Narcolepsy vs. Sleep Apnea: Key Differences and Similarities
Are you constantly feeling tired during the day? Do you struggle to stay awake or find yourself falling asleep unexpectedly? You may be experiencing symptoms of a sleep disorder, such as narcolepsy or sleep apnea. While these conditions may share similarities in terms of their impact on sleep, they have distinct differences in their causes, symptoms, and treatments. In this comprehensive guide, we will delve into the world of narcolepsy and sleep apnea, exploring their definitions, causes, symptoms, diagnosis, and treatment options. By understanding the unique characteristics of each condition, you can gain valuable insights into managing and navigating the challenges that come with these sleep disorders. So, let’s dive in and explore the key differences and commonalities between narcolepsy and sleep apnea.
Understanding Narcolepsy
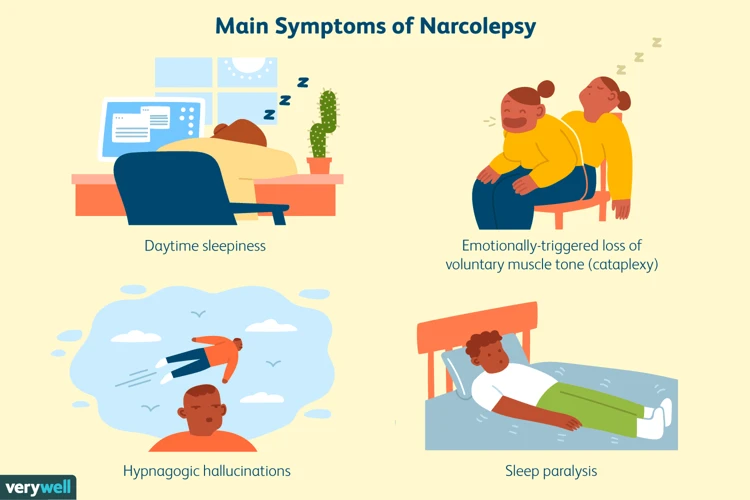
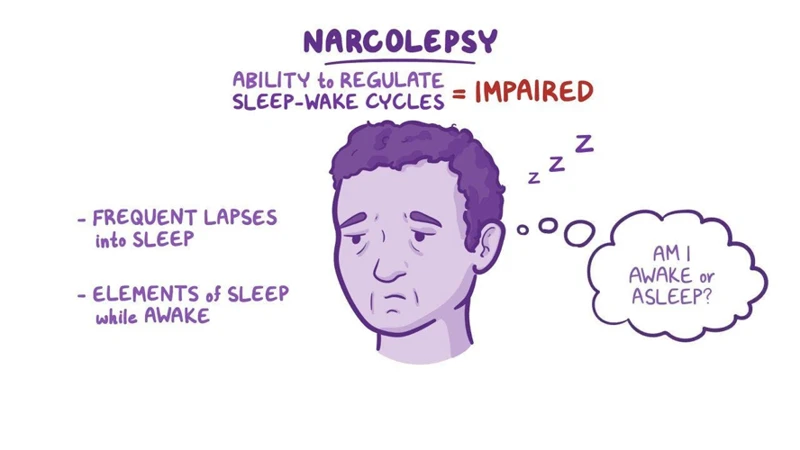
Narcolepsy is a complex neurological disorder that affects the brain’s ability to regulate sleep-wake cycles, resulting in excessive daytime sleepiness and sudden sleep attacks. This condition is often misunderstood and misdiagnosed, leading to significant disruptions in an individual’s daily life. One of the defining characteristics of narcolepsy is experiencing REM (Rapid Eye Movement) sleep symptoms while awake, such as vivid dreaming and hallucinations. These symptoms can be accompanied by a sudden loss of muscle control, known as cataplexy, which is triggered by intense emotions. While narcolepsy is predominantly known for its impact on sleep, it can also have profound effects on mental health and emotional well-being. It is crucial to demystify the misconceptions surrounding narcolepsy and understand its unique manifestations, potential comorbidities, and available interventions to ensure individuals receive proper care and support.
Definition and Overview
Narcolepsy is a neurological sleep disorder characterized by excessive daytime sleepiness and a disruption in the normal sleep-wake cycle. It affects approximately 1 in 2,000 individuals, although the exact prevalence is still uncertain due to underdiagnosis and misdiagnosis. People with narcolepsy often experience overwhelming and uncontrollable sleep attacks during the day, regardless of how much sleep they have had at night. These sleep attacks can occur at any time and in any situation, making it difficult for individuals to perform daily tasks, maintain employment, or engage in social activities.
In addition to excessive daytime sleepiness, narcolepsy is often accompanied by several other symptoms. These may include cataplexy, which is a sudden loss of muscle tone triggered by strong emotions such as laughter, surprise, or anger. Some individuals with narcolepsy may also experience hallucinations and sleep paralysis, characterized by vivid and often frightening dream-like experiences while falling asleep or waking up.
The underlying cause of narcolepsy is not fully understood, but it is thought to involve a combination of genetic and environmental factors. Research has identified a strong association between narcolepsy and a deficiency of a neurotransmitter called hypocretin (also known as orexin), which regulates wakefulness and sleep. This deficiency is thought to be due to an autoimmune process that targets the neurons in the brain responsible for producing hypocretin.
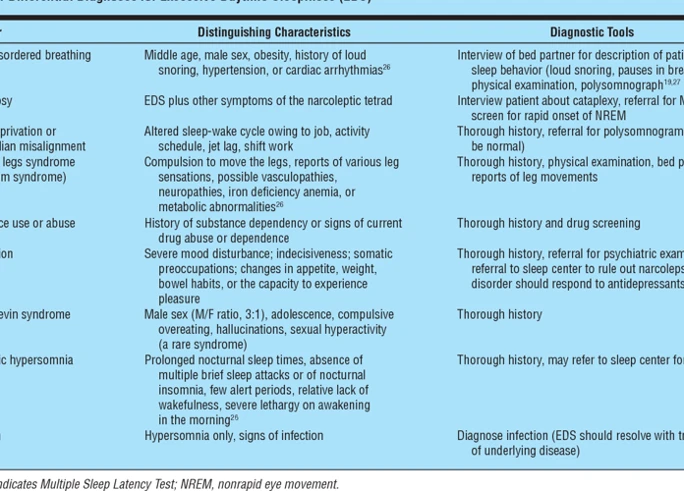
Diagnosing narcolepsy involves a thorough evaluation of a person’s sleep history, symptoms, and the results of specific tests. These may include a multiple sleep latency test (MSLT) to measure the time it takes for a person to fall asleep during the day, and a polysomnography (PSG) to monitor sleep patterns and detect any abnormalities. It is important to receive an accurate diagnosis as early as possible to prevent further disruptions to daily life and seek appropriate treatment.
Treatment for narcolepsy aims to manage symptoms and improve overall quality of life. This may involve a combination of medication, lifestyle adjustments, and support services. Medications, such as stimulants or antidepressants, can help control excessive daytime sleepiness, while medication specifically targeting cataplexy may be prescribed if necessary. Lifestyle changes, such as maintaining a regular sleep schedule, practicing good sleep hygiene, and scheduling short daytime naps, can also help manage symptoms. Additionally, counseling and support groups can provide emotional support and coping strategies for individuals with narcolepsy and their families.
Understanding the definition and overview of narcolepsy is essential in identifying the symptoms, seeking appropriate medical attention, and accessing necessary support and resources. By recognizing the complexities of this sleep disorder, we can promote greater awareness and contribute to improved well-being for individuals living with narcolepsy. To learn more about the connection between narcolepsy, dreaming, and emotional well-being, please refer to our article on the narcolepsy-mental health connection.
Causes and Symptoms
Narcolepsy: The exact cause of narcolepsy is still unknown, but it is believed to be a combination of genetic and environmental factors. Research suggests that narcolepsy may be linked to an abnormality in the brain’s production of a neurotransmitter called hypocretin, which plays a role in regulating wakefulness and sleep. In most cases, narcolepsy develops spontaneously, but it can also be triggered by certain infections or traumatic brain injuries.
The symptoms of narcolepsy can vary in severity from person to person. The hallmark symptom is excessive daytime sleepiness, where individuals feel an overwhelming urge to sleep throughout the day, often at inappropriate times. This can lead to sudden sleep attacks, where individuals may fall asleep without warning, even during activities such as eating, talking, or driving.
In addition to excessive sleepiness, narcolepsy is characterized by other symptoms, including cataplexy, sleep paralysis, hallucinations, and disrupted nighttime sleep. Cataplexy is a sudden loss of muscle tone triggered by intense emotions, such as laughter or surprise. Sleep paralysis occurs when a person is temporarily unable to move or speak upon waking up or falling asleep. Vivid hallucinations may accompany sleep paralysis or occur independently. Nighttime sleep may be fragmented, with frequent awakenings and periods of wakefulness.
Sleep Apnea: Sleep apnea, on the other hand, is primarily caused by a partial or complete obstruction of the airway during sleep. This obstruction leads to repetitive pauses in breathing, lasting for seconds or longer, throughout the night. The most common form of sleep apnea is obstructive sleep apnea (OSA), which occurs when the muscles in the throat relax and collapse, blocking the airflow. Another less common form is central sleep apnea (CSA), where the brain fails to send proper signals to the muscles that control breathing.
The main symptom of sleep apnea is loud and chronic snoring, usually followed by episodes of gasping or choking as breathing is temporarily disrupted. However, snoring does not necessarily indicate sleep apnea, as it can be common in individuals without the disorder. Other symptoms include excessive daytime sleepiness, morning headaches, difficulty concentrating, irritability, and waking up with a dry mouth or sore throat. Sleep apnea can also contribute to the development of other health conditions, such as high blood pressure, heart disease, and diabetes.
It’s important to note that while both narcolepsy and sleep apnea can cause excessive daytime sleepiness, the underlying mechanisms and symptoms differ significantly. Understanding these distinctions is essential for accurate diagnosis and appropriate treatment. For a deeper understanding of narcolepsy and its associated symptom of cataplexy, you can read our article on Demystifying Cataplexy in Narcolepsy. Additionally, if you suspect your child may have narcolepsy, it’s important to recognize the signs and seek early diagnosis and intervention. Learn more about this topic in our article on Narcolepsy in Children: Signs, Diagnosis, and Intervention.
Diagnosis and Treatment
Diagnosing narcolepsy involves a comprehensive evaluation by a healthcare professional specializing in sleep disorders. The process typically begins with a detailed medical history and physical examination to rule out other possible causes of excessive daytime sleepiness. To confirm the diagnosis, several tests may be conducted, including a polysomnogram and multiple sleep latency test (MSLT). The polysomnogram monitors sleep patterns during a full night’s sleep, while the MSLT measures the individual’s ability to fall asleep and enter REM sleep during several short nap opportunities throughout the day. These tests help assess the presence of abnormal sleep patterns characteristic of narcolepsy. Additionally, a healthcare provider may inquire about the frequency and intensity of symptoms and may request a sleep diary, where individuals record their sleep habits and patterns.
Once diagnosed, treatment for narcolepsy typically involves a combination of pharmacological and behavioral interventions. Medications, such as stimulants and selective serotonin reuptake inhibitors (SSRIs), may be prescribed to manage excessive daytime sleepiness, cataplexy, and other associated symptoms. Lifestyle adjustments, such as maintaining a regular sleep schedule, incorporating scheduled naps, and avoiding stimulating substances, like caffeine and alcohol, may also help alleviate symptoms. Cognitive-behavioral therapy (CBT) can be beneficial in addressing the impact of narcolepsy on daily functioning, managing stress, and improving overall sleep quality.
It is important to note that individual treatment plans may vary, and it is essential to work closely with healthcare professionals to find the most effective management approach for each person’s unique needs. Regular follow-up appointments and open communication with healthcare providers are crucial in monitoring symptoms, adjusting treatment as necessary, and ensuring optimal quality of life for individuals with narcolepsy. By engaging in a comprehensive treatment plan, individuals can better manage symptoms and improve their overall well-being.
Understanding Sleep Apnea

Sleep apnea is a common sleep disorder characterized by periods of interrupted breathing during sleep. It occurs when the muscles in the throat temporarily relax and block the airway, leading to brief pauses in breathing called apneas. These interruptions can cause a person to wake up briefly multiple times throughout the night, resulting in poor sleep quality and excessive daytime sleepiness. Sleep apnea can be caused by a variety of factors, including obesity, alcohol consumption, and structural abnormalities in the airway. One of the key symptoms of sleep apnea is loud snoring, often accompanied by gasping or choking sounds. If left untreated, sleep apnea can have serious implications for both physical and mental health, including increased risk of heart disease, stroke, and depression. It is important to understand the definition, underlying causes, and potential treatments for sleep apnea in order to address this sleep disorder effectively.
Definition and Overview
Narcolepsy is a neurological disorder characterized by excessive daytime sleepiness (EDS) and uncontrollable sleep attacks. Individuals with narcolepsy have difficulty maintaining wakefulness and may experience sudden, overwhelming bouts of sleepiness throughout the day. These sleep attacks can occur during various activities, including work, school, or even while driving, severely impacting daily functioning. Along with EDS, narcolepsy is also associated with a range of other symptoms such as cataplexy, which is the sudden loss of muscle tone triggered by emotions. This can result in temporary muscle weakness or even collapse. Other symptoms may include sleep paralysis, where individuals are temporarily unable to move or speak when falling asleep or waking up, and hallucinations, often vivid and dream-like, occurring during the transition between sleep and wakefulness.
Narcolepsy is a chronic condition that usually begins in adolescence or early adulthood and persists throughout a person’s life. The exact cause of narcolepsy is not fully understood, but it is believed to involve a combination of genetic predisposition and environmental factors. Research has identified a link between narcolepsy and the neurotransmitter hypocretin, which plays a crucial role in regulating sleep-wake cycles. In individuals with narcolepsy, there is a deficiency of hypocretin in the brain, potentially contributing to the disrupted sleep patterns and excessive daytime sleepiness.
It is essential to note that narcolepsy is a distinct disorder separate from other sleep disorders like sleep apnea or insomnia. While it can be challenging to diagnose due to its overlap with other conditions, a comprehensive evaluation involving sleep studies, medical history, and physical examination is crucial for accurate diagnosis. Treatment options for narcolepsy typically involve a combination of medication, lifestyle adjustments, and support for managing symptoms. It is important for individuals with narcolepsy to seek timely diagnosis and appropriate treatment in order to address their sleep-related difficulties and improve their overall quality of life.
Causes and Symptoms
Narcolepsy Causes: The exact cause of narcolepsy is not fully understood. However, it is believed to be a combination of genetic and environmental factors. Some studies suggest that narcolepsy may be linked to a deficiency of a neurotransmitter called hypocretin, which plays a role in regulating wakefulness and sleep. Autoimmune factors may also contribute to the destruction of the brain cells that produce hypocretin. Other potential triggers include viral infections, hormonal changes, and certain medications. Research is ongoing to uncover the precise mechanisms responsible for narcolepsy development.
Narcolepsy Symptoms: The most common symptom of narcolepsy is excessive daytime sleepiness (EDS), characterized by overwhelming drowsiness and an irresistible urge to sleep during the day, regardless of how much sleep one gets at night. Individuals with narcolepsy may also experience sudden loss of muscle tone, known as cataplexy, triggered by strong emotions such as laughter, anger, or surprise. Other symptoms include sleep paralysis, wherein a person is temporarily unable to move or speak while waking up or falling asleep, and hallucinations, which can be vivid and dream-like. Additionally, some individuals with narcolepsy may experience disrupted nighttime sleep, frequent awakenings, and restless and fragmented sleep patterns.
Sleep Apnea Causes: Sleep apnea is primarily caused by a partial or complete obstruction of the airway during sleep, leading to interrupted breathing. This obstruction can be due to various factors, including excess weight, anatomical abnormalities, such as large tonsils or a narrow throat, and medical conditions like nasal congestion, sinus problems, or gastroesophageal reflux disease (GERD). Aging, smoking, and alcohol consumption can also contribute to the development of sleep apnea.
Sleep Apnea Symptoms: The hallmark symptom of sleep apnea is loud and chronic snoring, often accompanied by pauses in breathing. These pauses can last for several seconds and may be followed by gasping or choking sounds as the person briefly awakens to resume breathing. Other common symptoms include excessive daytime sleepiness, morning headaches, dry mouth or sore throat upon waking, difficulty concentrating, irritability, and decreased libido. Sleep apnea can also contribute to high blood pressure, heart problems, and increased risk of stroke if left untreated.
While narcolepsy and sleep apnea can both impact an individual’s sleep, their causes and symptoms are distinct. Narcolepsy is primarily believed to be influenced by genetic and environmental factors, potentially involving hypocretin deficiency or autoimmune factors. Its symptoms include excessive daytime sleepiness, cataplexy, sleep paralysis, and hallucinations. On the other hand, sleep apnea is caused by airway obstructions during sleep and is commonly marked by symptoms such as loud snoring, pauses in breathing, excessive daytime sleepiness, and increased risk of other health complications if left untreated.
Diagnosis and Treatment
Diagnosing narcolepsy involves a multi-faceted approach that includes a thorough evaluation of a person’s medical history, sleep patterns, and symptoms. A key diagnostic tool is a polysomnogram, which measures brain activity, eye movement, muscle activity, and heart rhythm during sleep. Additionally, a Multiple Sleep Latency Test (MSLT) is conducted to assess daytime sleepiness by measuring how quickly a person falls asleep in a sleep-encouraging environment. If a person has narcolepsy, they will often enter REM sleep much faster than usual during the MSLT.
Once diagnosed, treatment for narcolepsy typically involves a combination of medication and lifestyle modifications. Stimulant medications, such as modafinil or methylphenidate, can help improve wakefulness and reduce daytime sleepiness. Antidepressant medications may also be prescribed to manage symptoms of cataplexy and improve overall sleep quality. It is important for individuals with narcolepsy to establish healthy sleep hygiene practices, such as maintaining a regular sleep schedule and creating a conducive sleep environment.
Support from healthcare professionals, such as sleep specialists and therapists, can be instrumental in helping individuals cope with the challenges associated with narcolepsy. These professionals can provide guidance on managing symptoms, developing coping strategies, and addressing any emotional or psychological issues that may arise.
In contrast, the diagnosis of sleep apnea involves a comprehensive evaluation of symptoms, which may include loud snoring, gasping for air during sleep, and excessive daytime sleepiness. A sleep study, known as a polysomnogram, is typically conducted to measure breathing patterns, oxygen levels, and disruptions in sleep. The use of a portable monitor, known as a home sleep apnea test, may also be employed in some cases for a more convenient evaluation.
Treatment for sleep apnea primarily focuses on improving the individual’s breathing during sleep. The most common treatment option is Continuous Positive Airway Pressure (CPAP) therapy, which involves wearing a mask that delivers a continuous flow of air to keep the airways open. Other treatment options may include oral appliances, which help to reposition the jaw and tongue to prevent airway obstruction, and surgery in severe cases.
In addition to medical interventions, lifestyle changes can also be effective in managing sleep apnea. Maintaining a healthy weight through exercise and proper nutrition can reduce the severity of the condition. Avoiding alcohol, sedatives, and smoking is also recommended, as these substances can worsen symptoms. It is crucial for individuals with sleep apnea to prioritize regular sleep patterns and create a sleep-friendly environment, such as keeping the bedroom dark, quiet, and comfortable.
Support and education are important aspects of managing sleep apnea. Healthcare professionals can provide guidance on lifestyle modifications and assist with the proper use of CPAP machines or oral appliances. Additionally, support groups and online communities offer a space for individuals with sleep apnea to connect, share experiences, and gather information about treatment options and coping strategies.
Both narcolepsy and sleep apnea require an accurate diagnosis and an individualized treatment approach. While narcolepsy focuses on managing excessive daytime sleepiness and addressing symptoms like cataplexy, sleep apnea primarily targets improving breathing during sleep. Consulting with healthcare professionals, adhering to prescribed treatments, and implementing healthy lifestyle changes is essential for effectively managing these sleep disorders and enhancing overall well-being.
Key Differences

When comparing narcolepsy and sleep apnea, it is essential to recognize the key differences between these two sleep disorders. One significant distinction lies in the symptoms and manifestations experienced by individuals. In narcolepsy, excessive daytime sleepiness, sudden sleep attacks, and REM sleep abnormalities are prominent features. On the other hand, sleep apnea is characterized by disrupted breathing during sleep, resulting in loud snoring, gasping for air, and frequent awakenings. Another significant difference lies in the underlying mechanisms of these conditions. Narcolepsy is believed to be primarily caused by a deficiency in hypocretin, a neurotransmitter that regulates wakefulness, whereas sleep apnea is often the result of blocked or narrowed airways, leading to breathing disruptions. Additionally, these disorders can have different implications for physical health. Narcolepsy primarily affects daytime functioning and can increase the risk of accidents, while sleep apnea is associated with cardiovascular problems, high blood pressure, and other health complications. By understanding these key differences, individuals and healthcare professionals can effectively diagnose, treat, and manage each condition.
Symptoms and Manifestations
Narcolepsy and sleep apnea may both disrupt sleep patterns, but they exhibit distinct symptoms and manifestations. In the case of narcolepsy, excessive daytime sleepiness (EDS) is a prominent symptom, often accompanied by sudden and uncontrollable sleep attacks. These sleep attacks can occur at any time, regardless of the individual’s level of activity or the surrounding environment. Another hallmark symptom of narcolepsy is cataplexy, which involves a sudden loss of muscle tone triggered by intense emotions such as laughter, anger, or surprise. This can range from mild muscle weakness to complete paralysis and can significantly impact an individual’s quality of life. Other symptoms of narcolepsy include sleep paralysis, where an individual is unable to move or speak while falling asleep or waking up, hallucinations, and disrupted nighttime sleep with frequent awakenings. In contrast, sleep apnea is characterized by snoring, interrupted breathing during sleep, and recurrent awakenings due to breathing difficulties.
Underlying Mechanisms
Underlying Mechanisms between Narcolepsy and Sleep Apnea:
– Narcolepsy: The underlying mechanisms of narcolepsy involve a deficiency or dysfunction in the neurotransmitter hypocretin, which is responsible for regulating wakefulness and sleep. In the majority of cases, this deficiency is due to an autoimmune response that leads to the destruction of the hypocretin-producing cells in the brain. This autoimmune response is believed to be triggered by genetic factors and environmental triggers, although the exact cause is not well understood. The loss of hypocretin results in fragmented sleep patterns and the inability to maintain a consistent sleep-wake cycle.
– Sleep Apnea: Sleep apnea, on the other hand, is primarily caused by a physical obstruction of the airway during sleep, leading to repeated pauses in breathing. This obstruction can be the result of relaxed throat muscles or physical abnormalities in the airway structure. The most common form of sleep apnea, known as obstructive sleep apnea (OSA), occurs when the muscles in the back of the throat fail to keep the airway open, causing brief episodes of breathing cessation throughout the night. In central sleep apnea (CSA), the brain fails to send the proper signals to the muscles that control breathing. The disruption in airflow leads to fragmented sleep and decreased oxygen levels, triggering a cycle of shallow sleep and frequent awakenings.
It’s important to note that while the mechanisms of narcolepsy and sleep apnea differ, they can both disrupt the quality and quantity of sleep, resulting in daytime fatigue and other related symptoms. Understanding these underlying mechanisms is crucial in determining the appropriate treatments and management strategies for each condition.
Physical Health Implications
Narcolepsy and sleep apnea can both have significant implications for an individual’s physical health. However, the specific ways in which these conditions impact physical well-being differ. In narcolepsy, the excessive daytime sleepiness can lead to potential accidents and injuries due to sudden sleep attacks and impaired alertness. These episodes can occur at any time, making daily activities, such as driving or operating machinery, dangerous. Additionally, the fragmented sleep patterns and disrupted REM sleep in narcolepsy can contribute to difficulties in maintaining a healthy sleep schedule and obtaining restorative sleep.
On the other hand, sleep apnea primarily affects physical health through repeated disturbances in breathing during sleep. These interruptions in breathing can result in decreased oxygen saturation in the blood and lead to a range of health issues. Chronic sleep apnea has been linked to an increased risk of cardiovascular problems, including high blood pressure, heart disease, and stroke. The repetitive cycles of interrupted breathing can strain the cardiovascular system, causing changes in blood pressure and increasing the workload on the heart.
It is important to note that individuals with either narcolepsy or sleep apnea may also experience overlapping health implications. For instance, the chronic sleep deprivation associated with both conditions can lead to an increased risk of obesity, diabetes, and metabolic disorders. Additionally, the disruptive nature of these sleep disorders can negatively impact immune function, which may result in frequent infections and a compromised ability to fight off illnesses.
While both narcolepsy and sleep apnea have physical health implications, the specific consequences differ based on the nature of the sleep disturbance and its impact on the body’s physiological processes. Proactive management and treatment of these conditions are crucial in minimizing their potential adverse effects on physical health.
Narcolepsy and Heart Health: The Connection and Impact on the Cardiovascular System
Key Similarities
Both narcolepsy and sleep apnea share some key similarities in terms of the impact they have on sleep and the process of evaluating and diagnosing these conditions. One commonality is the presence of sleep disturbances. Individuals with both narcolepsy and sleep apnea often experience disrupted and fragmented sleep patterns, leading to excessive daytime sleepiness and a decrease in overall sleep quality. Another similarity lies in the evaluation and diagnosis process. In both cases, a comprehensive evaluation is necessary, which may include a sleep study, medical history review, and physical examination. Additionally, lifestyle modifications, such as weight management and healthy sleep practices, can benefit individuals with both conditions. While there are important differences between narcolepsy and sleep apnea, recognizing these shared aspects can help in understanding the challenges faced by individuals with these sleep disorders and guide towards effective management strategies.
Sleep Disturbances
Sleep disturbances are a common thread between narcolepsy and sleep apnea, albeit with distinctive features. In narcolepsy, the primary sleep disturbance is excessive daytime sleepiness. Individuals with narcolepsy have an overwhelming urge to sleep during the day, which can result in unintended napping episodes that interfere with daily activities. These daytime sleep attacks can occur in various settings, such as while at work, during meals, or even while engaging in conversations. On the other hand, sleep apnea manifests primarily as disrupted nighttime sleep. It is characterized by repeated pauses in breathing during sleep, known as apneas, causing individuals with sleep apnea to frequently wake up throughout the night, albeit often without full conscious awareness. These sleep disturbances can lead to excessive daytime sleepiness, morning headaches, and difficulty concentrating. Both narcolepsy and sleep apnea can severely impact an individual’s overall quality of sleep, leaving them feeling fatigued and unrefreshed during the day.
Evaluation and Diagnosis
Evaluation and diagnosis are crucial steps in identifying and differentiating between narcolepsy and sleep apnea. When it comes to narcolepsy, the diagnosis typically involves a thorough evaluation of the patient’s medical history, sleep patterns, and symptoms reported. Since narcolepsy is a chronic condition, it is essential to track the frequency and duration of excessive daytime sleepiness, as well as any episodes of sudden muscle weakness or paralysis (cataplexy). To confirm the diagnosis, a sleep study known as a polysomnography may be conducted, which involves monitoring brain waves, eye movements, muscle activity, and other physiological parameters during sleep. Additionally, a Multiple Sleep Latency Test (MSLT) may be performed to assess daytime sleepiness by measuring how quickly an individual falls asleep during specific nap opportunities. These diagnostic tests help healthcare professionals determine if an individual meets the criteria for narcolepsy and differentiate it from other sleep disorders.
On the other hand, when evaluating the possibility of sleep apnea, several factors are taken into consideration. A comprehensive assessment of the patient’s medical history, including symptoms such as snoring, gasping for air during sleep, and morning headaches, is conducted. Additionally, a physical examination may be performed to check for anatomical abnormalities, such as an enlarged tongue or tonsils, that can contribute to airway obstruction during sleep. Diagnostic tests such as a polysomnography or a home sleep apnea test are usually utilized to measure the frequency and severity of breathing interruptions during sleep. These tests monitor various parameters like oxygen levels, heart rate, and airflow to provide an accurate diagnosis of sleep apnea.
Both narcolepsy and sleep apnea require careful evaluation and diagnosis by healthcare professionals specializing in sleep medicine. These diagnostic assessments play a vital role in selecting appropriate treatment strategies and helping individuals manage their sleep disorders effectively.
Living with Narcolepsy
Living with narcolepsy can present significant challenges, but with proper coping strategies and support, it is possible to manage the condition and lead a fulfilling life. One key coping strategy is establishing a consistent sleep schedule, prioritizing regular sleep patterns, and ensuring an adequate amount of restful sleep each night. It can also be helpful to practice good sleep hygiene, such as creating a comfortable sleep environment, avoiding stimulants before bedtime, and implementing relaxation techniques to promote better sleep quality. Additionally, individuals with narcolepsy can benefit from developing strategies to manage excessive daytime sleepiness, such as taking scheduled naps throughout the day and incorporating physical activity into their routines. Support and resources, including narcolepsy support groups, therapy, and educational materials, can offer valuable guidance and a sense of community for individuals navigating the challenges of living with narcolepsy.
Coping Strategies
When it comes to coping with narcolepsy, individuals can employ various strategies to manage their symptoms and improve their quality of life. First and foremost, establishing a regular sleep schedule is essential. This includes maintaining a consistent sleep routine by going to bed and waking up at the same time each day. Creating a sleep-friendly environment can also contribute to better sleep hygiene, such as keeping the bedroom cool, dark, and quiet. Additionally, avoiding stimulating activities close to bedtime, like electronics or caffeine consumption, can help promote better sleep. Taking short, scheduled naps throughout the day can also be beneficial for managing excessive daytime sleepiness. It is important to prioritize self-care and engage in activities that promote relaxation and stress reduction, such as yoga, meditation, or deep breathing exercises. Seeking support from loved ones and joining support groups or online communities can provide a valuable network of individuals who understand the challenges of narcolepsy. Lastly, incorporating regular exercise into the daily routine can enhance overall well-being and promote better sleep quality. It is crucial to consult with a healthcare professional to develop a personalized coping strategy that suits individual needs and addresses specific symptoms.
Support and Resources
Finding the right support and resources is essential for individuals with narcolepsy or sleep apnea to effectively manage their condition and improve their quality of life. There are several avenues available to help individuals navigate the challenges and seek assistance. Support groups can be incredibly valuable, offering a sense of community and understanding among individuals who share similar experiences. These groups provide a platform for emotional support, sharing coping strategies, and exchanging information about the latest research and treatment options. Additionally, online forums and social media platforms dedicated to narcolepsy or sleep apnea offer a virtual space for individuals to connect, seek advice, and find support. It is important for individuals to take advantage of these resources, as they can provide validation, encouragement, and a wealth of knowledge. It is also advisable to consult healthcare professionals specializing in sleep disorders, such as sleep medicine specialists or sleep psychologists, who can provide tailored support and guidance. They can offer insights into treatment options, help individuals develop coping strategies, and address any concerns or questions that may arise. Additionally, they may recommend specific educational resources, such as books, websites, or articles, that provide comprehensive information about narcolepsy or sleep apnea. By availing themselves of the support and resources available, individuals can enhance their understanding of their condition, improve their overall well-being, and feel empowered to effectively manage their symptoms.
Living with Sleep Apnea
Living with sleep apnea can present various challenges and disruptions to daily life. Sleep apnea is a sleep disorder characterized by pauses in breathing during sleep, often resulting in loud snoring and fragmented sleep. These interruptions in breathing can lead to daytime fatigue, morning headaches, and difficulty concentrating. Coping with sleep apnea may involve implementing lifestyle changes, such as maintaining a healthy weight, avoiding alcohol and sedatives, and sleeping in a specific position that promotes better breathing. Continuous Positive Airway Pressure (CPAP) therapy is a common treatment option for sleep apnea, where a machine delivers a constant flow of air to keep the airways open during sleep. Adapting to wearing a CPAP mask during sleep and incorporating it into a nightly routine can enhance the quality of sleep and overall well-being for individuals with sleep apnea. Seeking support from healthcare professionals, joining support groups, and utilizing educational resources can also provide valuable assistance and encouragement on the journey of living with sleep apnea.
Coping Strategies
Living with narcolepsy or sleep apnea can be challenging, but there are various strategies that can help individuals manage their symptoms and improve their overall well-being. When it comes to coping with narcolepsy, establishing a consistent sleep schedule is paramount. Maintaining regular sleep and wake times can help regulate the body’s internal clock and improve sleep quality. Additionally, individuals with narcolepsy can benefit from scheduling short, strategic naps throughout the day to combat excessive sleepiness.
Incorporating healthy lifestyle habits can also make a significant difference. Eating a well-balanced diet, engaging in regular physical exercise, and avoiding excessive alcohol and caffeine consumption can promote better overall health and potentially alleviate symptoms. It is also crucial to create a sleep-friendly environment, including a comfortable bed, a dark and quiet room, and a relaxing bedtime routine.
Seeking support from family, friends, and healthcare professionals is vital for managing the emotional and psychological challenges that come with these sleep disorders. Support groups, therapy, and counseling can provide a safe space to share experiences, learn coping strategies, and receive validation from others who are going through similar journeys.
For individuals living with sleep apnea, the primary coping strategy is often the use of Continuous Positive Airway Pressure (CPAP) therapy. This therapy involves wearing a mask that delivers a constant flow of air to keep the airways open during sleep, thereby reducing episodes of obstructed breathing. Adhering to the prescribed CPAP therapy is key to managing sleep apnea and improving overall quality of sleep.
In addition to CPAP therapy, lifestyle changes such as weight loss, avoiding alcohol and sedatives, and sleeping in a side position can also be beneficial in alleviating sleep apnea symptoms. Regular exercise and practicing relaxation techniques, such as deep breathing or meditation, can help reduce stress and promote better sleep.
In both narcolepsy and sleep apnea, it is important for individuals to communicate openly with their healthcare providers and follow their recommended treatment plans. By working closely with healthcare professionals and implementing suitable coping strategies, individuals can effectively manage their symptoms and experience a better quality of life.
Support and Resources
Navigating life with a sleep disorder like narcolepsy or sleep apnea can be challenging, but there are numerous support and resources available to help individuals cope with their condition. Support groups provide a safe space for individuals to connect with others who are going through similar experiences. They offer a platform for sharing personal stories, exchanging coping strategies, and finding emotional support. These groups can be in-person or online, allowing individuals to connect regardless of their location. Additionally, organizations and foundations dedicated to sleep disorders provide valuable resources and information. They often have websites, educational materials, and helplines staffed by experts who can answer questions and offer guidance. Healthcare professionals such as sleep specialists, psychologists, and therapists are also vital resources for managing the emotional and psychological aspects of living with a sleep disorder. They can provide individualized treatment plans, therapy sessions, and medication management options. It’s important for individuals to explore these support and resource options to build a strong network of assistance and receive the necessary guidance and understanding in their journey towards better sleep health.
Conclusion
In conclusion, narcolepsy and sleep apnea are two distinct sleep disorders that share certain similarities but also have significant differences. While both conditions can lead to sleep disturbances and have an impact on a person’s daily life, narcolepsy is characterized by excessive daytime sleepiness, sudden sleep attacks, and REM sleep symptoms during wakefulness, whereas sleep apnea is primarily marked by episodes of interrupted breathing during sleep. The underlying mechanisms and physical health implications also differ, as narcolepsy is a neurological disorder affecting the brain’s sleep-wake cycles, while sleep apnea is often related to obstruction of the airway during sleep. Understanding these differences is crucial for accurate diagnosis and appropriate treatment. Coping with these conditions involves specific strategies tailored to each disorder, such as lifestyle modifications, medication, and the use of medical devices in the case of sleep apnea. Support and resources are available for individuals living with narcolepsy or sleep apnea, offering guidance, education, and a community of understanding. By seeking proper diagnosis and adopting effective coping strategies, individuals can find ways to manage their symptoms and improve their quality of life.
Frequently Asked Questions
What are the primary symptoms of narcolepsy?
The primary symptoms of narcolepsy include excessive daytime sleepiness, sudden sleep attacks, hypnagogic hallucinations, sleep paralysis, and cataplexy.
How is narcolepsy diagnosed?
Narcolepsy is diagnosed through a combination of medical history, physical examination, sleep studies, and specific tests like a Multiple Sleep Latency Test (MSLT) and a Polysomnography (PSG).
What causes narcolepsy?
The exact cause of narcolepsy is still unknown, but it is believed to involve genetic factors and an autoimmune response that affects the production of a neurotransmitter called hypocretin.
Can narcolepsy occur in children?
Yes, narcolepsy can occur in children, although it is less common. The symptoms may differ slightly from those in adults, and it can often be misdiagnosed as other conditions.
What is cataplexy?
Cataplexy is a sudden loss of muscle control triggered by strong emotions, such as laughter, anger, or surprise. It is a unique symptom of narcolepsy and can range from subtle weakness to complete collapse.
Is there a cure for narcolepsy?
Currently, there is no cure for narcolepsy. However, treatments such as medication, lifestyle changes, and support strategies can help manage the symptoms and improve quality of life.
Can narcolepsy be dangerous?
Narcolepsy itself is not life-threatening. However, the excessive daytime sleepiness and sudden sleep attacks can pose risks, especially when operating machinery or driving. It is essential to manage the condition effectively to minimize potential dangers.
What is the connection between narcolepsy and mental health?
Narcolepsy can have a significant impact on mental health, as individuals may experience depression, anxiety, and mood disturbances due to the challenges of managing the condition and coping with excessive daytime sleepiness.
Are there any support groups for people with narcolepsy?
Yes, there are numerous support groups, online communities, and advocacy organizations dedicated to providing support, education, and resources for individuals with narcolepsy and their families. Connecting with these groups can offer valuable guidance and a sense of belonging.
Can lifestyle changes help manage narcolepsy?
Yes, lifestyle changes such as maintaining a regular sleep schedule, incorporating scheduled naps, avoiding stimulants, and practicing good sleep hygiene can complement medical treatments and help manage narcolepsy symptoms more effectively.