular sleep schedule, avoiding caffeine and alcohol, and practicing good sleep hygiene can all contribute to better sleep quality. Supportive therapies such as cognitive-behavioral therapy (CBT) and scheduled napping can also be helpful in managing the symptoms of narcolepsy. It is important to work closely with a healthcare professional to determine the most suitable treatment plan for individual needs and to ensure ongoing support and monitoring.
Medications
Medications play a crucial role in the management of narcolepsy. There are several drugs available that can help alleviate the symptoms and improve the quality of life for individuals with this condition. One commonly prescribed medication is Modafinil. Modafinil is a stimulant that promotes wakefulness and helps combat excessive daytime sleepiness. It works by affecting certain chemicals in the brain that regulate sleep-wake cycles. Another medication frequently used for narcolepsy is Sodium Oxybate. This medication is taken at night and helps improve nighttime sleep and reduce the occurrence of cataplexy, sleep paralysis, and hallucinations. It is important to note that medications for narcolepsy should be prescribed by a qualified healthcare professional, as they require careful monitoring and adjustment to ensure effectiveness and minimize potential side effects. In addition to these medications, lifestyle adjustments and support therapies are often recommended as part of a comprehensive treatment plan for narcolepsy.
Lifestyle Changes
Lifestyle changes can play an important role in managing narcolepsy symptoms and improving overall quality of life for individuals with this condition. Here are some lifestyle modifications that can be beneficial:
1. Establish a Regular Sleep Schedule: Stick to a consistent sleep schedule by going to bed and waking up at the same time every day. This can help regulate your body’s internal clock and promote better sleep.
2. Create a Sleep-Friendly Environment: Make your bedroom a comfortable space for sleep. Use blackout curtains or an eye mask to block out light, keep the room cool and quiet, and invest in a supportive mattress and pillows.
3. Avoid Stimulants: Limit your intake of caffeine and other stimulants, especially in the afternoon and evening. These substances can interfere with your ability to fall asleep and stay asleep.
4. Manage Stress: Stress can worsen narcolepsy symptoms, so finding effective stress management techniques can be helpful. Consider practicing relaxation exercises, such as deep breathing or meditation, and engage in activities that help you unwind.
5. Take Regular Naps: Short power naps during the day can provide temporary relief from excessive sleepiness. Keep your naps short (around 15-20 minutes) and try to schedule them strategically to avoid interfering with nighttime sleep.
6. Exercise Regularly: Engaging in regular physical activity can improve sleep quality and overall well-being. Aim for at least 30 minutes of moderate-intensity exercise most days of the week, but avoid vigorous workouts close to bedtime.
7. Follow a Healthy Diet: Maintain a nutritious diet that includes whole grains, fruits, vegetables, and lean proteins. Avoid heavy meals or foods high in sugar close to bedtime, as they can disrupt sleep.
8. Stick to a Bedtime Routine: Establish a relaxing bedtime routine to signal to your body that it’s time to wind down and prepare for sleep. This could include activities such as reading a book, taking a warm bath, or practicing gentle stretching.
By incorporating these lifestyle changes into your daily routine, you can support better sleep patterns and minimize the impact of narcolepsy symptoms on your daily life. Remember, it’s important to consult with your healthcare provider for personalized advice and guidance in managing your narcolepsy.
Supportive Therapies
Supportive therapies play a crucial role in managing narcolepsy and improving the quality of life for individuals affected by this condition. These therapies aim to complement other treatment options and help individuals cope with the symptoms of narcolepsy on a daily basis. One commonly used supportive therapy is behavioral interventions, which focus on adopting healthy sleep habits and implementing sleep hygiene practices. This may include establishing a regular sleep schedule, creating a conducive sleep environment, and avoiding stimulants close to bedtime. Another helpful approach is the incorporation of scheduled short naps throughout the day to combat excessive daytime sleepiness. These planned naps can help individuals with narcolepsy manage their sleepiness and increase their wakefulness during the day. Additionally, psychological counseling and cognitive-behavioral therapy (CBT) can be beneficial for addressing the emotional and psychological impact of narcolepsy. These therapies provide individuals with coping strategies and support in managing any anxiety, depression, or stress that may arise due to living with narcolepsy. Finally, support groups and online forums can be valuable resources for individuals to connect with others who are also dealing with narcolepsy. Sharing experiences and receiving support from peers who understand the challenges of living with this condition can be immensely helpful on the journey of managing narcolepsy.
Living with Narcolepsy
Living with narcolepsy can present various challenges, but with the right strategies and support, individuals can effectively manage their symptoms and lead fulfilling lives. One of the key aspects of managing narcolepsy is developing coping strategies to combat excessive daytime sleepiness. This may involve scheduling short naps throughout the day to combat sudden bouts of sleepiness and maintaining a consistent sleep schedule at night. Additionally, incorporating regular exercise and avoiding caffeine and heavy meals close to bedtime can help improve overall sleep quality. It is also essential to adhere to prescribed medications, such as stimulants or antidepressants, as they can greatly enhance wakefulness during the day. Seeking support from healthcare professionals and joining support groups can provide valuable insights and emotional support. With a combination of lifestyle adjustments, medication management, and a strong support system, individuals with narcolepsy can effectively navigate the challenges and live fulfilling lives.
Managing Symptoms
Managing the symptoms of narcolepsy is crucial in order to improve the overall quality of life for individuals living with this condition. While there is no cure for narcolepsy, there are various strategies and treatment options available to help manage its symptoms. One important aspect of symptom management is the use of medications. Stimulants, such as modafinil and armodafinil, can be prescribed to promote wakefulness during the day and combat excessive sleepiness. Additionally, antidepressants, such as selective serotonin reuptake inhibitors (SSRIs), may be used to help manage cataplexy and other symptoms. However, it’s important to note that medication alone is not sufficient and should be accompanied by lifestyle changes to effectively manage narcolepsy symptoms. Establishing a consistent sleep schedule, practicing good sleep hygiene (such as avoiding caffeine and electronic devices before bed), and taking regular short naps throughout the day can all help regulate sleep patterns. Creating an environment conducive to sleep, such as maintaining a cool and dark bedroom, can also promote better sleep quality. Incorporating regular exercise and maintaining a healthy diet can contribute to overall well-being and energy levels. Lastly, establishing a support network and seeking therapy or counseling can be beneficial in managing the emotional and psychological impact of living with narcolepsy. It’s important for individuals with narcolepsy to develop coping mechanisms, prioritize self-care, and seek the necessary support to navigate the challenges associated with this condition.
Support and Coping Strategies
Support and coping strategies play a crucial role in helping individuals with narcolepsy manage their symptoms and improve their quality of life. Here are some strategies and resources that can provide support to those living with narcolepsy:
1. Support Groups: Joining a support group can be beneficial for individuals with narcolepsy. It provides an opportunity to connect with others who understand the challenges and experiences associated with the condition. Sharing stories, tips, and coping mechanisms can offer emotional support and a sense of community.
2. Education and Awareness: Learning more about narcolepsy can help individuals and their loved ones better understand the condition. Knowledge about the disorder can also reduce misconceptions and stigma surrounding it. Organizations such as the National Sleep Foundation or Narcolepsy Network provide educational resources and materials for individuals seeking information on narcolepsy.
3. Sleep Hygiene: Maintaining good sleep hygiene is crucial for individuals with narcolepsy. Establishing a regular sleep schedule, creating a relaxing sleep environment, and avoiding stimulants like caffeine and nicotine can help improve sleep quality. Additionally, incorporating relaxation techniques such as meditation or deep breathing exercises before bedtime may aid in falling asleep more easily.
4. Healthy Lifestyle: Adopting a healthy lifestyle can have a positive impact on managing narcolepsy symptoms. Engaging in regular physical activity, maintaining a balanced diet, and managing stress levels can contribute to overall well-being and potentially improve sleep patterns.
5. Workplace Support: Open communication with employers about the condition is essential. Informing supervisors and colleagues about narcolepsy can help create a supportive work environment. Adjustments such as flexible work hours or taking short, scheduled naps during the day may enhance productivity and lessen the impact of excessive daytime sleepiness.
6. Counseling and Therapy: Seeking professional help from counselors or therapists can assist individuals in managing the emotional and psychological aspects of living with narcolepsy. Therapy sessions can provide coping strategies, stress management techniques, and help address any anxiety or depression that may coexist with the condition.
Remember, each individual’s experience with narcolepsy is unique, and it may take time to find the most effective support and coping strategies. Being patient and persistent in exploring different methods can ultimately lead to better management of symptoms, improved well-being, and a more fulfilling life.
Conclusion
In conclusion, narcolepsy is a complex neurological disorder that affects the brain’s ability to regulate sleep-wake cycles. It is characterized by excessive daytime sleepiness, sudden sleep attacks, and other symptoms such as cataplexy, sleep paralysis, and hallucinations. The underlying causes of narcolepsy are still not fully understood, but research suggests a combination of genetic predisposition and autoimmune response may play a role. Despite the challenges that narcolepsy presents, there are treatment options available to manage the symptoms, including medication, lifestyle changes, and supportive therapies. Additionally, individuals with narcolepsy can benefit from adopting strategies to effectively manage their symptoms and seek support from healthcare professionals and support networks. By gaining a deeper understanding of the science behind narcolepsy and the impact it has on the brain, we can improve diagnosis, treatment, and support for individuals living with this condition. Remember, if you suspect that you or someone you know may have narcolepsy, it’s important to consult a healthcare professional for proper evaluation and guidance.
Frequently Asked Questions
FAQs about Narcolepsy
1. Can narcolepsy be mistaken for laziness?
No, narcolepsy is a neurological disorder characterized by excessive sleepiness that is beyond the control of an individual. It is not related to laziness.
2. Is narcolepsy a rare condition?
Narcolepsy is considered a relatively rare condition, affecting approximately 1 in 2,000 people worldwide.
3. Can narcolepsy develop at any age?
While narcolepsy typically develops between the ages of 15 and 30, it can occur at any age, even in young children.
4. Can stress trigger narcolepsy symptoms?
Yes, stress can be a triggering factor for narcolepsy symptoms. It is important for individuals with narcolepsy to manage stress levels effectively.
5. Can narcolepsy cause memory problems?
Yes, narcolepsy can affect memory and cognitive abilities, especially when individuals experience disrupted sleep patterns.
6. Can people with narcolepsy drive safely?
Driving can be challenging for individuals with narcolepsy due to sudden episodes of sleepiness. It is important to discuss driving safety with a healthcare professional.
7. Can narcolepsy be cured?
At present, there is no known cure for narcolepsy. However, its symptoms can be managed through various treatment options.
8. Can medication completely control narcolepsy symptoms?
Medication can help alleviate narcolepsy symptoms and promote wakefulness, but it may not completely eliminate all symptoms.
9. Can narcolepsy affect relationships?
Narcolepsy can have an impact on relationships, as the symptoms can affect daily activities and require understanding and support from loved ones.
10. Can narcolepsy lead to other health complications?
Untreated narcolepsy can potentially lead to other health complications, such as an increased risk of accidents and injuries, depression, and obesity.